Neonatal acne
| Neonatal acne | |
|---|---|
| Other names: Acne infantum, acne neonatorum,[1] | |
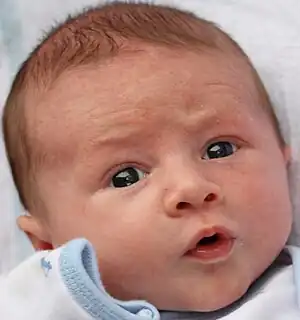 | |
| An infant with neonatal acne on the face | |
| Specialty | Dermatology |
| Symptoms | Open and closed comedones on the cheeks, chin and forehead |
| Usual onset | Birth to 6 weeks |
| Duration | 4 to 12 weeks |
| Causes | Androgens; Malassezia yeast |
| Differential diagnosis | Erythema toxicum neonatorum, neonatal cephalic pustulosis, transient neonatal pustular melanosis, folliculitis, miliaria, milia |
| Prognosis | Often mild and self-resolving |
| Frequency | 20% of newborns under 6 weeks |
Neonatal acne is a type of acne that occurs in a newborn baby.[2] It typically presents with a few small bumps, some of which may contain yellow fluid, on the face of a baby.[2] There may also be open and closed comedones on the cheeks, chin, and forehead.[3]
The cause is not entirely known. The underlying mechanism may involves elevated androgens, which are transferred from the mother to the newborn via the placenta and produced endogenously by the fetal adrenal gland and neonatal testicles. These androgens are thought to stimulate sebaceous glands to increase sebum production, causing comedone formation.[3][4] An inflammatory reaction to the yeast Malassezia Furfur may also be involved.[3]
Neonatal acne is typically mild and self-limited and rarely requires treatment.[3] Persistent or severe cases may warrant therapy with topical benzoyl peroxide, topical retinoids, topical antibiotics, and topical antifungals.[5][6]
Neonatal acne occurs in 20% of newborns, and is more common in males than females by a ratio of 5:1.
Signs and Symptoms
Neonatal acne presents from birth to the first 4-6 weeks of life.[7][4] Common symptoms are open and closed comedones such as papules and pustules that occur most commonly on the face on the areas of the cheeks, chin and forehead.[3] Less commonly, lesions can be present on the chest and back.[6]
.jpg.webp) Neonatal acne
Neonatal acne.jpg.webp) Neonatal cephalic pustulosis
Neonatal cephalic pustulosis
Causes
The etiology of neonatal acne is not entirely known. It is thought that maternal androgens transferred to the infant through the placenta stimulate sebaceous glands leading to increased sebum production and comedone formation.[3][4] Dehydroepiandrosterone (DHEA) produced from the fetal adrenal gland and androgen production from neonatal testicles may also stimulate sebum production from sebaceous glands.[6][4]
The role of genetics is unclear but a positive family history supports association with neonatal acne.[7]
Some researchers suggest that neonatal acne represents a hypersensitivity reaction to skin colonization by commensal yeast Malassezia, although this tends to be linked more frequently to neonatal cephalic pustulosis.[3]
Diagnosis
Further workup is suggested in cases of severe acneiform eruptions, sexual precocity, virilization or growth abnormalities to rule out potential endocrine diseases, tumor formation, or gonadal development abnormalities.[8] A referral to a pediatric endocrinologist may be warranted.[9]
Differential diagnosis
Other causes of acneiform eruptions such as those induced by the use of topical products like creams, ointments and shampoos on the skin are often ruled out before diagnosis.[6] Maternal medications like lithium and high dose corticosteroids may also induce formulation of pustules in newborns and can be assessed with a thorough family history.[7] Likewise, newborns can be assessed for infection whether bacterial, fungal or viral in nature. Erythema toxicum neonatorum, neonatal cephalic pustulosis, transient neonatal pustular melanosis, folliculitis, miliaria and milia are often ruled out before diagnosis.[3][6]
Some experts consider neonatal cephalic pustulosis (NCP) a form of neonatal acne while others do not.[4] NCP presents with facial papules and pustules but no comedones. NCP has been linked to Malassezia colonization, a normal yeast found on skin, but inconsistent patterns of positive colonization and NCP suggests that Malassezia hypersensitivity reactions in susceptible newborns are the cause of the acneiform eruptions rather than colonization itself.[4][7]
Treatment
Neonatal acne will typically self-resolves over 2-6 months and rarely requires treatment[3]. In mild cases, cleansing the face daily with gentle soap and water while avoiding use of potential comedogenic soaps, lotions and oils is often sufficient. Further treatment is not necessary, but topical therapy can be initiated in severe or persistent cases.[6]
Benzoyl peroxide
Topical benzoyl peroxide (BPO) may be indicated in persistent or inflammatory cases.[6] BPO is a lipophilic agent that penetrates into sebaceous glands and generates reactive oxygen species that kill P. acnes.[5] It also has comedolytic and anti-inflammatory properties and can prevent development of antimicrobial resistance.[10]
Topical retinoids
Topical retinoids can be used alone or in combination with BPO. Retinoids are derived from vitamin A. They bind to retinoic receptors to normalize the rate of keratinocyte growth and prevent inflammation.[8][11] Overactive keratinocyte production can lead to comedone formation.[12]
Topical antibiotics
In cases where scarring is a concern, topical antibiotics may be recommended.[5] Topical clindamycin and erythromycin are the most commonly prescribed options for acne. Antibiotics kill P. acnes on skin that could be causing inflammation.[12] With the emergence of resistant P. acnes, experts recommend topical antibiotics to be used in combination with BPO to reduce the risk of development of antimicrobial resistance.[5] The most common side effects of topical antibiotics are stinging, burning and redness at the site of application.[4]
Topical antifungals
Some experts suggest the use of topical ketoconazole in newborns with more pustular neonatal acne as there is evidence it shortens lesions duration.[4] This may be in cases more suggestive of neonatal cephalic pustulosis than neonatal acne.[6]
Epidemiology
Neonatal acne occurs in 20% of newborns. However, there has been debate regarding whether this accurately represents the true prevalence, as controversy exists as to whether neonatal acne is distinct from non-comedone forming acneiform disorders, such as neonatal cephalic pustulosis.[11] Neonatal acne occurs more often in boys than girls by a ratio of 5:1. This is because males tend to have higher circulating androgen levels due to androgen production in both the adrenal glands and testes, while female androgens are produced only in the adrenal glands.[3]
See also
References
- ↑ Holm EA, Jemec GB (December 2000). "[Acne neonatorum/acne infantum]". Ugeskrift for Læger (in dansk). 162 (50): 6856–7. PMID 11187144.
- 1 2 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "13. Acne". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Elsevier. pp. 231–251. ISBN 978-0-323-54753-6. Archived from the original on 2023-06-30. Retrieved 2023-07-20.
- 1 2 3 4 5 6 7 8 9 10 Greydanus, Donald E.; Azmeh, Roua; Cabral, Maria Demma; Dickson, Cheryl A.; Patel, Dilip R. (2021-04-01). "Acne in the first three decades of life: An update of a disorder with profound implications for all decades of life". Disease-a-Month. 67 (4): 101103. doi:10.1016/j.disamonth.2020.101103. ISSN 0011-5029. PMID 33041056. Archived from the original on 2021-04-18. Retrieved 2021-05-12.
- 1 2 3 4 5 6 7 8 Maroñas-Jiménez, L.; Krakowski, A. C. (2016-04-01). "Pediatric Acne: Clinical Patterns and Pearls". Dermatologic Clinics. 34 (2): 195–202. doi:10.1016/j.det.2015.11.006. ISSN 0733-8635. PMID 27015779. Archived from the original on 2021-04-23. Retrieved 2021-05-12.
- 1 2 3 4 Gamble, Ryan; Dunn, Jeff; Dawson, Annelise; Petersen, Brian; McLaughlin, Lauren; Small, Alison; Kindle, Scott; Dellavalle, Robert P. (June 2012). "Topical Antimicrobial Treatment of Acne Vulgaris: An Evidence-Based Review". American Journal of Clinical Dermatology. 13 (3): 141–152. doi:10.2165/11597880-000000000-00000. ISSN 1175-0561. PMID 22268388. S2CID 5838346. Archived from the original on 2021-08-28. Retrieved 2021-05-12.
- 1 2 3 4 5 6 7 8 Chernoff, Karen A.; Zaenglein, Andrea L. (2017), Teng, Joyce M.C.; Marqueling, Ann L.; Benjamin, Latanya T. (eds.), "Disorders of the Sebaceous and Sweat Gland", Therapy in Pediatric Dermatology, Cham: Springer International Publishing, pp. 113–122, doi:10.1007/978-3-319-43630-2_8, ISBN 978-3-319-43628-9, archived from the original on 2021-08-28, retrieved 2021-04-19
- 1 2 3 4 Herane, Maria Isabel (2014), Zouboulis, Christos C.; Katsambas, Andreas D.; Kligman, Albert M. (eds.), "Childhood Acne", Pathogenesis and Treatment of Acne and Rosacea, Berlin, Heidelberg: Springer Berlin Heidelberg, pp. 227–234, doi:10.1007/978-3-540-69375-8_30, ISBN 978-3-540-69374-1, archived from the original on 2021-08-28, retrieved 2021-04-19
- 1 2 Zeichner, Joshua, ed. (2014). Acneiform Eruptions in Dermatology: A Differential Diagnosis. New York, NY: Springer New York. doi:10.1007/978-1-4614-8344-1. ISBN 978-1-4614-8343-4. Archived from the original on 2021-08-28. Retrieved 2021-05-12.
- ↑ Baldwin, Hilary (2014), Zeichner, Joshua (ed.), "Neonatal and Infantile Acne", Acneiform Eruptions in Dermatology: A Differential Diagnosis, New York, NY: Springer, pp. 371–374, doi:10.1007/978-1-4614-8344-1_51, ISBN 978-1-4614-8344-1, archived from the original on 2021-08-28, retrieved 2021-04-20
- ↑ Eichenfield, L. F.; Krakowski, A. C.; Piggott, C.; Del Rosso, J.; Baldwin, H.; Friedlander, S. F.; Levy, M.; Lucky, A.; Mancini, A. J.; Orlow, S. J.; Yan, A. C. (2013-05-01). "Evidence-Based Recommendations for the Diagnosis and Treatment of Pediatric Acne". Pediatrics. 131 (Supplement): S163–S186. doi:10.1542/peds.2013-0490B. ISSN 0031-4005. PMID 23637225. S2CID 2277620. Archived from the original on 2021-08-28. Retrieved 2021-05-12.
- 1 2 Ashton, Rosalind; Weinstein, Miriam (November 2019). "Acne Vulgaris in the Pediatric Patient". Pediatrics in Review. 40 (11): 577–589. doi:10.1542/pir.2018-0137. ISSN 0191-9601. PMID 31676531. S2CID 207834296. Archived from the original on 2021-08-28. Retrieved 2021-05-12.
- 1 2 Zeichner, Joshua, ed. (2014). Acneiform Eruptions in Dermatology: A Differential Diagnosis. New York, NY: Springer New York. doi:10.1007/978-1-4614-8344-1. ISBN 978-1-4614-8343-4. Archived from the original on 2021-08-28. Retrieved 2021-05-12.
Further reading
- Katsambas AD, Katoulis AC, Stavropoulos P (February 1999). "Acne neonatorum: a study of 22 cases". Int. J. Dermatol. 38 (2): 128–30. doi:10.1046/j.1365-4362.1999.00638.x. PMID 10192162.
- O'Connor NR, McLaughlin MR, Ham P (January 2008). "Newborn skin: Part I. Common rashes". Am Fam Physician. 77 (1): 47–52. PMID 18236822. Archived from the original on 2017-03-29. Retrieved 2021-05-12.