Metoidioplasty
| Part of a series on |
| Transgender topics |
|---|
|
|

Metoidioplasty, metaoidioplasty, or metaidoioplasty[2] (informally called a meto or meta) is a female-to-male sex reassignment surgery.[3]
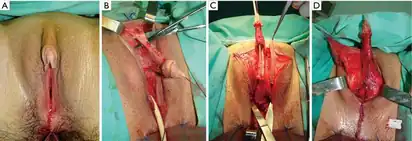
Testosterone replacement therapy gradually enlarges the clitoris to a mean maximum size of 4.6 cm (1.6–2 in)[4] (as the clitoris and the penis are developmentally homologous). In a metoidioplasty, the urethral plate and urethra are completely dissected from the clitoral corporeal bodies, then divided at the distal end, and the testosterone-enlarged clitoris straightened out and elongated. A longitudinal vascularized island flap is configured and harvested from the dorsal skin of the clitoris, reversed to the ventral side, tubularized and an anastomosis is formed with the native urethra. The new urethral meatus is placed along the neophallus to the distal end and the skin of the neophallus and scrotum reconstructed using labia minora and majora flaps.[5] The new neophallus ranges in size from 4–10 cm (with an average of 5.7 cm) and has the approximate girth of a human adult thumb.[6]
The term derives from meta- "change," Ancient Greek αἰδοῖον (aidoion) "genitals," and -plasty, denoting surgical construction or modification.[2]
Comparison with phalloplasty
Metoidioplasty is technically simpler than phalloplasty, costs less, and has fewer potential complications. However, phalloplasty patients are far more likely to be capable of sexual penetration (mainly due to size constraints) after they recover from surgery.[7]
In a phalloplasty, the surgeon fabricates a neopenis by grafting tissue from a donor site (such as from the patient's back, arm or leg). A phalloplasty takes about 8–10 hours to complete (the first stage), and is generally followed by multiple (up to 3) additional surgical procedures including glansplasty, scrotoplasty, testicular prosthesis, and/or penile implant.
Metoidioplasty typically requires 2–3 hours to complete. Because the clitoris' erectile tissue functions normally, a prosthesis is unnecessary for erection (although the clitoris might not become as rigid as a penile erection). In nearly all cases, metoidioplasty patients can continue to have clitoral orgasms after surgery.
Note also, that the two alternative techniques are not mutually exclusive and phalloplasty extension of a metioidiplasic base neophallus is possible.[8]
Operation

Alternative techniques
Recent studies have introduced an operative technique known as Extensive Metoidioplasty. This method extensively detaches the clitoris, nearly completely detaching it from the pubic arch before its reattachment and elongation. Current studies show this method yielding penile lengths of 6-12 centimeters, with 7/10 patients being capable of obtaining erections capable of penetrative intercourse.[10]
Complications
Complications from Metoidioplasty vary in severity. Minor complications may be resolved through minor supportive care, while more serious complications may require surgical correction. As with other surgical procedures, metoidioplasty has the possibility to cause infection, bleeding, blood clots, damage to surrounding tissues, pain, as well as negative reactions to anesthesia or other required medications.
If urethral lengthening is performed, urethral complications such as urinary fistula may occur.[11] Patients who experience postvoid incontinence or dribbling following surgery report their symptoms as resolved within three months.[12]
Satisfaction rates among patients who undergo Metoidioplasty are generally very high regarding both appearance and sexual satisfaction.[12][13]
See also
- List of transgender-related topics
- Phalloplasty
References
- ↑ Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML (2021-10-13). "Metoidioplasty: Surgical Options and Outcomes in 813 Cases". Frontiers in Endocrinology. 12: 760284. doi:10.3389/fendo.2021.760284. PMC 8548780. PMID 34721306.
- 1 2 Hage JJ (January 1996). "Metaidoioplasty: an alternative phalloplasty technique in transsexuals". Plastic and Reconstructive Surgery. 97 (1): 161–167. doi:10.1097/00006534-199601000-00026. PMID 8532774. S2CID 38412526.
- ↑ Perovic SV, Djordjevic ML (December 2003). "Metoidioplasty: a variant of phalloplasty in female transsexuals". BJU International. 92 (9): 981–5. doi:10.1111/j.1464-410x.2003.04524.x. PMID 14632860. S2CID 11836091.
- ↑ Meyer WJ, Webb A, Stuart CA, Finkelstein JW, Lawrence B, Walker PA (April 1986). "Physical and hormonal evaluation of transsexual patients: a longitudinal study". Archives of Sexual Behavior. 15 (2): 121–38. doi:10.1007/BF01542220. PMID 3013122. S2CID 42786642.
- ↑ Perovic, S. and Djordjevic, M. (2003), Metoidioplasty: a variant of phalloplasty in female transsexuals. BJU International, 92: 981-985. doi:10.1111/j.1464-410X.2003.04524.x
- ↑ Djordjevic ML, Stanojevic D, Bizic M, Kojovic V, Majstorovic M, Vujovic S, Milosevic A, Korac G, Perovic SV (May 2009). "Metoidioplasty as a single stage sex reassignment surgery in female transsexuals: Belgrade experience". The Journal of Sexual Medicine. 6 (5): 1306–13. doi:10.1111/j.1743-6109.2008.01065.x. PMID 19175859.
- ↑ Frey JD, Poudrier G, Chiodo MV, Hazen A (December 2016). "A Systematic Review of Metoidioplasty and Radial Forearm Flap Phalloplasty in Female-to-male Transgender Genital Reconstruction: Is the "Ideal" Neophallus an Achievable Goal?". Plastic and Reconstructive Surgery. Global Open. 4 (12): e1131. doi:10.1097/GOX.0000000000001131. PMC 5222645. PMID 28293500.
- ↑ Al-Tamimi M, Pigot GL, van der Sluis WB, van de Grift TC, van Moorselaar RJ, Mullender MG, et al. (November 2019). "The Surgical Techniques and Outcomes of Secondary Phalloplasty After Metoidioplasty in Transgender Men: An International, Multi-Center Case Series". The Journal of Sexual Medicine. 16 (11): 1849–1859. doi:10.1016/j.jsxm.2019.07.027. PMID 31542350. S2CID 202731384.
- 1 2 Djordjevic ML, Stojanovic B, Bizic M (June 2019). "Metoidioplasty: techniques and outcomes". Translational Andrology and Urology. 8 (3): 248–253. doi:10.21037/tau.2019.06.12. PMC 6626308. PMID 31380231.
- ↑ Cohanzad S (February 2016). "Extensive Metoidioplasty as a Technique Capable of Creating a Compatible Analogue to a Natural Penis in Female Transsexuals". Aesthetic Plastic Surgery. 40 (1): 130–8. doi:10.1007/s00266-015-0607-4. PMID 26744289. S2CID 40551674.
- ↑ "Metoidioplasty Risks and Complications: Is Metoidioplasty Really Worth It?". Trans Media Network.
- 1 2 Vukadinovic V, Stojanovic B, Majstorovic M, Milosevic A (2014). "The role of clitoral anatomy in female to male sex reassignment surgery". TheScientificWorldJournal. 2014: 437378. doi:10.1155/2014/437378. PMC 4005052. PMID 24982953.
- ↑ De Cuypere G, TSjoen G, Beerten R, Selvaggi G, De Sutter P, Hoebeke P, et al. (December 2005). "Sexual and physical health after sex reassignment surgery". Archives of Sexual Behavior. 34 (6): 679–90. doi:10.1007/s10508-005-7926-5. PMID 16362252. S2CID 42916543.
Further reading
- Greenwald D, Stadelmann W (July 2001). "Gender reassignment". EMedicine Journal. 2 (7).