Snakebite
| Snakebite | |
|---|---|
 | |
| A rattlesnake bite on the foot of a 9-year-old girl in Venezuela | |
| Specialty | Emergency medicine |
| Symptoms | Two puncture wounds, redness, swelling, severe pain at the area[1][2] |
| Complications | Bleeding, kidney failure, severe allergic reaction, tissue death around the bite, breathing problems, amputation[1][3] |
| Causes | Snakes[1] |
| Risk factors | Working outside with one's hands (farming, forestry, construction)[1][3] |
| Prevention | Protective footwear, avoiding areas where snakes live, not handling snakes[1] |
| Treatment | Washing the wound with soap and water, antivenom[1][4] |
| Prognosis | Depends on type of snake[5] |
| Frequency | Up to 5 million a year[3] |
| Deaths | 94,000–125,000 per year[3] |
A snakebite is an injury caused by the bite of a snake, especially a venomous snake.[6] A common sign of a bite from a venomous snake is the presence of two puncture wounds from the animal's fangs.[1] Sometimes venom injection from the bite may occur.[3] This may result in redness, swelling, and severe pain at the area, which may take up to an hour to appear.[1][2] Vomiting, blurred vision, tingling of the limbs, and sweating may result.[1][2] Most bites are on the hands, arms, or legs.[2][7] Fear following a bite is common with symptoms of a racing heart and feeling faint.[2] The venom may cause bleeding, kidney failure, a severe allergic reaction, tissue death around the bite, or breathing problems.[1][3] Bites may result in the loss of a limb or other chronic problems.[3] The outcome depends on the type of snake, the area of the body bitten, the amount of venom injected, and the general health of the person bitten.[5] Problems are often more severe in children than adults, due to their smaller size.[3][8][9]
Snakes bite, both as a method of hunting, and as a means of protection.[10] Risk factors for bites include working outside with one's hands such as in farming, forestry, and construction.[1][3] Snakes commonly involved in poisonings include elapids (such as kraits, cobras and mambas), vipers, and sea snakes.[4] The majority of snake species do not have venom and kill their prey by squeezing them.[2] Venomous snakes can be found on every continent except Antarctica.[10] Determining the type of snake that caused a bite is often not possible.[4] The World Health Organization says snakebites are a "neglected public health issue in many tropical and subtropical countries".[9]
Prevention of snake bites can involve wearing protective footwear, avoiding areas where snakes live, and not handling snakes.[1] Treatment partly depends on the type of snake.[1] Washing the wound with soap and water and holding the limb still is recommended.[1][4] Trying to suck out the venom, cutting the wound with a knife, or using a tourniquet is not recommended.[1] Antivenom is effective at preventing death from bites; however, antivenoms frequently have side effects.[3][11] The type of antivenom needed depends on the type of snake involved.[4] When the type of snake is unknown, antivenom is often given based on the types known to be in the area.[4] In some areas of the world getting the right type of antivenom is difficult and this partly contributes to why they sometimes do not work.[3] An additional issue is the cost of these medications.[3] Antivenom has little effect on the area around the bite itself.[4] Supporting the person's breathing is sometimes also required.[4]
The number of venomous snakebites that occur each year may be as high as five million.[3] They result in about 2.5 million poisonings and 20,000 to 125,000 deaths.[3][10] The frequency and severity of bites vary greatly among different parts of the world.[10] They occur most commonly in Africa, Asia, and Latin America,[3] with rural areas more greatly affected.[3][9] Deaths are relatively rare in Australia, Europe and North America.[10][11][12] For example, in the United States, about seven to eight thousand people per year are bitten by venomous snakes (about one in 40 thousand people) and about five people die (about one death per 65 million people).[1]
Signs and symptoms
The most common first symptom of all snakebites is an overwhelming fear, which may contribute to other symptoms, and may include nausea and vomiting, diarrhea, vertigo, fainting, tachycardia, and cold, clammy skin.[2][16] Television, literature, and folklore may contribute to the fear surrounding snakebites, causing people to experience unwarranted thoughts of imminent death.
Dry snakebites and those inflicted by a non-venomous species may still cause severe injury. The bite may become infected from the snake's saliva. The fangs sometimes harbor pathogenic microbial organisms, including Clostridium tetani. Infection is often reported from the bites of vipers, whose fangs are capable of deep puncture wounds, which may introduce infectious organisms into the tissue. Venom may cause anaphylaxis in certain people.
Most snakebites, from either a venomous or a non-venemous snake, will have some type of local effect. Minor pain and redness occur in over 90 percent of cases, although this varies depending on the site.[2] Bites by vipers and some cobras may be extremely painful, with the local tissue sometimes becoming tender and severely swollen within five minutes.[11] This area may also bleed and blister, and may lead to tissue necrosis. Other common initial symptoms of pit viper and viper bites include lethargy, bleeding, weakness, nausea, and vomiting.[2][11] Symptoms may become more life-threatening over time, developing into hypotension, tachypnea, severe tachycardia, severe internal bleeding, altered sensorium, kidney failure, and respiratory failure.[2][11]
Bites by some snakes, such as the kraits, coral snake, Mojave rattlesnake, and the speckled rattlesnake, may cause little or no pain, despite their serious and potentially life-threatening venom.[2] Some people report experiencing a "rubbery", "minty", or "metallic" taste after being bitten by certain species of rattlesnake.[2] Spitting cobras and rinkhalses can spit venom in a person's eyes. This results in immediate pain, ophthalmoparesis, and sometimes blindness.[17][18]

Some Australian elapids and most viper envenomations will cause coagulopathy, sometimes so severe that a person may bleed spontaneously from the mouth, nose, and even old, seemingly healed wounds.[11] Internal organs may bleed, including the brain and intestines, and ecchymosis (bruising) of the skin is often seen.
The venom of elapids, including sea snakes, kraits, cobras, king cobra, mambas, and many Australian species, contains toxins which attack the nervous system, causing neurotoxicity.[2][11][20] The person may present with strange disturbances to their vision, including blurriness. Paresthesia throughout the body, as well as difficulty in speaking and breathing, may be reported.[2] Nervous system problems will cause a huge array of symptoms, and those provided here are not exhaustive. If not treated immediately they may die from respiratory failure.
Venom emitted from some types of cobras, almost all vipers and some sea snakes causes necrosis of muscle tissue.[11] Muscle tissue will begin to die throughout the body, a condition known as rhabdomyolysis. Rhabdomyolysis can result in damage to the kidneys as a result of myoglobin accumulation in the renal tubules. This, coupled with hypotension, can lead to acute kidney injury, and, if left untreated, eventually death.[11]
Cause
In the developing world most snakebites occur in those who work outside such as farmers, hunters, and fishermen. They often happen when a person steps on the snake or approaches it too closely. In the United States and Europe snakebites most commonly occur in those who keep them as pets.[21]
The type of snake that most often delivers serious bites depends on the region of the world. In Africa, it is mambas, Egyptian cobras, puff adders, and carpet vipers. In the Middle East, it is carpet vipers and elapids. In Latin America, it is snakes of the Bothrops and Crotalus types, the latter including rattlesnakes.[21] In North America, rattlesnakes are the primary concern, and up to 95% of all snakebite-related deaths in the United States are attributed to the western and eastern diamondback rattlesnakes.[2] In South Asia, it was previously believed that Indian cobras, common kraits, Russell's viper, and carpet vipers were the most dangerous; other snakes, however, may also cause significant problems in this area of the world.[21]
Pathophysiology
Since envenomation is completely voluntary, all venomous snakes are capable of biting without injecting venom into a person. Snakes may deliver such a "dry bite" rather than waste their venom on a creature too large for them to eat, a behaviour called venom metering.[22] However, the percentage of dry bites varies among species: 80 percent of bites inflicted by sea snakes, which are normally timid, do not result in envenomation,[20] whereas only 25 percent of pit viper bites are dry.[2] Furthermore, some snake genera, such as rattlesnakes, significantly increase the amount of venom injected in defensive bites compared to predatory strikes.[23]
Some dry bites may also be the result of imprecise timing on the snake's part, as venom may be prematurely released before the fangs have penetrated the person.[22] Even without venom, some snakes, particularly large constrictors such as those belonging to the Boidae and Pythonidae families, can deliver damaging bites; large specimens often cause severe lacerations, or the snake itself pulls away, causing the flesh to be torn by the needle-sharp recurved teeth embedded in the person. While not as life-threatening as a bite from a venomous species, the bite can be at least temporarily debilitating and could lead to dangerous infections if improperly dealt with.
While most snakes must open their mouths before biting, African and Middle Eastern snakes belonging to the family Atractaspididae are able to fold their fangs to the side of their head without opening their mouth and jab a person.[24]
Snake venom
It has been suggested that snakes evolved the mechanisms necessary for venom formation and delivery sometime during the Miocene epoch.[25] During the mid-Tertiary, most snakes were large ambush predators belonging to the superfamily Henophidia, which use constriction to kill their prey. As open grasslands replaced forested areas in parts of the world, some snake families evolved to become smaller and thus more agile. However, subduing and killing prey became more difficult for the smaller snakes, leading to the evolution of snake venom.[25] Other research on Toxicofera, a hypothetical clade thought to be ancestral to most living reptiles, suggests an earlier time frame for the evolution of snake venom, possibly to the order of tens of millions of years, during the Late Cretaceous.[26]
Snake venom is produced in modified parotid glands normally responsible for secreting saliva. It is stored in structures called alveoli behind the animal's eyes, and ejected voluntarily through its hollow tubular fangs. Venom is composed of hundreds to thousands of different proteins and enzymes, all serving a variety of purposes, such as interfering with a prey's cardiac system or increasing tissue permeability so that venom is absorbed faster.
Venom in many snakes, such as pit vipers, affects virtually every organ system in the human body and can be a combination of many toxins, including cytotoxins, hemotoxins, neurotoxins, and myotoxins, allowing for an enormous variety of symptoms.[2][27] Earlier, the venom of a particular snake was considered to be one kind only, i.e. either hemotoxic or neurotoxic, and this erroneous belief may still persist wherever the updated literature is hard to access. Although there is much known about the protein compositions of venoms from Asian and American snakes, comparatively little is known of Australian snakes.
The strength of venom differs markedly between species and even more so between families, as measured by median lethal dose (LD50) in mice. Subcutaneous LD50 varies by over 140-fold within elapids and by more than 100-fold in vipers. The amount of venom produced also differs among species, with the Gaboon viper able to potentially deliver from 450–600 milligrams of venom in a single bite, the most of any snake.[28] Opisthoglyphous colubrids have venom ranging from life-threatening (in the case of the boomslang) to barely noticeable (as in Tantilla).
Prevention

Snakes are most likely to bite when they feel threatened, are startled, are provoked, or when they have been cornered.Snakes are likely to approach residential areas when attracted by prey, such as rodents. Regular pest control can reduce the threat of snakes considerably. It is beneficial to know the species of snake that are common in local areas, or while travelling or hiking. Africa, Australia, the Neotropics, and southern Asia in particular are populated by many dangerous species of snake. Being aware of—and ultimately avoiding—areas known to be heavily populated by dangerous snakes is strongly recommended.
When in the wilderness, treading heavily creates ground vibrations and noise, which will often cause snakes to flee from the area. However, this generally only applies to vipers, as some larger and more aggressive snakes in other parts of the world, such as mambas and cobras,[29] will respond more aggressively. If presented with a direct encounter, it is best to remain silent and motionless. If the snake has not yet fled, it is important to step away slowly and cautiously.
The use of a flashlight when engaged in camping activities, such as gathering firewood at night, can be helpful. Snakes may also be unusually active during especially warm nights when ambient temperatures exceed 21 °C (70 °F). It is advised not to reach blindly into hollow logs, flip over large rocks, and enter old cabins or other potential snake hiding-places. When rock climbing, it is not safe to grab ledges or crevices without examining them first, as snakes are cold-blooded and often sunbathe atop rock ledges.
In the United States, more than 40 percent of people bitten by snake intentionally put themselves in harm's way by attempting to capture wild snakes or by carelessly handling their dangerous pets—40 percent of that number had a blood alcohol level of 0.1 percent or more.[30]
It is also important to avoid snakes that appear to be dead, as some species will actually roll over on their backs and stick out their tongue to fool potential threats. A snake's detached head can immediately act by reflex and potentially bite. The induced bite can be just as severe as that of a live snake.[2][31] As a dead snake is incapable of regulating the venom injected, a bite from a dead snake can often contain large amounts of venom.[32]
Treatment
It may be difficult to determine if a bite by any species of snake is life-threatening. A bite by a North American copperhead on the ankle is usually a moderate injury to a healthy adult, but a bite to a child's abdomen or face by the same snake may be fatal. The outcome of all snakebites depends on a multitude of factors: the type of snake, the size, physical condition, and temperature of the snake, the age and physical condition of the person, the area and tissue bitten (e.g., foot, torso, vein or muscle), the amount of venom injected, the time it takes for the person to find treatment, and finally the quality of that treatment.[2][33]
Snake identification
Identification of the snake is important in planning treatment in certain areas of the world, but is not always possible. Ideally the dead snake would be brought in with the person, but in areas where snake bite is more common, local knowledge may be sufficient to recognize the snake. However, in regions where polyvalent antivenoms are available, such as North America, identification of snake is not a high priority item. Attempting to catch or kill the offending snake also puts one at risk for re-envenomation or creating a second person bitten, and generally is not recommended.
The three types of venomous snakes that cause the majority of major clinical problems are vipers, kraits, and cobras. Knowledge of what species are present locally can be crucial, as is knowledge of typical signs and symptoms of envenomation by each type of snake. A scoring system can be used to try to determine the biting snake based on clinical features,[34] but these scoring systems are extremely specific to particular geographical areas.
First aid
Snakebite first aid recommendations vary, in part because different snakes have different types of venom. Some have little local effect, but life-threatening systemic effects, in which case containing the venom in the region of the bite by pressure immobilization is desirable. Other venoms instigate localized tissue damage around the bitten area, and immobilization may increase the severity of the damage in this area, but also reduce the total area affected; whether this trade-off is desirable remains a point of controversy. Because snakes vary from one country to another, first aid methods also vary.
Many organizations, including the American Medical Association and American Red Cross, recommend washing the bite with soap and water. Australian recommendations for snake bite treatment recommend against cleaning the wound. Traces of venom left on the skin/bandages from the strike can be used in combination with a snake bite identification kit to identify the species of snake. This speeds determination of which antivenom to administer in the emergency room.[35]
Pressure immobilization

As of 2008, clinical evidence for pressure immobilization via the use of an elastic bandage is limited.[36] It is recommended for snakebites that have occurred in Australia (due to elapids which are neurotoxic).[37] It is not recommended for bites from non-neurotoxic snakes such as those found in North America and other regions of the world.[37][38] The British military recommends pressure immobilization in all cases where the type of snake is unknown.[39]
The object of pressure immobilization is to contain venom within a bitten limb and prevent it from moving through the lymphatic system to the vital organs. This therapy has two components: pressure to prevent lymphatic drainage, and immobilization of the bitten limb to prevent the pumping action of the skeletal muscles.
Antivenom
Until the advent of antivenom, bites from some species of snake were almost universally fatal.[40] Despite huge advances in emergency therapy, antivenom is often still the only effective treatment for envenomation. The first antivenom was developed in 1895 by French physician Albert Calmette for the treatment of Indian cobra bites. Antivenom is made by injecting a small amount of venom into an animal (usually a horse or sheep) to initiate an immune system response. The resulting antibodies are then harvested from the animal's blood.
Antivenom is injected into the person intravenously, and works by binding to and neutralizing venom enzymes. It cannot undo damage already caused by venom, so antivenom treatment should be sought as soon as possible. Modern antivenoms are usually polyvalent, making them effective against the venom of numerous snake species. Pharmaceutical companies which produce antivenom target their products against the species native to a particular area. Although some people may develop serious adverse reactions to antivenom, such as anaphylaxis, in emergency situations this is usually treatable and hence the benefit outweighs the potential consequences of not using antivenom. Giving adrenaline (epinephrine) to prevent adverse reactions to antivenom before they occur might be reasonable in cases where they occur commonly.[41] Antihistamines do not appear to provide any benefit in preventing adverse reactions.[41]
Outmoded

The following treatments, while once recommended, are considered of no use or harmful, including tourniquets, incisions, suction, application of cold, and application of electricity.[38] Cases in which these treatments appear to work may be the result of dry bites.
- Application of a tourniquet to the bitten limb is generally not recommended. There is no convincing evidence that it is an effective first-aid tool as ordinarily applied.[42] Tourniquets have been found to be completely ineffective in the treatment of Crotalus durissus bites,[43] but some positive results have been seen with properly applied tourniquets for cobra venom in the Philippines.[44] Uninformed tourniquet use is dangerous, since reducing or cutting off circulation can lead to gangrene, which can be fatal.[42] The use of a compression bandage is generally as effective, and much safer.
- Cutting open the bitten area, an action often taken prior to suction, is not recommended since it causes further damage and increases the risk of infection; the subsequent cauterization of the area with fire or silver nitrate (also known as infernal stone) is also potentially threatening.[45]
- Sucking out venom, either by mouth or with a pump, does not work and may harm the affected area directly.[46] Suction started after three minutes removes a clinically insignificant quantity—less than one-thousandth of the venom injected—as shown in a human study.[47] In a study with pigs, suction not only caused no improvement but led to necrosis in the suctioned area.[48] Suctioning by mouth presents a risk of further poisoning through the mouth's mucous tissues.[49] The helper may also release bacteria into the person's wound, leading to infection.
- Immersion in warm water or sour milk, followed by the application of snake-stones (also known as la Pierre Noire), which are believed to draw off the poison in much the way a sponge soaks up water.
- Application of a one-percent solution of potassium permanganate or chromic acid to the cut, exposed area.[45] The latter substance is notably toxic and carcinogenic.
- Drinking abundant quantities of alcohol following the cauterization or disinfection of the wound area.[45]
- Use of electroshock therapy in animal tests has shown this treatment to be useless and potentially dangerous.[50][51][52][53]
In extreme cases, in remote areas, all of these misguided attempts at treatment have resulted in injuries far worse than an otherwise mild to moderate snakebite. In worst-case scenarios, thoroughly constricting tourniquets have been applied to bitten limbs, completely shutting off blood flow to the area. By the time the person finally reached appropriate medical facilities their limbs had to be amputated.
Epidemiology

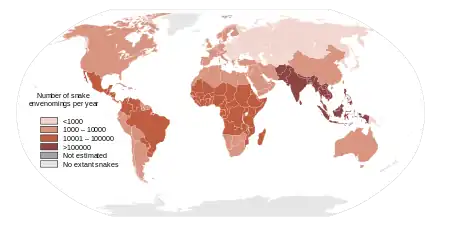
Estimates vary from 1.2 to 5.5 million snakebites, 421,000 to 2.5 million envenomings, and 20,000 to 125,000 deaths.[3][10] Since reporting is not mandatory in much of the world, the data on the frequency of snakebites is not precise.[10] Many people who survive bites have permanent tissue damage caused by venom, leading to disability.[11] Most snake envenomings and fatalities occur in South Asia, Southeast Asia, and sub-Saharan Africa, with India reporting the most snakebite deaths of any country.[10]
Most snakebites are caused by non-venomous snakes. Of the roughly 3,000 known species of snake found worldwide, only 15% are considered dangerous to humans.[2][10] Snakes are found on every continent except Antarctica.[10] The most diverse and widely distributed snake family, the colubrids, has approximately 700 venomous species,[54] but only five genera—boomslangs, twig snakes, keelback snakes, green snakes, and slender snakes—have caused human fatalities.[54]
Worldwide, snakebites occur most frequently in the summer season when snakes are active and humans are outdoors.[10][55] Agricultural and tropical regions report more snakebites than anywhere else.[10][56] In the United States, those bitten are typically male and between 17 and 27 years of age.[2][55][57] Children and the elderly are the most likely to die.[2][33]
Society and culture

Snakes were both revered and worshipped and feared by early civilizations. The ancient Egyptians recorded prescribed treatments for snakebites as early as the Thirteenth Dynasty in the Brooklyn Papyrus, which includes at least seven venomous species common to the region today, such as the horned vipers.[58] In Judaism, the Nehushtan was a pole with a snake made of copper fixed upon it. The object was regarded as a divinely empowered instrument of God that could bring healing to Jews bitten by venomous snakes while they were wandering in the desert after their exodus from Egypt. Healing was said to occur by merely looking at the object as it was held up by Moses.
Historically, snakebites were seen as a means of execution in some cultures. In medieval Europe, a form of capital punishment was to throw people into snake pits, leaving people to die from multiple venomous bites. A similar form of punishment was common in Southern Han during China's Five Dynasties and Ten Kingdoms period and in India.[59] Snakebites were also used as a form of suicide, most notably by Egyptian queen Cleopatra VII, who reportedly died from the bite of an asp—likely an Egyptian cobra[58][60]—after hearing of Mark Antony's death.
Snakebite as a surreptitious form of murder has been featured in stories such as Sir Arthur Conan Doyle's The Adventure of the Speckled Band, but actual occurrences are virtually unheard of, with only a few documented cases.[59][61][62] It has been suggested that Boris III of Bulgaria, who was allied to Nazi Germany during World War II, may have been killed with snake venom,[59] although there is no definitive evidence. At least one attempted suicide by snakebite has been documented in medical literature involving a puff adder bite to the hand.[63]
Research

In 2017, the World Health Organization listed snakebite envenoming as a neglected tropical disease.[65][66][67] In 2019, they launched a strategy to prevent and control snakebite envenoming, which involved a program targeting affected communities and their health systems.[68][69]
Other animals
Several animals acquired immunity against venom of snakes that occur in the same habitat.[70] This has been documented in some humans as well.[71]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 "Venomous Snakes". U.S. National Institute for Occupational Safety and Health. 24 February 2012. Archived from the original on 29 April 2015. Retrieved 19 May 2015.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Gold, Barry S.; Richard C. Dart; Robert A. Barish (1 April 2002). "Bites of venomous snakes". The New England Journal of Medicine. 347 (5): 347–56. doi:10.1056/NEJMra013477. PMID 12151473.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 "Animal bites: Fact sheet N°373". World Health Organization. February 2015. Archived from the original on 4 May 2015. Retrieved 19 May 2015.
- 1 2 3 4 5 6 7 8 "Neglected tropical diseases: Snakebite". World Health Organization. Archived from the original on 30 September 2015. Retrieved 19 May 2015.
- 1 2 Marx, John A. (2010). Rosen's emergency medicine : concepts and clinical practice (7 ed.). Philadelphia: Mosby/Elsevier. p. 746. ISBN 9780323054720. Archived from the original on 21 May 2015.
- ↑ "Definition of Snakebite". www.merriam-webster.com. Archived from the original on 17 June 2019. Retrieved 17 June 2019.
- ↑ Daley, BJ; Torres, J (June 2014). "Venomous snakebites". JEMS : A Journal of Emergency Medical Services. 39 (6): 58–62. PMID 25109149.
- ↑ Peden, M. M. (2008). World Report on Child Injury Prevention. World Health Organization. p. 128. ISBN 9789241563574. Archived from the original on 2 February 2017.
- 1 2 3 "Snake antivenoms: Fact sheet N°337". World Health Organization. February 2015. Archived from the original on 18 April 2017. Retrieved 16 May 2017.
- 1 2 3 4 5 6 7 8 9 10 11 12 Kasturiratne, A.; Wickremasinghe, A. R.; de Silva, N; Gunawardena, NK; Pathmeswaran, A; Premaratna, R; Savioli, L; Lalloo, DG; de Silva, HJ (4 November 2008). "The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths". PLOS Medicine. 5 (11): e218. doi:10.1371/journal.pmed.0050218. PMC 2577696. PMID 18986210.
- 1 2 3 4 5 6 7 8 9 10 Gutiérrez, José María; Bruno Lomonte; Guillermo León; Alexandra Rucavado; Fernando Chaves; Yamileth Angulo (2007). "Trends in Snakebite Envenomation Therapy: Scientific, Technological and Public Health Considerations". Current Pharmaceutical Design. 13 (28): 2935–50. doi:10.2174/138161207782023784. PMID 17979738.
- ↑ Chippaux, J. P. (1998). "Snake-bites: appraisal of the global situation". Bulletin of the World Health Organization. 76 (5): 515–24. PMC 2305789. PMID 9868843.
- 1 2 MedlinePlus – Snake bites Archived 4 December 2010 at the Wayback Machine From Tintinalli JE, Kelen GD, Stapcynski JS, eds. Emergency Medicine: A Comprehensive Study Guide. 6th ed. New York, NY: McGraw Hill; 2004. Update date: 27 February 2008. Updated by: Stephen C. Acosta, MD, Department of Emergency Medicine, Portland VA Medical Center, Portland, OR. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. Retrieved on 19 mars, 2009
- ↑ Health-care-clinic.org – Snake Bite First Aid – Snakebite Archived 16 January 2016 at the Wayback Machine Retrieved on 21 mars, 2009
- ↑ Snake bite image example at MDconsult – Patient Education – Wounds, Cuts and Punctures, First Aid for Archived 7 January 2016 at the Wayback Machine
- ↑ Kitchens C, Van Mierop L (1987). "Envenomation by the Eastern coral snake (Micrurus fulvius fulvius). A study of 39 victims". JAMA. 258 (12): 1615–18. doi:10.1001/jama.258.12.1615. PMID 3625968.
- ↑ Warrell, David A.; L. David Ormerod (1976). "Snake Venom Ophthalmia and Blindness Caused by the Spitting Cobra (Naja Nigricollis) in Nigeria". The American Journal of Tropical Medicine and Hygiene. 25 (3): 525–9. doi:10.4269/ajtmh.1976.25.525. PMID 1084700.
- ↑ Ismail M, al-Bekairi AM, el-Bedaiwy AM, Abd-el Salam MA (1993). "The ocular effects of spitting cobras: I. The ringhals cobra (Hemachatus haemachatus) Venom-Induced corneal opacification syndrome". Clinical Toxicology. 31 (1): 31–41. doi:10.3109/15563659309000372. PMID 8433414.
- ↑ Gutiérrez, José María; Theakston, R. David G; Warrell, David A (2006). "Confronting the Neglected Problem of Snake Bite Envenoming: The Need for a Global Partnership". PLOS Medicine. 3 (6): e150. doi:10.1371/journal.pmed.0030150. PMC 1472552. PMID 16729843.
{{cite journal}}: CS1 maint: url-status (link) - 1 2 Phillips, Charles M. (2002). "Sea snake envenomation" (PDF). Dermatologic Therapy. 15 (1): 58–61(4). doi:10.1046/j.1529-8019.2002.01504.x. Archived (PDF) from the original on 28 April 2011. Retrieved 24 July 2009.
- 1 2 3 Brutto, edited by Hector H. Garcia, Herbert B. Tanowitz, Oscar H. Del (2013). Neuroparasitology and tropical neurology. p. 351. ISBN 9780444534996. Archived from the original on 8 September 2017.
- 1 2 Young, Bruce A.; Cynthia E. Lee; Kylle M. Daley (2002). "Do Snakes Meter Venom?". BioScience. 52 (12): 1121–26. doi:10.1641/0006-3568(2002)052[1121:DSMV]2.0.CO;2.
The second major assumption that underlies venom metering is the snake's ability to accurately assess the target
- ↑ Young, Bruce A.; Krista Zahn (2001). "Venom flow in rattlesnakes: mechanics and metering" (PDF). The Journal of Experimental Biology. 204 (Pt 24): 4345–4351. PMID 11815658. Archived (PDF) from the original on 9 January 2009.
With the species and size of target held constant, the duration of venom flow, maximum venom flow rate and total venom volume were all significantly lower in predatory than in defensive strikes
- ↑ Deufel, Alexandra; David Cundall (2003). "Feeding in Atractaspis (Serpentes: Atractaspididae): a study in conflicting functional constraints". Zoology. 106 (1): 43–61. doi:10.1078/0944-2006-00088. PMID 16351890. Archived from the original on 7 January 2016. Retrieved 19 May 2014.
- 1 2 Jackson, Kate (2003). "The evolution of venom-delivery systems in snakes" (PDF). Zoological Journal of the Linnean Society. 137 (3): 337–354. doi:10.1046/j.1096-3642.2003.00052.x. Archived (PDF) from the original on 10 October 2012. Retrieved 25 July 2009.
- ↑ Fry BG, Vidal N, Norman JA, Vonk FJ, Scheib H, Ramjan SF, Kuruppu S, Fung K, Hedges SB, Richardson MK, Hodgson WC, Ignjatovic V, Summerhayes R, Kochva E (2006). "Early evolution of the venom system in lizards and snakes" (PDF). Nature. 439 (7076): 584–8. Bibcode:2006Natur.439..584F. doi:10.1038/nature04328. PMID 16292255. S2CID 4386245. Archived from the original (PDF) on 30 May 2009. Retrieved 18 September 2009.
- ↑ Russell, Findlay E. (1980). "Snake Venom Poisoning in the United States". Annual Review of Medicine. 31: 247–59. doi:10.1146/annurev.me.31.020180.001335. PMID 6994610. S2CID 1322336.
- ↑ Spawls, Stephen; Bill Branch (1997). The Dangerous Snakes of Africa. Johannesburg: Southern Book Publishers. p. 192. ISBN 978-1-86812-575-3.
- ↑ Haji, R. "Venomous snakes and snake bites" (PDF). Zoocheck Canada. Archived from the original (PDF) on 25 April 2012. Retrieved 25 October 2013.
- ↑ Kurecki B, Brownlee H (1987). "Venomous snakebites in the United States". Journal of Family Practice. 25 (4): 386–92. PMID 3655676.
- ↑ Gold B, Barish R (1992). "Venomous snakebites. Current concepts in diagnosis, treatment, and management". Emerg Med Clin North Am. 10 (2): 249–67. PMID 1559468.
- ↑ Suchard, JR; LoVecchio F. (1999). "Envenomations by Rattlesnakes Thought to Be Dead". The New England Journal of Medicine. 340 (24): 1930. doi:10.1056/NEJM199906173402420. PMID 10375322.
- 1 2 Gold BS, Wingert WA (1994). "Snake venom poisoning in the United States: a review of therapeutic practice". South. Med. J. 87 (6): 579–89. doi:10.1097/00007611-199406000-00001. PMID 8202764. S2CID 37771848. Archived from the original on 2021-08-29. Retrieved 2019-12-03.
- ↑ Pathmeswaran A, Kasturiratne A, Fonseka M, Nandasena S, Lalloo D, de Silva H (2006). "Identifying the biting species in snakebite by clinical features: an epidemiological tool for community surveys". Trans R Soc Trop Med Hyg. 100 (9): 874–8. doi:10.1016/j.trstmh.2005.10.003. PMID 16412486.
- ↑ Chris Thompson. "Treatment of Australian Snake Bites". Australian anaesthetists' website. Archived from the original on 23 March 2007.
- ↑ Currie, Bart J.; Elizabeth Canale; Geoffrey K. Isbister (2008). "Effectiveness of pressure-immobilization first aid for snakebite requires further study". Emergency Medicine Australasia. 20 (3): 267–270(4). doi:10.1111/j.1742-6723.2008.01093.x. PMID 18549384.
- 1 2 Patrick Walker, J; Morrison, R; Stewart, R; Gore, D (January 2013). "Venomous bites and stings". Current Problems in Surgery. 50 (1): 9–44. doi:10.1067/j.cpsurg.2012.09.003. PMID 23244230.
- 1 2 American College of Medical Toxicology, American Academy of Clinical, Toxicology, American Association of Poison Control Centers, European Association of Poison Control Centres, International Society of, Toxinology, Asia Pacific Association of Medical Toxicology (December 2011). "Pressure immobilization after North American Crotalinae snake envenomation". Journal of Medical Toxicology. 7 (4): 322–3. doi:10.1007/s13181-011-0174-2. PMC 3550191. PMID 22065370.
- ↑ Wall, C (September 2012). "British Military snake-bite guidelines: pressure immobilisation". Journal of the Royal Army Medical Corps. 158 (3): 194–8. doi:10.1136/jramc-158-03-09. PMID 23472565. S2CID 22415445.
- ↑ White, Julian (November 1991). "Oxyuranus microlepidotus". Chemical Safety Information from Intergovernmental Organizations. Archived from the original on 3 August 2009. Retrieved 24 July 2009.
Without appropriate antivenom treatment up to 75% of taipan bites will be fatal. Indeed, in the era prior to specific antivenom therapy, virtually no survivors of taipan bite were recorded.
- 1 2 Nuchpraryoon, I; Garner, P (2000). "Interventions for preventing reactions to snake antivenom". The Cochrane Database of Systematic Reviews (2): CD002153. doi:10.1002/14651858.CD002153. PMC 7017854. PMID 10796682.
- 1 2 Theakston RD (1997). "An objective approach to antivenom therapy and assessment of first-aid measures in snake bite" (PDF). Ann. Trop. Med. Parasitol. 91 (7): 857–65. doi:10.1080/00034989760626. PMID 9625943. Archived (PDF) from the original on 30 December 2008.
- ↑ Amaral CF, Campolina D, Dias MB, Bueno CM, Rezende NA (1998). "Tourniquet ineffectiveness to reduce the severity of envenoming after Crotalus durissus snake bite in Belo Horizonte, Minas Gerais, Brazil". Toxicon. 36 (5): 805–8. doi:10.1016/S0041-0101(97)00132-3. PMID 9655642.
- ↑ Watt G, Padre L, Tuazon ML, Theakston RD, Laughlin LW (1988). "Tourniquet application after cobra bite: delay in the onset of neurotoxicity and the dangers of sudden release". Am. J. Trop. Med. Hyg. 38 (3): 618–22. doi:10.4269/ajtmh.1988.38.618. PMID 3275141. S2CID 29451180.
- 1 2 3 Lupano, Guglielmo; Peola, Paolo (1915). Corso di Scienze Naturali a uso delle Scuole Complementari [A Course of Natural Sciences for the Complementary Institutes] (in Italian). G.B. Paravia. p. 68.
{{cite book}}: CS1 maint: unrecognized language (link) - ↑ Holstege CP, Singletary EM (2006). "Images in emergency medicine. Skin damage following application of suction device for snakebite". Annals of Emergency Medicine. 48 (1): 105, 113. doi:10.1016/j.annemergmed.2005.12.019. PMID 16781926.
- ↑ Alberts M, Shalit M, LoGalbo F (2004). "Suction for venomous snakebite: a study of "mock venom" extraction in a human model". Annals of Emergency Medicine. 43 (2): 181–6. doi:10.1016/S0196-0644(03)00813-8. PMID 14747805.
- ↑ Bush SP, Hegewald KG, Green SM, Cardwell MD, Hayes WK (2000). "Effects of a negative pressure venom extraction device (Extractor) on local tissue injury after artificial rattlesnake envenomation in a porcine model". Wilderness & Environmental Medicine. 11 (3): 180–8. doi:10.1580/1080-6032(2000)011[0180:EOANPV]2.3.CO;2. PMID 11055564.
- ↑ Riggs BS, Smilkstein MJ, Kulig KW, et al. Rattlesnake envenomation with massive oropharyngeal edema following incision and suction (Abstract). Presented at the AACT/AAPCC/ABMT/CAPCC Annual Scientific Meeting, Vancouver, Canada, September 27 October 2, 1987.
- ↑ Russell F (1987). "Another warning about electric shock for snakebite". Postgrad Med. 82 (5): 32. doi:10.1080/00325481.1987.11699990. PMID 3671201.
- ↑ Ryan A (1987). "Don't use electric shock for snakebite". Postgrad Med. 82 (2): 42. doi:10.1080/00325481.1987.11699922. PMID 3497394.
- ↑ Howe N, Meisenheimer J (1988). "Electric shock does not save snakebitten rats". Annals of Emergency Medicine. 17 (3): 254–6. doi:10.1016/S0196-0644(88)80118-5. PMID 3257850.
- ↑ Johnson E, Kardong K, Mackessy S (1987). "Electric shocks are ineffective in treatment of lethal effects of rattlesnake envenomation in mice". Toxicon. 25 (12): 1347–9. doi:10.1016/0041-0101(87)90013-4. PMID 3438923.
- 1 2 Mackessy, Stephen P. (2002). "Biochemistry and pharmacology of colubrid snake venoms" (PDF). Journal of Toxicology: Toxin Reviews. 21 (1–2): 43–83. CiteSeerX 10.1.1.596.5081. doi:10.1081/TXR-120004741. S2CID 86568032. Archived from the original (PDF) on 2 June 2010. Retrieved 26 September 2009.
Estimates of the number of venomous colubrids approach 700 species. Most may not produce a venom capable of causing serious damage to humans, but at least five species (Dispholidus typus, Thelotornis capensis, Rhabdophis tigrinus, Philodryas olfersii and Tachymenis peruviana) have caused human fatalities
- 1 2 Wingert W, Chan L (1 January 1988). "Rattlesnake Bites in Southern California and Rationale for Recommended Treatment". West J Med. 148 (1): 37–44. PMC 1026007. PMID 3277335.
- ↑ Gutiérrez, José María; R. David G. Theakston; David A. Warrell (6 June 2006). "Confronting the Neglected Problem of Snake Bite Envenoming: The Need for a Global Partnership". PLOS Medicine. 3 (6): e150. doi:10.1371/journal.pmed.0030150. PMC 1472552. PMID 16729843.
{{cite journal}}: CS1 maint: url-status (link) - ↑ Parrish H (1966). "Incidence of treated snakebites in the United States". Public Health Rep. 81 (3): 269–76. doi:10.2307/4592691. JSTOR 4592691. PMC 1919692. PMID 4956000.
- 1 2 Schneemann M, Cathomas R, Laidlaw ST, El Nahas AM, Theakston RD, Warrell DA (2004). "Life-threatening envenoming by the Saharan horned viper (Cerastes cerastes) causing micro-angiopathic haemolysis, coagulopathy and acute renal failure: clinical cases and review" (PDF). QJM: An International Journal of Medicine. 97 (11): 717–27. doi:10.1093/qjmed/hch118. PMID 15496528. Retrieved 4 September 2009.
This echoed the opinion of the Egyptian physicians who wrote the earliest known account of the treatment of snake bite, the Brooklyn Museum Papyri, dating perhaps from 2200 BC. They regarded bites by horned vipers 'fy' as non-lethal, as the victims could be saved.
- 1 2 3 Anil, Aggrawal (2004). "Homicide with snakes: A distinct possibility and its medicolegal ramifications". Anil Aggrawal's Internet Journal of Forensic Medicine and Toxicology. 4 (2). Archived from the original on 18 July 2007.
- ↑ Crawford, Amy (1 April 2007). "Who Was Cleopatra? Mythology, propaganda, Liz Taylor and the real Queen of the Nile". Smithsonian. Archived from the original on 13 November 2013. Retrieved 4 September 2009.
- ↑ Warrell, D.A. (2009). "Commissioned article: management of exotic snakebites". QJM: An International Journal of Medicine. 102 (9): 593–601. doi:10.1093/qjmed/hcp075. PMID 19535618.
- ↑ Straight, Richard C.; James L. Glenn (1994). "Human fatalities caused by venomous animals in Utah, 1900–90". Great Basin Naturalist. 53 (4): 390–4. doi:10.5962/bhl.part.16607. Archived from the original on 8 October 2011. Retrieved 4 September 2009.
A third unusual death was a tragic fatality (1987), recorded as a homicide, which resulted when a large rattlesnake (G. v. lutosus) bit a 22-month-old girl after the snake had been placed around her neck (Washington County). The child died in approximately 5 h.
- ↑ Strubel, T.; A. Birkhofer; F. Eyer; K.D. Werber; H. Förstl (2008). "Suizidversuch durch Schlangenbiss: Kasuistik und Literaturübersicht" [Attempted suicide by snake bite: Case report and literature survey]. Der Nervenarzt (in German). 79 (5): 604–6. doi:10.1007/s00115-008-2431-4. PMID 18365165. S2CID 21805895.
Ein etwa 20-jähriger Arbeiter wurde nach dem Biss seiner Puffotter (Bitis arietans) in die Hand auf die toxikologische Intensivstation aufgenommen. Zunächst berichtet der Patient, dass es beim „Melken“ der Giftschlange zu dem Biss gekommen sei, erst im weiteren Verlauf räumt er einen Suizidversuch ein. Als Gründe werden Einsamkeit angeführt sowie unerträgliche Schmerzen im Penis.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Korambayil, PM; Ambookan, PV; Abraham, SV; Ambalakat, A (January 2015). "A Multidisciplinary Approach with Hyperbaric Oxygen Therapy Improve Outcome in Snake Bite Injuries". Toxicology international. 22 (1): 104–9. doi:10.4103/0971-6580.172287. PMID 26862269.
- ↑ Abela-Ridder, Bernadette; Cooke, Emer; Malecela, Mwelecele Ntuli; Minghui, Ren (22 May 2019). "WHO's Snakebite Envenoming Strategy for prevention and control". The Lancet Global Health. 7 (7): e837–e838. doi:10.1016/S2214-109X(19)30225-6. ISSN 2214-109X. PMID 31129124. Archived from the original on 29 August 2021. Retrieved 30 May 2019.
- ↑ Schiermeier, Quirin (16 May 2019). "Snakebite crisis gets US$100-million boost for better antivenoms". Nature. doi:10.1038/d41586-019-01557-0. PMID 32409762. Archived from the original on 16 May 2019. Retrieved 30 May 2019.
- ↑ "WHO | Snakebite envenomation turns again into a neglected tropical disease!". WHO. Archived from the original on 2020-07-15. Retrieved 2020-07-25.
- ↑ "Snakebite: WHO targets 50% reduction in deaths and disabilities". World Health Organization. Archived from the original on 8 May 2019. Retrieved 30 May 2019.
- ↑ Warrell, David A.; Harrison, Robert A.; Turner, Michael; Fan, Hui Wen; Junghanss, Thomas; Habib, Abdulrazaq G.; Nickerson, Andrea D.; Bulfone, Tommaso C.; Ainsworth, Stuart; Abela-Ridder, Bernadette; Faiz, Mohd Abul; Williams, David J. (21 February 2019). "Strategy for a globally coordinated response to a priority neglected tropical disease: Snakebite envenoming". PLOS Neglected Tropical Diseases. 13 (2): e0007059. doi:10.1371/journal.pntd.0007059. ISSN 1935-2735. PMC 6383867. PMID 30789906.
- ↑ Bittel, Jason. "The Animals That Venom Can't Touch". Smithsonian. Archived from the original on 30 May 2018. Retrieved 29 May 2018.
- ↑ Collins, Britt (11 February 2018). "Poison pass: the man who became immune to snake venom". the Guardian. Archived from the original on 29 May 2018. Retrieved 29 May 2018.
- Bibliography
- Greene, Harry W. (1997). Snakes: The Evolution of Mystery in Nature. Berkeley, CA: University of California Press. ISBN 978-0-520-20014-2.
- Stephen P., Mackessy, ed. (2010). Handbook of Venoms and Toxins of Reptiles (2nd ed.). Boca Raton, FL: CRC Press. ISBN 978-0-8493-9165-1.
- Valenta, Jiri (2010). Venomous Snakes: Envenoming, Therapy (2nd ed.). Hauppauge, NY: Nova Science Publishers. ISBN 978-1-60876-618-5.
Further reading
| Library resources about Snakebite |
- Campbell, Jonathan A.; William W. Lamar (2004). The Venomous Reptiles of the Western Hemisphere. Ithaca, NY: Cornell University Press. ISBN 978-0-8014-4141-7
- Spawls, Stephen; Bill Branch (1995). The Dangerous Snakes of Africa: Natural History, Species Directory, Venoms and Snakebite. Sanibel Island, FL: Ralph Curtis Publishing. ISBN 978-0-88359-029-4
- Sullivan JB, Wingert WA, Norris Jr RL. (1995). North American Venomous Reptile Bites. Wilderness Medicine: Management of Wilderness and Environmental Emergencies. 3: 680–709.
- Thorpe, Roger S.; Wolfgang Wüster, Anita Malhotra (1996). Venomous Snakes: Ecology, Evolution, and Snakebite'. Oxford, England: Oxford University Press. ISBN 978-0-19-854986-4
External links
- WHO Snake Antivenoms Database Archived 2010-05-07 at the Wayback Machine
- Organization (2016). Guidelines for the management of snakebites. Regional Office for South-East Asia, World Health Organization. hdl:10665/249547. ISBN 9789290225300.
| Classification | |
|---|---|
| External resources |
|
