Repolarization
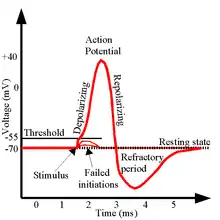
In neuroscience, repolarization refers to the change in membrane potential that returns it to a negative value just after the depolarization phase of an action potential which has changed the membrane potential to a positive value. The repolarization phase usually returns the membrane potential back to the resting membrane potential. The efflux of potassium (K+) ions results in the falling phase of an action potential. The ions pass through the selectivity filter of the K+ channel pore.
Repolarization typically results from the movement of positively charged K+ ions out of the cell. The repolarization phase of an action potential initially results in hyperpolarization, attainment of a membrane potential, termed the afterhyperpolarization, that is more negative than the resting potential. Repolarization usually takes several milliseconds.[1]
Repolarization is a stage of an action potential in which the cell experiences a decrease of voltage due to the efflux of potassium (K+) ions along its electrochemical gradient. This phase occurs after the cell reaches its highest voltage from depolarization. After repolarization, the cell hyperpolarizes as it reaches resting membrane potential (−70 mV){in neuron −70 mV}. Sodium (Na+) and potassium ions inside and outside the cell are moved by a sodium potassium pump, ensuring that electrochemical equilibrium remains unreached to allow the cell to maintain a state of resting membrane potential.[2] In the graph of an action potential, the hyper-polarization section looks like a downward dip that goes lower than the line of resting membrane potential. In this afterhyperpolarization (the downward dip), the cell sits at more negative potential than rest (about −80 mV) due to the slow inactivation of voltage gated K+ delayed rectifier channels, which are the primary K+ channels associated with repolarization.[3] At these low voltages, all of the voltage gated K+ channels close, and the cell returns to resting potential within a few milliseconds. A cell which is experiencing repolarization is said to be in its absolute refractory period. Other voltage gated K+ channels which contribute to repolarization include A-type channels and Ca2+-activated K+ channels.[4] Protein transport molecules are responsible for Na+ out of the cell and K+ into the cell to restore the original resting ion concentrations.[5]
Deviations from normal repolarization
Blockages in repolarization can arise due to modifications of the voltage-gated K+ channels. This is demonstrated with selectively blocking voltage gated K+ channels with the antagonist tetraethylammonium (TEA). By blocking the channel, repolarization is effectively stopped.[6] Dendrotoxins are another example of a selective pharmacological blocker for voltage gated K+ channels. The lack of repolarization means that neuron stays at a high voltage, which slows sodium channel deinactivation to a point where there is not enough inwards Na+ current to depolarize and sustain firing.[7]
Voltage gated K+ mechanisms
The structure of the voltage gated K+ channel is that of six transmembrane helices along the lipid bilayer. The selectivity of this channel to voltage is mediated by four of these transmembrane domains (S1–S4) – the voltage sensing domain. The other two domains (S5, S6) form the pore by which ions traverse.[8] Activation and deactivation of the voltage gated K+ channel is triggered by conformational changes in the voltage sensing domain. Specifically, the S4 domain moves such that it activates and deactivates the pore. During activation, there is outward S4 motion, causing tighter VSD-pore linkage. Deactivation is characterized by inward S4 motion.[9]
The switch from depolarization into repolarization is dependent on the kinetic mechanisms of both voltage gated K+ and Na+ channels. Although both voltage gated Na+ and K+ channels activate at roughly the same voltage (−50 mV), Na+ channels have faster kinetics and activate/deinactivate much more quickly.[10] Repolarization occurs as the influx of Na+ decreases (channels deinactivate) and the efflux of K+ ions increases as its channels open.[11] The decreased conductance of sodium ions and increased conductance of potassium ions cause the cell's membrane potential to very quickly return to, and past the resting membrane potential, which causes the hyperpolarization due to the potassium channels closing slowly, allowing more potassium to flow through after the resting membrane potential has been reached.[10]
Type of K+ channels in repolarization
Following the action potential, characteristically generated by the influx of Na+ through voltage gated Na+ channels, there is a period of repolarization in which the Na+ channels are inactivated while K+ channels are activated. Further study of K+ channels shows that there are four types which influence the repolarization of the cell membrane to re-establish the resting potential. The four types are Kv1, Kv2, Kv3 and Kv4. The Kv1 channel primarily influences the repolarization of the axon. The Kv2 channel is characteristically activated slower. The Kv4 channels are characteristically activated rapidly. When Kv2 and Kv4 channels are blocked, the action potential predictably widens.[12] The Kv3 channels open at a more positive membrane potential and deactivate 10 times faster than the other Kv channels. These properties allow for the high-frequency firing that mammalian neurons require. Areas with dense Kv3 channels include the neocortex, basal ganglia, brain stem and hippocampus as these regions create microsecond action potentials that requires quick repolarization.[13]
Utilizing voltage-clamp data from experiments based on rodent neurons, the Kv4 channels are associated with the primary repolarization conductance following the depolarization period of a neuron. When the Kv4 channel is blocked, the action potential becomes broader, resulting in an extended repolarization period, delaying the neuron from being able to fire again. The rate of repolarization closely regulates the amount of Ca2+ ions entering the cell. When large quantities of Ca2+ ions enter the cell due to extended repolarization periods, the neuron may die, leading to the development of stroke or seizures.[12]
The Kv1 channels are found to contribute to repolarization of pyramidal neurons, likely associated with an upregulation of the Kv4 channels. The Kv2 channels were not found to contribute to repolarization rate as blocking these channels did not result in changes in neuron repolarization rates.[12]
Repolarization of atria cells
Another type of K+ channel that helps to mediate repolarization in the human atria is the SK channel, which are K+ channels which are activated by increases in Ca2+ concentration. "SK channel" stands for a small conductance calcium activated potassium channel, and the channels are found in the heart. SK channels specifically act in the right atrium of the heart, and have not been found to be functionally important in the ventricles of the human heart. The channels are active during repolarization as well as during the atrial diastole phase when the current undergoes hyperpolarization.[14] Specifically, these channels are activated when Ca2+ binds to calmodulin (CaM) because the N-lobe of CaM interacts with the channel's S4/S5 linker to induce conformational change.[15] When these K+ channels are activated, the K+ ions rush out of the cell during the peak of its action potential causing the cell to repolarize as the influx of Ca2+ ions are exceeded by K+ ions leaving the cell continuously.[16]
Ventricular repolarization
In the human ventricles, repolarization can be seen on an ECG (electrocardiogram) via the J-wave (Osborn), ST segment, T wave and U wave. Due to the complexity of the heart, specifically how it contains three layers of cells (endocardium, myocardium and epicardium), there are many physiological changes effecting repolarization that will also affect these waves.[17] Apart from changes in the structure of the heart that effect repolarization, there are many pharmaceuticals that have the same effect.
On top of that, repolarization is also altered based on the location and duration of the initial action potential. In action potentials stimulated on the epicardium, it was found that the duration of the action potential needed to be 40–60 msec to give a normal, upright T-wave, whereas a duration of 20–40 msec would give an isoelectric wave and anything under 20 msec would result in a negative T-wave.[18]
Early repolarization is a phenomenon that can be seen in ECG recordings of ventricular cells where there is an elevated ST segment, also known as a J wave. The J wave is prominent when there is a larger outward current in the epicardium compared to the endocardium.[19] It has been historically considered to be a normal variant in cardiac rhythm but recent studies show that it is related to an increased risk of cardiac arrest. Early repolarization occurs mainly in males and is associated with a larger potassium current caused by the hormone testosterone. Additionally, although the risk is unknown, African American individuals seem more likely to have the early repolarization more often.[20]
Early repolarization syndrome
As mentioned in the previous section, early repolarization is known as appearing as elevated wave segments on ECGs. Recent studies have shown a connection between early repolarization and sudden cardiac death, which is identified as early repolarization syndrome. The condition is shown in both ventricular fibrillation without other structural heart defects as well as an early depolarization pattern, which can be seen on ECG.[21]
The primary root of early repolarization syndrome stems from malfunctions of electrical conductance in ion channels, which may be due to genetic factors. Malfunctions of the syndrome include fluctuating sodium, potassium, and calcium currents. Changes in these currents may result in overlap of myocardial regions undergoing different phases of the action potential simultaneously, leading to risk of ventricular fibrillation and arrhythmias.[22]
Upon being diagnosed, most individuals do not need immediate intervention, as early repolarization on an ECG does not indicate any life-threatening medical emergency.[23] Three to thirteen percent of healthy individuals have been observed to have early repolarization on an ECG.[21] However, patients who display early repolarization after surviving an event of early repolarization syndrome (a sudden-cardiac death experience), an implantable cardioverter-defibrillator (ICD) is strongly recommended.[23] In addition, a patient may be more prone to atrial fibrillation if the individual has early repolarization syndrome and is under sixty years of age.[21]
Impaired cardiac repolarization with obstructive sleep apnea
Patients who suffer from obstructive sleep apnea can experience impaired cardiac repolarization, increasing the morbidity and mortality of the condition greatly. Especially at higher altitudes, patients are much more susceptible to repolarization disturbances. This can be somewhat mitigated through the use of medications such as acetazolamide, but the drugs do not provide sufficient protection. Acetazolamide and similar drugs are known to be able to improve the oxygenation and sleep apnea for patients in higher altitudes, but the benefits of the drug have been observed only when traveling at altitudes temporarily, not for people who remain at a higher altitude for a longer time.[24]
References
- ↑ Hardin J, Bertoni GP, Kleinsmith LJ (December 2010). Becker's World of the Cell. Benjamin-Cummings Publishing Company. p. 389. ISBN 978-0-321-71602-6.
- ↑ Chrysafides SM, Sharma S (2019). Physiology, Resting Potential. StatPearls. StatPearls Publishing. PMID 30855922.
- ↑ Lentz TL, Erulkar SD (2018). "Nervous System". Encyclopædia Britannica.
- ↑ Purves D, Augustine GJ, Fitzpatrick D, Katz LC, LaMantia AS, McNamara JO, Williams SM, eds. (2001). Neuroscience (2nd ed.). Sunderland, Mass: Sinauer Assoc. ISBN 0-87893-742-0.
- ↑ "Action Potential". Britannica Academic. Encyclopædia Britannica, Inc. Retrieved 2019-09-26.
- ↑ Whishaw IQ, Kolb B (2015). Fundamentals of Human Neuropsychology. New York, NY: Worth Publishers.
- ↑ Hirokawa N, Windhorst U (2008). "Depolarization Block". Encyclopedia of Neuroscience. pp. 943–944. doi:10.1007/978-3-540-29678-2_1453. ISBN 978-3-540-23735-8.
- ↑ Kuang Q, Purhonen P, Hebert H (October 2015). "Structure of potassium channels". Cellular and Molecular Life Sciences. 72 (19): 3677–93. doi:10.1007/s00018-015-1948-5. PMC 4565861. PMID 26070303.
- ↑ Jensen MØ, Jogini V, Borhani DW, Leffler AE, Dror RO, Shaw DE (April 2012). "Mechanism of voltage gating in potassium channels". Science. 336 (6078): 229–33. Bibcode:2012Sci...336..229J. doi:10.1126/science.1216533. PMID 22499946. S2CID 2340286.
- 1 2 Byrn JH. "Chapter Two: Ionic Mechanisms and Action Potentials". Neuroscience Online. University of Texas Medical School.
- ↑ Striedter GF (2016). Neurobiology: A Functional Approach. New York, NY: Oxford University Press.
- 1 2 3 Pathak D, Guan D, Foehring RC (May 2016). "Roles of specific Kv channel types in repolarization of the action potential in genetically identified subclasses of pyramidal neurons in mouse neocortex". Journal of Neurophysiology. 115 (5): 2317–29. doi:10.1152/jn.01028.2015. PMC 4922457. PMID 26864770.
- ↑ Kaczmarek LK, Zhang Y (October 2017). "Kv3 Channels: Enablers of Rapid Firing, Neurotransmitter Release, and Neuronal Endurance". Physiological Reviews. 97 (4): 1431–1468. doi:10.1152/physrev.00002.2017. PMC 6151494. PMID 28904001.
- ↑ Skibsbye L, Poulet C, Diness JG, Bentzen BH, Yuan L, Kappert U, et al. (July 2014). "Small-conductance calcium-activated potassium (SK) channels contribute to action potential repolarization in human atria". Cardiovascular Research. 103 (1): 156–67. doi:10.1093/cvr/cvu121. PMID 24817686.
- ↑ Lee CH, MacKinnon R (May 2018). "Activation mechanism of a human SK-calmodulin channel complex elucidated by cryo-EM structures". Science. 360 (6388): 508–513. Bibcode:2018Sci...360..508L. doi:10.1126/science.aas9466. PMC 6241251. PMID 29724949.
- ↑ Goodman S. "Cardiovascular". Physiology Medical Study Guides. University of Kansas Department of Physiology. Retrieved 2019-09-25.
- ↑ Yan GX, Lankipalli RS, Burke JF, Musco S, Kowey PR (August 2003). "Ventricular repolarization components on the electrocardiogram: cellular basis and clinical significance". Journal of the American College of Cardiology. 42 (3): 401–9. doi:10.1016/s0735-1097(03)00713-7. PMID 12906963.
- ↑ Higuchi T, Nakaya Y (August 1984). "T wave polarity related to the repolarization process of epicardial and endocardial ventricular surfaces". American Heart Journal. 108 (2): 290–5. doi:10.1016/0002-8703(84)90614-8. PMID 6464965.
- ↑ Ali A, Butt N, Sheikh AS (August 2015). "Early repolarization syndrome: A cause of sudden cardiac death". World Journal of Cardiology. 7 (8): 466–75. doi:10.4330/wjc.v7.i8.466. PMC 4549780. PMID 26322186.
- ↑ Zakka, Patrick. "Early Repolarization Syndrome". American College of Cardiology. Retrieved 15 October 2019.
- 1 2 3 Hasegawa Y, Watanabe H, Ikami Y, Otsuki S, Iijima K, Yagihara N, et al. (April 2019). "Early repolarization and risk of lone atrial fibrillation". Journal of Cardiovascular Electrophysiology. 30 (4): 565–568. doi:10.1111/jce.13848. PMID 30661277. S2CID 58641364.
- ↑ Rawshani, Dr. Araz (August 2019). "The early repolarization and pattern syndrome: from ECG criteria to management". Clinical ECG Interpretation.
- 1 2 Bourier F, Denis A, Cheniti G, Lam A, Vlachos K, Takigawa M, et al. (2018). "Early Repolarization Syndrome: Diagnostic and Therapeutic Approach". Frontiers in Cardiovascular Medicine. 5: 169. doi:10.3389/fcvm.2018.00169. PMC 6278243. PMID 30542653.
- ↑ Latshang TD, Kaufmann B, Nussbaumer-Ochsner Y, Ulrich S, Furian M, Kohler M, et al. (September 2016). "Patients with Obstructive Sleep Apnea Have Cardiac Repolarization Disturbances when Travelling to Altitude: Randomized, Placebo-Controlled Trial of Acetazolamide". Sleep. 39 (9): 1631–7. doi:10.5665/sleep.6080. PMC 4989251. PMID 27306264.
External links
- "Repolarization (Animation)". Psychology Department, Hanover College. Retrieved 18 May 2013.