This article was co-authored by Pippa Elliott, MRCVS. Dr. Elliott, BVMS, MRCVS is a veterinarian with over 30 years of experience in veterinary surgery and companion animal practice. She graduated from the University of Glasgow in 1987 with a degree in veterinary medicine and surgery. She has worked at the same animal clinic in her hometown for over 20 years.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 20,671 times.
Feline cancer is not as common as canine cancer, but is often more aggressive and advanced when diagnosed.[1] As a pet owner, you may be uncertain about how to move forward with treating your cat’s cancer. Fortunately, advancements in veterinary oncology have led to vastly improved knowledge about feline cancer and how best to treat it. Before proceeding with treatment, take time to learn as much as you can about the diagnosis and treatment of feline cancer.
Steps
Deciding Whether to Treat Your Cat’s Cancer
-
1Evaluate your cat’s quality of life. Quality of life should play a major factor in deciding whether to treat your cat’s cancer.[2] If your cat seems to be generally in good spirits and does not have unmanageable pain or severe cancer-related symptoms, she may be able to handle the rigors of cancer treatment. However, if her quality of life is suffering and she seems miserable, treatment may not be the best option for her.
- As much as you may want to do everything you can to treat your cat, your cat’s quality of life should take priority.
- Realize that putting her through cancer treatment could make her feel even worse.
-
2Consider the cost of treatment. Treating feline cancer can be very expensive, especially if you seek treatment by a veterinary oncologist. For example, diagnosis alone can cost several hundred dollars ($500 to $800). Depending on the type of treatment that the oncologist recommends, your cat’s treatment could cost anywhere from about $800 to $6000.[3]
- Your veterinarian may be able to treat your cat for less,[4] but may not have access to more specialized treatment options (e.g., radiation therapy). He or she may end up referring you to a veterinary oncologist.
- Additional costs may include special food, pain medications, and anti-nausea medications.
- You may feel guilty about weighing the cost of treatment against your emotional want to treat your cat’s cancer. However, it may not be financially feasible for you to devote a significant portion of your finances towards your cat’s cancer treatment.
Advertisement -
3Discuss the requirements of care with your veterinarian. Treating your cat’s cancer may involve frequent trips to your veterinarian’s office, depending on the type of treatment.[5] Determine if you would be able to manage frequent office visits with your work schedule.
- Depending on where you live, a veterinary oncologist may not be nearby. You may need to factor in the distance to reach a treatment center when deciding whether to move forward with treating your cat’s cancer.
- Your cat’s cancer treatment may involve at-home administration of oral chemotherapy.[6] Discuss this possibility with your veterinarian, and if you would feel comfortable giving your cat chemotherapy on your own.
- Having a full understanding of your cat’s needs during her cancer treatment will help you make a more informed decision about whether to proceed with the treatment.
- Another factor is the cat's temperament. Many chemo drugs need to be given via a catheter in the vein. If the cat is highly stressed or aggressive, then sedation may be required so you should weigh up if your cat is can cope with the additional distress and if you can cope financially with the added cost of sedation.
Taking Your Cat to Your Veterinarian
-
1Observe your cat’s clinical signs. Cats often try to mask their clinical signs when they are sick.[7] As attentive a pet owner as you may be, you may not immediately notice when your cat is feeling unwell. Unfortunately, masking illness can make cancer detection difficult.[8]
- The later the cancer is diagnosed by your veterinarian, the costlier and more aggressive the treatment may be.[9]
- A new lump or bump is an easily visible sign of potential cancer.[10]
- Clinical signs may vary based on the location of the tumor. For example, a gastrointestinal cancer would cause such symptoms as vomiting and diarrhea. With skin cancer, you may see redness and irritation, along with a lump or bump.[11]
- Be mindful that your cat’s cancer may not produce any clinical signs initially, and then cause a sudden appearance of clinical signs.[12]
-
2Schedule an appointment with your veterinarian. Take your cat to your veterinarian as soon as you start to notice clinical signs. You may not suspect cancer, but your veterinarian can run various diagnostic tests to determine why your cat is ill. When it comes to cancer, early detection and diagnosis are key.[13]
- Diagnostic tests that your veterinarian may run include imaging (e.g., x-rays, ultrasound), blood work, and a biopsy.[14]
- Be aware that biopsies are not always conclusive.[15]
- Your veterinarian may also want to test for feline leukemia virus (FeLV) and feline immunodeficiency virus (FIV), both of which have been associated with cancer in cats (especially FeLV).[16]
- The diagnostic tests can help to assess your cat’s overall health and her ability to undergo cancer treatment, as well as determine how advanced the cancer is.[17]
-
3Talk with your veterinarian. If the diagnostic tests reveal that your cat has cancer, talk with your veterinarian about how to move forward. He or she will understand that you will have a lot of questions and concerns about treating your cat’s cancer. For example, ask about the cost of cancer treatment, which could range from several hundred to several thousand dollars.[18]
- You can also ask what may have caused your cat’s cancer. Keep in mind that feline cancer often has unknown causes.[19] Some causes that are known include FeLV and repeated sun exposure (especially in white-headed cats).[20]
- Consider getting a second opinion from a veterinary oncologist. Different veterinarians have different approaches to cancer treatment, so it may help to learn the perspectives of several veterinarians regarding your cat’s cancer treatment.[21]
- A veterinary oncologist may have knowledge of treatment options that your own veterinarian may not be aware of.[22]
Exploring Your Treatment Options
-
1Discuss surgical tumor removal with your veterinarian. Surgery is a very common form of cancer treatment, particularly for skin tumors and internal tumors with distinct borders.[23] Among the various cancer treatment options, it is considered most likely to be curative.[24]
- The size of some internal tumors can cause your cat to feel unwell. For large tumors, surgical therapy can reduce the size of tumor (‘debulking’) and thus relieve some of your cat’s symptoms.[25]
- Some cancers can spread to surrounding healthy tissue. For this reason, healthy tissue is often removed with the cancerous tissue during surgery.[26] The healthy tissue can then be microscopically analyzed for signs of cancer cell invasion.
- Be aware that surgery may not prevent the risk of cancer recurrence in your cat. Your veterinarian can discuss this likelihood as you are considering treatment options.[27]
-
2Learn about chemotherapy. Chemotherapy is another common cancer treatment. For feline cancer, it is not curative. Rather, chemotherapy is used to slow cancer cell growth and relieve clinical signs.[28] It is also used when surgery is not an option, such as when the cancer has spread to other body parts.[29]
- Your veterinarian will probably consult with a veterinary oncologist to develop a unique chemotherapy regimen for your cat.
- The chemotherapy regimen may change during the course of your cat’s treatment, depending on such factors as your cat’s tolerance of the medication and the cancer’s response to the medication.
- Fortunately, the side effects of chemotherapy are milder in cats than in people. The most common side effects are gastrointestinal upset (e.g., vomiting, diarrhea) and loss of energy, and are frequently mild.
- Chemotherapy can be administered in different ways (e.g., intravenous, orally) and is administered over several minutes to several hours.
-
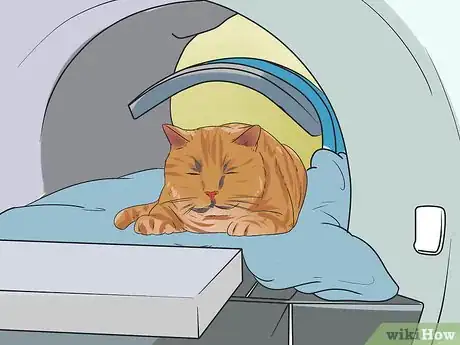
3Ask your veterinarian about radiation therapy. Radiation therapy (RT) is another cancer treatment option for your cat. It uses x-rays or electrons to kill cancer cells. RT is often used in combination with chemotherapy and may be used after surgery if the entire tumor could not be surgically removed.
- Your veterinarian may suggest RT if your cat’s tumor is in a location that would make it dangerous to remove.
- Specialized imaging modalities, such as computed tomography or magnetic resonance imaging, may be needed to identify the planned site of RT.
- Because complete stillness is required during a session of RT, your cat would need to be under general anesthesia.
- RT is typically administered in small doses over several weeks. A veterinary oncologist would be able to develop a radiation therapy treatment plan for your cat.
- Side effects of RT vary depending on the dose and type of radiation. Common side effects are redness and discomfort at the treatment site. Your cat may need pain medication to relieve this discomfort.
Caring For Your Cat at Home
-
1Feed your cat a healthy diet. Cancer can produce what is called cancer cachexia: malnutrition and severe weight loss, even with an adequate amount of food being eaten. Cancer cachexia can get even worse if your cat has a loss of appetite because of the cancer and/or cancer treatment.[30] Addressing your cat’s nutritional needs during her cancer treatment is crucial to counteracting the cachexia and keeping her as healthy and strong as possible.
- There are many causes of cancer-related weight loss and loss of appetite: altered sense of taste and smell, GI upset, tumor location (e.g., in the stomach or intestines), and changes in metabolism.[31]
- During cancer treatment, your cat will need to eat foods that are energy dense.[32]
- Fat should be about 25-40% of your cat’s diet. Cancer cells typically don’t use fat, but fat can be used as an energy source for your cat.[33]
- Protein should be another main component of your cat’s diet (40-50%), since cancer cachexia leads to loss of muscle mass and, subsequently, protein.[34]
- Your cat’s diet during cancer treatment should be low in carbohydrates, since cancer cells use glucose for energy.[35]
- Omega-3 fatty acids and vitamin B12 are good additions to your cat’s diet.[36]
- Consult with your veterinarian to develop the ideal treatment plan for your cat while she is being treated for cancer.
-
2Administer medications to relieve treatment side effects. Although your cat will likely experience only mild treatment side effects, she may still need additional medication to relieve her discomfort. For example, she may need pain medication, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids.[37]
- Meloxicam and ketoprofen are NSAIDs approved for use in cats.[38] Your veterinarian will need to write you a prescription for these medications. However, be aware that corticosteroids are a common part of a chemotherapy protocol. NSAIDs are NOT compatible with steroids. To combine the two could cause serious, potentially life threatening side effects such as bleeding from the gut. Always check with your veterinarian before giving any medication to your cat.
- GI upset is a common side effect of NSAIDs.[39]
- Your veterinarian may want to prescribe an opiate, such as morphine, if your cat has moderate to severe pain.[40]
- Do not use give your cat Tylenol. Tylenol is toxic to cats.[41]
- Your cat may also need anti-nausea medication to relieve treatment-induced nausea.
- Follow your veterinarian’s instructions on administering medication to your cat at home.
-
3Take precautions to prevent drug exposure at home. This is applicable if your cat is receiving chemotherapy treatment. The drugs will be in your cat’s system for up to 72 hours after drug administration,[42] so you will need to be extra careful when handling your cat’s waste and bedding after her treatment sessions.
- Wear disposable gloves when you clean your cat’s litter box and any accidents.[43]
- Clean her litter box daily.[44]
- Always double bag the waste and wash your hands after cleaning up after your cat.[45]
- Double bag your gloves when you take them off.[46]
- Keep your other pets away from your cat’s waste.[47]
- Clean your cat’s bedding separately.[48]
-
4Administer at-home chemotherapy. If you are administering chemotherapy to your cat at home, it is extremely important to prevent your own exposure to the drugs. For example, you should wear gloves and refrain from eating, drinking, or chewing gum when giving her the drugs. Also, double bag your gloves when you have finished administering the chemotherapy.[49]
Expert Q&A
-
QuestionDo cats have chemo side effects?
 Pippa Elliott, MRCVSDr. Elliott, BVMS, MRCVS is a veterinarian with over 30 years of experience in veterinary surgery and companion animal practice. She graduated from the University of Glasgow in 1987 with a degree in veterinary medicine and surgery. She has worked at the same animal clinic in her hometown for over 20 years.
Pippa Elliott, MRCVSDr. Elliott, BVMS, MRCVS is a veterinarian with over 30 years of experience in veterinary surgery and companion animal practice. She graduated from the University of Glasgow in 1987 with a degree in veterinary medicine and surgery. She has worked at the same animal clinic in her hometown for over 20 years.
Veterinarian Yes, but they typically aren't as bad. Chemotherapy protocols for cats are designed to minimize distress to the patient. The doses used are smaller than in people, and therefore the side effects are less severe.
Yes, but they typically aren't as bad. Chemotherapy protocols for cats are designed to minimize distress to the patient. The doses used are smaller than in people, and therefore the side effects are less severe.
Warnings
- Your cat’s health may seriously decline during her cancer treatment. If this happens, you may need to consider euthanizing her.[54] This can be a very difficult decision to make, so talk openly with your veterinarian about the possibility of euthanasia.⧼thumbs_response⧽
- The grief over losing a pet can be overwhelming. Pet bereavement services are available to help you cope with and manage your grief.[55] Also, many veterinary schools have pet support hotlines to help pet owners cope with the loss of a pet.⧼thumbs_response⧽
- Tylenol is toxic to cats.[56]⧼thumbs_response⧽
References
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment
- ↑ https://www.aspca.org/pet-care/cat-care/cancer
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment?page=3
- ↑ https://www.bluecross.org.uk/pet-advice/coping-cancer-cats
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment
- ↑ https://www.aspca.org/pet-care/cat-care/cancer
- ↑ https://www.bluecross.org.uk/pet-advice/coping-cancer-cats
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment?page=3
- ↑ https://www.aspca.org/pet-care/cat-care/cancer
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment?page=2
- ↑ https://www.bluecross.org.uk/pet-advice/coping-cancer-cats
- ↑ https://www.bluecross.org.uk/pet-advice/coping-cancer-cats
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment?page=3
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment?page=2
- ↑ https://www.aspca.org/pet-care/cat-care/cancer
- ↑ https://www.aspca.org/pet-care/cat-care/cancer
- ↑ http://pets.webmd.com/cats/guide/cancer-in-cats-types-symptoms-prevention-and-treatment?page=4
- ↑ https://www.bluecross.org.uk/pet-advice/coping-cancer-cats
- ↑ http://icatcare.org/advice/cat-health/treatment-cancer-cats
- ↑ http://icatcare.org/advice/cat-health/treatment-cancer-cats
- ↑ http://icatcare.org/advice/cat-health/treatment-cancer-cats
- ↑ https://www.bluecross.org.uk/pet-advice/coping-cancer-cats
- ↑ https://www.bluecross.org.uk/pet-advice/coping-cancer-cats
- ↑ https://www.bluecross.org.uk/pet-advice/coping-cancer-cats
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3614
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3614
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3614
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3614
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3614
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3614
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3614
- ↑ https://www.dvm360.com/view/treating-cancer-pain-dogs-and-cats
- ↑ https://www.dvm360.com/view/treating-cancer-pain-dogs-and-cats
- ↑ https://www.dvm360.com/view/treating-cancer-pain-dogs-and-cats
- ↑ https://www.dvm360.com/view/treating-cancer-pain-dogs-and-cats
- ↑ https://www.dvm360.com/view/treating-cancer-pain-dogs-and-cats
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3608
- ↑ http://www.peteducation.com/article.cfm?c=1+2120&aid=3614
- ↑ https://www.bluecross.org.uk/pet-advice/coping-cancer-cats
- ↑ https://www.bluecross.org.uk/pet-advice/coping-cancer-cats
- ↑ https://www.dvm360.com/view/treating-cancer-pain-dogs-and-cats