Effects of nicotine on human brain development
Exposure to nicotine, from conventional or electronic cigarettes during adolescence can impair the developing human brain.[1] E-cigarette use is recognized as a substantial threat to adolescent behavioral health.[notes 1][3] The use of tobacco products, no matter what type, is almost always started and established during adolescence when the developing brain is most vulnerable to nicotine addiction.[notes 2][5] Young people's brains build synapses faster than adult brains.[6] Because addiction is a form of learning, adolescents can get addicted more easily than adults.[6] The nicotine in e-cigarettes can also prime the adolescent brain for addiction to other drugs such as cocaine.[6] Exposure to nicotine and its great risk of developing an addiction, are areas of significant concern.[7]
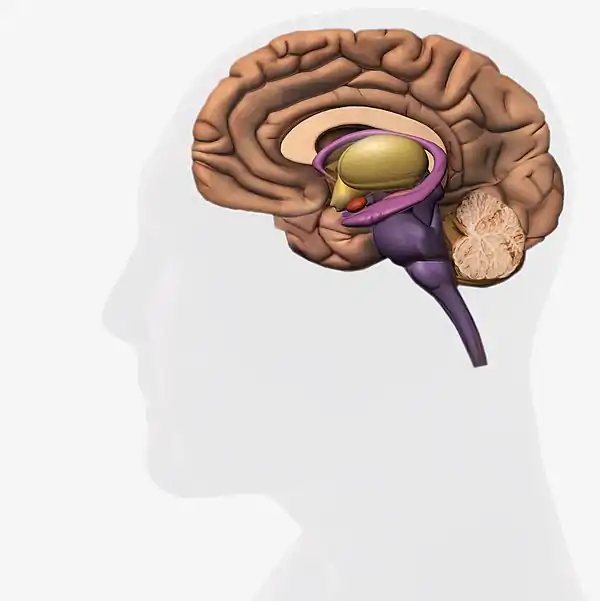
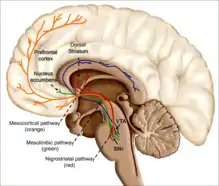
Nicotine is a parasympathomimetic stimulant[8] that binds to and activates nicotinic acetylcholine receptors in the brain,[9] which subsequently causes the release of dopamine and other neurotransmitters, such as norepinephrine, acetylcholine, serotonin, gamma-aminobutyric acid, glutamate and endorphins.[10] Nicotine interferes with the blood–brain barrier function, and as a consequence raises the risk of brain edema and neuroinflammation.[11] When nicotine enters the brain it stimulates, among other activities, the midbrain dopaminergic neurons situated in the ventral tegmental area and pars compacta.[12]
Nicotine negatively affects the prefrontal cortex of the developing brain. Prenatal nicotine exposure can result in long-term adverse effects to the developing brain.[notes 3][14] Prenatal nicotine exposure has been associated with dysregulation of catecholaminergic, serotonergic, and other neurotransmitter systems.[15] E-liquid exposure whether intentional or unintentional from ingestion, eye contact, or skin contact can cause adverse effects such as seizures and anoxic brain trauma.[16] A study on the offspring of the pregnant mice, which were exposed to nicotine-containing e-liquid, showed significant behavioral alterations.[17] This indicated that exposure to e-cigarette components in a susceptible time period of brain development could induce persistent behavioral changes.[17]
Effects of nicotine
The health effects of long-term nicotine use is unknown.[18] It may be decades before the long-term health effects of nicotine e-cigarette aerosol (vapor) inhalation is known.[19] Short-term nicotine use excites the autonomic ganglia nerves and autonomic nerves, but chronic use seems to induce negative effects on endothelial cells.[20] Nicotine may result in neuroplasticity modifications in the brain.[21] Nicotine has been demonstrated to alter the amounts of brain-derived neurotrophic factor in humans.[22] Side effects of nicotine include mild headache, headache, dysphoria, depressed mood, irritability, aggression, frustration, impatience, anxiety, sleep disturbances, abnormal dreams, irritability, and dizziness.[23]
The neuroregulation and structural interactions in the brain and lungs from nicotine may interfere with an array of reflexes and responses.[24] These alterations may raise the risk of hypoxia.[24] Continued use of nicotine may result in harmful effects to women's brains because it restricts estrogen signaling.[24] This could lead to making the brain more vulnerable to ischemia.[24] A 2015 review concluded that "Nicotine acts as a gateway drug on the brain, and this effect is likely to occur whether the exposure is from smoking tobacco, passive tobacco smoke or e-cigarettes."[25]
Nicotine may have a profound impact on sleep.[26] The effects on sleep vary after being intoxicated, during withdrawal, and from long-term use.[26] Nicotine may result in arousal and wakefulness, mainly via incitement in the basal forebrain.[27] Nicotine withdrawal, after abstaining from nicotine use in non-smokers, was linked with longer overall length of sleep and REM rebound.[26] A 2016 review states that "Although smokers say they smoke to control stress, studies show a significant increase in cortisol concentrations in daily smokers compared with occasional smokers or nonsmokers. These findings suggest that, despite the subjective effects, smoking may actually worsen the negative emotional states. The effects of nicotine on the sleep-wake cycle through nicotine receptors may have a functional significance. Nicotine receptor stimulation promotes wake time and reduces both total sleep time and rapid eye movement sleep."[7]
Effects of nicotine diagram
Possible effects of nicotine on the developing human brain
|
Comparative risk assessment chart
| Harms | Benefits |
|---|---|
| Increased youth exposure to nicotine and potentially greater initiation of conventional cigarettes | Reduced disease risk for current smokers who completely switch to e-cigarettes |
| Slowing cessation by smokers due to nicotine addiction | Reduced disease morbidity for smokers with existing heart or lung disease who switch to e-cigarettes |
| Nicotine addiction in former smokers who begin to use e-cigarettes and possibly transition back to smoking | Potential for cessation of combustible products |
| Renormalization of nicotine use and smoking as acceptable | Fewer users of combustible products in the entire population |
| Future disease risks for youth who are exposed to nicotine | |
| Increasing the dual use of e-cigarettes with combustible products | |
| Serving as a "gateway" to the initiation of tobacco smoking | |
| Increased disease risk vs. complete cessation among those who use both e-cigarettes and combustible products | |
| Exposure to secondhand aerosol and lack of clean air |
Addiction and dependence
Psychological and physical dependence
Nicotine, a key ingredient[32] in most e-liquids,[33] is well-recognized as one of the most addictive substances, as addictive as heroin and cocaine.[34] Addiction is believed to be a disorder of experience-dependent brain plasticity.[35] The reinforcing effects of nicotine play a significant role in the beginning and continuing use of the drug.[36] First-time nicotine users develop a dependence about 32% of the time.[37] Chronic nicotine use involves both psychological and physical dependence.[38] Nicotine-containing e-cigarette aerosol induces addiction-related neurochemical, physiological and behavioral changes.[17]
Nicotine affects neurological, neuromuscular, cardiovascular, respiratory, immunological and gastrointestinal systems.[39] Neuroplasticity within the brain's reward system occurs as a result of long-term nicotine use, leading to nicotine dependence.[40] The neurophysiological activities that are the basis of nicotine dependence are intricate.[41] It includes genetic components, age, gender, and the environment.[41] Pre-existing cognitive and mood disorders may influence the development and maintenance of nicotine dependence.[42]
Nicotine addiction is a disorder which alters different neural systems such as dopaminergic, glutamatergic, GABAergic, serotoninergic, that take part in reacting to nicotine.[43] In 2015 the psychological and behavioral effects of e-cigarettes were studied using whole-body exposure to e-cigarette aerosol, followed by a series of biochemical and behavioral studies.[17] The results showed that nicotine-containing e-cigarette aerosol induces addiction-related neurochemical, physiological and behavioral changes.[17]
Long-term nicotine use affects a broad range of genes associated with neurotransmission, signal transduction, and synaptic architecture.[44] The most well-known hereditary influence related to nicotine dependence is a mutation at rs16969968 in the nicotinic acetylcholine receptor CHRNA5, resulting in an amino acid alteration from aspartic acid to asparagine.[45] The single-nucleotide polymorphisms (SNPs) rs6474413 and rs10958726 in CHRNB3 are highly correlated with nicotine dependence.[46] Many other known variants within the CHRNB3–CHRNA6 nicotinic acetylcholine receptors are also correlated with nicotine dependence in certain ethnic groups.[46] There is a relationship between CHRNA5-CHRNA3-CHRNB4 nicotinic acetylcholine receptors and complete smoking cessation.[47]
Increasing evidence indicates that the genetic variant CHRNA5 predicts the response to smoking cessation medicine.[47] The ability to quitting smoking is affected by genetic factors, including genetically based differences in the way nicotine is metabolized.[48] In the CYP450 system there are 173 genetic variants, which impacts how quickly nicotine is metabolizes by each individual.[49] The speed of metabolism impacts the regularity and quantity of nicotine used.[49] For instance, in people who metabolize nicotine gradually their central nervous system effects of nicotine lasts longer, increasing their probability of dependence, but also increasing ability with quitting smoking.[49]
Stimulation of the brain
How does the nicotine in e-cigarettes affect the brain?[6] Until about age 25, the brain is still growing.[6] Each time a new memory is created or a new skill is learned, stronger connections – or synapses – are built between brain cells.[6] Young people's brains build synapses faster than adult brains.[6] Because addiction is a form of learning, adolescents can get addicted more easily than adults.[6] The nicotine in e-cigarettes and other tobacco products can also prime the adolescent brain for addiction to other drugs such as cocaine.[51]
Nicotine is a parasympathomimetic stimulant[8] that binds to and activates nicotinic acetylcholine receptors in the brain,[9] which subsequently causes the release of dopamine and other neurotransmitters, such as norepinephrine, acetylcholine, serotonin, gamma-aminobutyric acid, glutamate, endorphins,[10] and several neuropeptides, including proopiomelanocortin-derived α-MSH and adrenocorticotropic hormone.[52] Corticotropin-releasing factor, Neuropeptide Y, orexins, and norepinephrine are involved in nicotine addiction.[53]
Continuous exposure to nicotine can cause an increase in the number of nicotinic receptors, which is believed to be a result of receptor desensitization and subsequent receptor upregulation.[10] Long-term exposure to nicotine can also result in downregulation of glutamate transporter 1.[54] Long-term nicotine exposure upregulates cortical nicotinic receptors, but it also lowers the activity of the nicotinic receptors in the cortical vasodilation region.[55] These effects are not easily understood.[55]
With constant use of nicotine, tolerance occurs at least partially as a result of the development of new nicotinic acetylcholine receptors in the brain.[10] After several months of nicotine abstinence, the number of receptors go back to normal.[9] The extent to which alterations in the brain caused by nicotine use are reversible is not fully understood.[44] Nicotine also stimulates nicotinic acetylcholine receptors in the adrenal medulla, resulting in increased levels of epinephrine and beta-endorphin.[10] Its physiological effects stem from the stimulation of nicotinic acetylcholine receptors, which are located throughout the central and peripheral nervous systems.[56]
The α4β2 nicotinic receptor subtype is the main nicotinic receptor subtype.[57] Nicotine activates brain receptors which produce sedative as well as pleasurable effects.[58] Chronic nicotinic acetylcholine receptor activation from repeated nicotine exposure can induce strong effects on the brain, including changes in the brain's physiology, that result from the stimulation of regions of the brain associated with reward, pleasure, and anxiety.[59] These complex effects of nicotine on the brain are still not well understood.[59]
Nicotine interferes with the blood–brain barrier function, and as a consequence raises the risk of brain edema and neuroinflammation.[11] When nicotine enters the brain it stimulates, among other activities, the midbrain dopaminergic neurons situated in the ventral tegmental area and pars compacta.[12] It induces the release of dopamine in different parts of the brain, such as the nucleus accumbens, amygdala, and hippocampus.[12] Ghrelin-induced dopamine release occurs as a result of the activation of the cholinergic–dopaminergic reward link in the ventral tegmental area, a critical part of the reward areas in the brain related with reinforcement.[60] Ghrelin signaling may affect the reinforcing effects of drug dependence.[60]
Discontinuing nicotine use
When nicotine intake stops, the upregulated nicotinic acetylcholine receptors induce withdrawal symptoms.[9] These symptoms can include cravings for nicotine, anger, irritability, anxiety, depression, impatience, trouble sleeping, restlessness, hunger, weight gain, and difficulty concentrating.[61] When trying to quit smoking with vaping a base containing nicotine, symptoms of withdrawal can include irritability, restlessness, poor concentration, anxiety, depression, and hunger.[62] The changes in the brain cause a nicotine user to feel abnormal when not using nicotine.[63] In order to feel normal, the user has to keep his or her body supplied with nicotine.[63] E-cigarettes may reduce cigarette craving and withdrawal symptoms.[64]
Limiting tobacco consumption with the use of campaigns that portray cigarette smoking as unacceptable and harmful have been enacted; though, advocating for the use of e-cigarettes jeopardizes this because of the possibility of escalating nicotine addiction.[65] It is not clear whether e-cigarette use will decrease or increase overall nicotine addiction,[66] but the nicotine content in e-cigarettes is adequate to sustain nicotine dependence.[67] Chronic nicotine use causes a broad range of neuroplastic adaptations, making quitting hard to accomplish.[41]
A 2015 study found that users vaping non-nicotine e-liquid exhibited signs of dependence.[68] Experienced users tend to take longer puffs which may result in higher nicotine intake.[69] It is difficult to assess the impact of nicotine dependence from e-cigarette use because of the wide range of e-cigarette products.[67] The addiction potential of e-cigarettes may have risen because as they have progressed, they delivery nicotine better.[70] A 2016 review states that "The highly addictive nature of nicotine is responsible for its widespread use and difficulty with quitting."[7]
Young adults and youth
Addiction and dependence
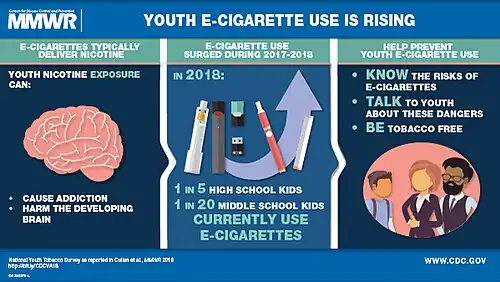
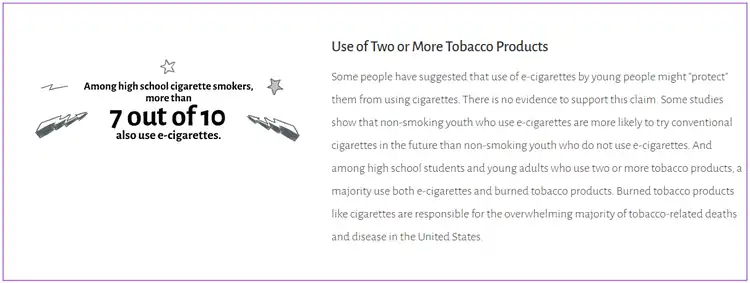
E-cigarettes use by children and adolescents may result in nicotine addiction.[73]: C [74]: A Following the possibility of nicotine addiction via e-cigarettes, there is concern that children may start smoking cigarettes.[75] Adolescents are likely to underestimate nicotine's addictiveness.[76] Vulnerability to the brain-modifying effects of nicotine, along with youthful experimentation with e-cigarettes, could lead to a lifelong addiction.[77] A long-term nicotine addiction from using a vape may result in using other tobacco products.[78]
The majority of addiction to nicotine starts during youth and young adulthood.[79] Adolescents are more likely to become nicotine dependent than adults.[80] The adolescent brain seems to be particularly sensitive to neuroplasticity as a result of nicotine.[44] Minimal exposure could be enough to produce neuroplastic alterations in the very sensitive adolescent brain.[44] Exposure to nicotine during adolescence may increase vulnerability to getting addicted to cocaine and other drugs.[81]
The ability of e-cigarettes to deliver comparable or higher amounts of nicotine compared to traditional cigarettes raises concerns about e-cigarette use generating nicotine dependence among young people.[82] Youth who believe they are vaping without nicotine could still be inhaling nicotine because there are significant differences between declared and true nicotine content.[83]
A 2016 US Surgeon General report concluded that e-cigarette use among young adults and youths is of public health concern.[71] Various organizations,[84] including the International Union Against Tuberculosis and Lung Disease, the American Academy of Pediatrics, the American Cancer Society, the Centers for Disease Control and Prevention, and the US Food and Drug Administration (US FDA), have expressed concern that e-cigarette use could increase the prevalence of nicotine addiction in youth.[85]: IUATLD [86]: AAP [87]: ACS [79]: CDC [88]: US FDA
Flavored tobacco is especially enticing to youth, and certain flavored tobacco products increase addiction.[14] There is concern that flavored e-cigarettes could have a similar impact on youth.[14] The extent to which teens are using e-cigarettes may lead to addiction or substance dependence in youth, is unknown.[89] A 2017 review noted that "adolescents experience symptoms of dependence at lower levels of nicotine exposure than adults. Consequently, it is harder to reverse addiction originating in this stage compared with later in life."[90]
Adolescents are particularly susceptible to nicotine addiction: the majority (90%) of smokers start before the age of 18, a fact that has been utilized by tobacco companies for decades in their teen-targeted advertising, marketing and even product design.[34] E-cigarette marketing tactics have the possibility to glamorize smoking and enticing children and never smokers, even when such outcomes are unintended.[91] Adolescents may show signs of dependence with even infrequent nicotine use; sustained nicotine exposure leads to upregulation of the receptors in the prefrontal cortex, pathways which are involved in cognitive control, and which are not fully matured until the mid-twenties.[34] Such disruption of neural circuit development may lead to long-term cognitive and behavioral impairment and has been associated with depression and anxiety.[34]
The nicotine content in e-cigarettes varies widely by product and by use.[34] Refill solutions may contain anywhere from 1.8% nicotine (18 mg/mL) to over 5% (59 mg/mL).[34] Nicotine delivery may be affected by the device itself, for example, by increasing the voltage which changes the aerosol delivered, or by "dripping"—a process of inhaling liquid poured directly onto coils.[34] The latest generation of e-cigarettes, "pod products," such as Juul, have the highest nicotine content (59 mg/mL), in protonated salt, rather than the free-base nicotine form found in earlier generations, which makes it easier for less experienced users to inhale.[34] Despite the clear presence of nicotine in e-cigarettes, adolescents often do not recognize this fact, potentially fueling misperceptions about the health risks and addictive potential of e-cigarettes.[34]
In the US, the unprecedented increase in current (past-month) users from 11.7% of high school students in 2017 to 20.8% in 2018 would imply dependence, if not addiction, given what we know about nicotine and its effects on the adolescent brain.[34] Two recent studies in 2018 utilized validated measures to identify nicotine dependence in e-cigarette using adolescents.[34] Exposure to nicotine from certain types of e-cigarettes may be higher than that from traditional cigarettes.[34] For example, in a study in 2018 of adolescent pod users, their urinary cotinine (a breakdown product used to measure nicotine exposure) levels were higher than levels seen in adolescent cigarette smokers.[34]
Effects on the brain
Both preadolescence and adolescence are developmental periods associated with increased vulnerability to nicotine addiction, and exposure to nicotine during these periods may lead to long-lasting changes in behavioral and neuronal plasticity.[93] Nicotine has more significant and durable damaging effects on adolescent brains compared to adult brains, the former suffering more harmful effects.[94] Preclinical animal studies have shown that in rodent models, nicotinic acetylcholine receptor signaling is still actively changing during adolescence, with higher expression and functional activity of nicotinic acetylcholine receptors in the forebrain of adolescent rodents compared to their adult counterparts.[94]
In rodent models, nicotine actually enhances neuronal activity in several reward-related regions and does so more robustly in adolescents than in adults.[94] This increased sensitivity to nicotine in the reward pathways of adolescent rats is associated with enhanced behavioral responses, such as strengthening the stimulus response reward for administration of nicotine.[94] In conditioned place-preference tests—where reward is measured by the amount of time animals spend in an environment where they receive nicotine compared to an environment where nicotine is not administered—adolescent rodents have shown an increased sensitivity to the rewarding effects of nicotine at very low doses (0.03 mg/kg) and exhibited a unique vulnerability to oral self-administration during the early-adolescent period.[94]
Adolescent rodents also have shown higher levels of nicotine self-administration than adults, decreased sensitivity to the aversive effects of nicotine, and less prominent withdrawal symptoms following chronic nicotine exposure.[94] This characteristic in rodent models of increased positive and decreased negative short-term effects of nicotine during adolescence (versus adulthood) highlights the possibility that human adolescents might be particularly vulnerable to developing dependency to and continuing to use e-cigarettes.[94]
The teen years are critical for brain development, which continues into young adulthood.[30] Young people who use nicotine products in any form, including e-cigarettes, are uniquely at risk for long-lasting effects.[30] Because nicotine affects the development of the brain's reward system, continued e-cigarette use can not only lead to nicotine addiction, but it also can make other drugs such as cocaine and methamphetamine more pleasurable to a teen's developing brain.[30] Concerns exist in respect to adolescence vaping due to studies indicating nicotine may potentially have harmful effects on the brain.[95] Nicotine exposure during adolescence adversely affects cognitive development.[1]
Children are more sensitive to nicotine than adults.[77] The use of products containing nicotine in any form among youth, including in e-cigarettes, is unsafe.[28] Animal research indicates strong evidence that the limbic system, which modulates drug reward, cognition, and emotion, is growing during adolescence and is particularly vulnerable to the long lasting effects of nicotine.[3] In youth, nicotine is associated with cognitive impairment[3] as well as the chance of getting addicted for life.[96]
The adolescent's developing brain is especially sensitive to the harmful effects of nicotine.[97] A short period of regular or occasional nicotine exposure in adolescence exerts long-term neurobehavioral damage.[97] Risks of exposing the developing brain to nicotine include mood disorders and permanent lowering of impulse control.[6] The rise in vaping is of great concern because the parts encompassing in greater cognitive activities including the prefrontal cortex of the brain continues to develop into the 20s.[1] Nicotine exposure during brain development may hamper growth of neurons and brain circuits, effecting brain architecture, chemistry, and neurobehavioral activity.[1]
Nicotine changes the way synapses are formed, which can harm the parts of the brain that control attention and learning.[6] Preclinical studies indicate that teens being exposed to nicotine interferes with the structural development of the brain, inducing lasting alterations in the brain's neural circuits.[98] Nicotine affects the development of brain circuits that control attention and learning.[30] Other risks include mood disorders and permanent problems with impulse control—failure to fight an urge or impulse that may harm oneself or others.[30] Each e-cigarette brand differs in the exact amount of ingredients and nicotine in each product.[98] Therefore, little is known regarding the health consequences of each brand to the growing brains of youth.[98]
E-cigarettes are a source of potential developmental toxicants.[99] E-cigarette aerosol, e-liquids, flavoring, and the metallic coil can cause oxidative stress, and the growing brain is uniquely susceptible to the detrimental effects of oxidative stress.[100] As indicated in the limited research from animal studies, there is the potential for induced changes in neurocognitive growth among children who have been subjected to e-cigarette aerosols consisting of nicotine.[29] The US FDA stated in 2019 that some people who use e-cigarettes have experienced seizures, with most reports involving youth or young adult users.[101] Inhaling lead from e-cigarette aerosol can induce serious neurologic injury, notably to the growing brains of children.[102]
A 2017 review states that "Because the brain does not reach full maturity until the mid-20s, restricting sales of electronic cigarettes and all tobacco products to individuals aged at least 21 years and older could have positive health benefits for adolescents and young adults."[90] Adverse effects to the health of children is mostly not known.[103] Children subjected to e-cigarettes had a higher likelihood of having more than one adverse effect and effects were more significant, than with children subjected to traditional cigarettes.[103] Significant harmful effects were cyanosis, nausea, and coma, among others.[103]
Effects of nicotine on fetal development diagram
Possible effects of nicotine on the developing human fetal brain
Nicotine exposure during pregnancy can harm fetal brain development.[14]
|
Fetal development
There is accumulating research concerning the negative effects of nicotine on prenatal brain development.[notes 5][110] Vaping during pregnancy can be harmful to the fetus.[111] There is no supporting evidence demonstrating that vaping is safe for use in pregnant women.[104] Nicotine accumulates in the fetus because it goes through the placenta.[112] Nicotine has been found in placental tissue as early as seven weeks of embryonic gestation, and nicotine concentrations are higher in fetal fluids than in maternal fluids.[15] Nicotine can lead to vasoconstriction of uteroplacental vessels, reducing the delivery of both nutrients and oxygen to the fetus.[113]
As a result, nutrition is re-distributed to prioritize vital organs, such as the heart and the brain, at the cost of less vital organs, such as the liver, kidneys, adrenal glands, and pancreas, leading to underdevelopment and functional disorders later in life.[113] Nicotine attaches to nicotinic acetylcholine receptors in the fetus brain.[90] The stage when the human brain is developing is possibly the most sensitive time period to the effects of nicotine.[104] When the brain is being developed, activating or desensitizing nicotinic acetylcholine receptors by being exposed to nicotine can result in long-term developmental disturbances.[90]
Prenatal nicotine exposure has been associated with dysregulation of catecholaminergic, serotonergic, and other neurotransmitter systems.[15] Prenatal nicotine exposure is associated with preterm birth,[76] stillbirth,[76] sudden infant death syndrome,[104] auditory processing complications, changes to the corpus callosum,[105] changes in brain metabolism,[106] changes in neurological systems,[104] changes in neurotransmitter systems,[106] changes in normal brain development, lower birth weights compared to other infants,[104] and a reduction in brain weight.[108]
A 2017 review states, "because nicotine targets the fetal brain, damage can be present, even when birth weight is normal."[90] A 2014 US Surgeon General report found "that nicotine adversely affects maternal and fetal health during pregnancy, and that exposure to nicotine during fetal development has lasting adverse consequences for brain development."[14] Nicotine prenatal exposure is associated with behavioral abnormalities in adults and children.[107] Prenatal nicotine exposure may result in persisting, multigenerational changes in the epigenome.[3]
.svg.png.webp)
Effects of e-cigarette liquid
E-liquid exposure whether intentional or unintentional from ingestion, eye contact, or skin contact can cause adverse effects such as seizures and anoxic brain trauma.[16] The nicotine in e-liquids readily absorbs into the bloodstream when a person uses an e-cigarette.[30] Upon entering the blood, nicotine stimulates the adrenal glands to release the hormone epinephrine.[30] Epinephrine stimulates the central nervous system and increases blood pressure, breathing, and heart rate.[30]
As with most addictive substances, nicotine increases levels of a chemical messenger in the brain called dopamine, which affects parts of the brain that control reward (pleasure from natural behaviors such as eating).[30] These feelings motivate some people to use nicotine again and again, despite possible risks to their health and well-being.[30]
A 2015 study on the offspring of the pregnant mice, which were exposed to nicotine-containing e-liquid, showed significant behavioral alterations.[17] This indicated that exposure to e-cigarette components in a susceptible time period of brain development could induce persistent behavioral changes.[17] E-cigarette aerosols without containing nicotine could harm the growing conceptus.[115] This indicates that the ingredients in the e-liquid, such as the flavors, could be developmental toxicants.[115]
Gallery
- E-cigarette related videos
- Robbing the Future - Advertising Aimed at Children.
- E-cigarettes - An Emerging Public Health Challenge.
- Tobacco Use By Youth Is Rising – February 2019 – Vital Signs.
- Nicotine & Vaping - Don't Get Hacked - The Real Cost.
- Julius Dein Doing A Magic Trick on A Vape - The Real Cost.
Notes
- From prenatal development through adolescence and early adulthood, exposure to nicotine poses a serious threat, because these are critical times for brain development and brain plasticity.[2] Furthermore, youth and young adults are more vulnerable than adults to the long-term consequences of nicotine exposure, including susceptibility to nicotine addiction and potentially reduced impulse control, deficits in attention and cognition, and mood disorders.[2]
- A 2018 review found "Nicotine is the third most commonly used substance by adolescents and use of electronic cigarettes has become twice as popular as traditional tobacco products. Concomitantly, e-cigarettes have been found to increase the risk for transitioning to more traditional tobacco cigarettes. Although acute administration of nicotine may enhance cognition in teens and young adults, especially memory and attention, chronic use has been linked with attention and working memory deficits in teens. Acute withdrawal from nicotine in adolescent users has also been associated with abnormal reward processing, working memory, and verbal memory fMRI tasks, highlighting the necessity to measure last use of nicotine prior to neurocognitive assessment."[4]
- Studies of the effects of maternal smoking of conventional cigarettes during pregnancy, coupled with preclinical literature examining the effects of maternal self-administration of nicotine during pregnancy, suggest that e-cigarette use by mothers during pregnancy presents a wide variety of risks to fetal, infant, and child brain development.[13]
- The long-term health risks of e-cigarettes will not be known for decades, although evidence to date suggests that they are generally less harmful than combustible tobacco products.[31] However, less harmful is not the same as harmless.[31] A substantial amount of evidence is available on some components of the e-cigarette aerosols inhaled by e-cigarette users.[31] For many people, exposure to e-cigarette aerosol could occur across much of the life span, beginning in adolescence and even in childhood, when the lungs and brain are still developing.[31]
- Fetal exposure to nicotine during pregnancy can result in multiple adverse consequences, including sudden infant death syndrome, altered corpus callosum, auditory processing deficits, effects on behaviors and obesity, and deficits in attention and cognition.[109]
Bibliography
- McNeill, A; Brose, LS; Calder, R; Bauld, L; Robson, D (February 2018). "Evidence review of e-cigarettes and heated tobacco products 2018" (PDF). UK: Public Health England. pp. 1–243.
- Stratton, Kathleen; Kwan, Leslie Y.; Eaton, David L. (January 2018). Public Health Consequences of E-Cigarettes (PDF). National Academies of Sciences, Engineering, and Medicine. National Academies Press. pp. 1–774. doi:10.17226/24952. ISBN 978-0-309-46834-3. PMID 29894118.
- "E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General" (PDF). United States Department of Health and Human Services. Surgeon General of the United States. 2016. pp. 1–298.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "State Health Officer's Report on E-Cigarettes: A Community Health Threat" (PDF). California Tobacco Control Program. California Department of Public Health. January 2015. pp. 1–21.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Electronic nicotine delivery systems" (PDF). World Health Organization. 21 July 2014. pp. 1–13.
- National Center for Chronic Disease Prevention Health Promotion (US) Office on Smoking Health (2014). The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Surgeon General of the United States. pp. 1–943. PMID 24455788.
References
- England, Lucinda J.; Bunnell, Rebecca E.; Pechacek, Terry F.; Tong, Van T.; McAfee, Tim A. (2015). "Nicotine and the Developing Human". American Journal of Preventive Medicine. 49 (2): 286–93. doi:10.1016/j.amepre.2015.01.015. ISSN 0749-3797. PMC 4594223. PMID 25794473.
- SGUS 2016, p. 113; Chapter 3.
- Yuan, Menglu; Cross, Sarah J.; Loughlin, Sandra E.; Leslie, Frances M. (2015). "Nicotine and the adolescent brain". The Journal of Physiology. 593 (16): 3397–3412. doi:10.1113/JP270492. ISSN 0022-3751. PMC 4560573. PMID 26018031.
- Lisdahl, Krista M.; Sher, Kenneth J.; Conway, Kevin P.; Gonzalez, Raul; Feldstein Ewing, Sarah W.; Nixon, Sara Jo; Tapert, Susan; Bartsch, Hauke; Goldstein, Rita Z.; Heitzeg, Mary (2018). "Adolescent brain cognitive development (ABCD) study: Overview of substance use assessment methods". Developmental Cognitive Neuroscience. 32: 80–96. doi:10.1016/j.dcn.2018.02.007. ISSN 1878-9293. PMC 6375310. PMID 29559216.
- "Youth and Tobacco". United States Food and Drug Administration. 24 June 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Know the Risks". Surgeon General of the United States. 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Siqueira, Lorena M. (2016). "Nicotine and Tobacco as Substances of Abuse in Children and Adolescents". Pediatrics. 139 (1): e20163436. doi:10.1542/peds.2016-3436. ISSN 0031-4005. PMID 27994114. S2CID 2451568.
- Richard Beebe; Jeff Myers (19 July 2012). Professional Paramedic, Volume I: Foundations of Paramedic Care. Cengage Learning. pp. 640–. ISBN 978-1-133-71465-1.
- Bullen, Christopher (2014). "Electronic Cigarettes for Smoking Cessation". Current Cardiology Reports. 16 (11): 538. doi:10.1007/s11886-014-0538-8. ISSN 1523-3782. PMID 25303892. S2CID 2550483.
- Drug Therapeutics, Bulletin (2014). "Republished: Nicotine and health". BMJ. 349 (nov26 9): 2014.7.0264rep. doi:10.1136/bmj.2014.7.0264rep. ISSN 1756-1833. PMID 25428425. S2CID 45426626.
- Sajja, Ravi K; Rahman, Shafiqur; Cucullo, Luca (2016). "Drugs of abuse and blood–brain barrier endothelial dysfunction: A focus on the role of oxidative stress". Journal of Cerebral Blood Flow & Metabolism. 36 (3): 539–54. doi:10.1177/0271678X15616978. ISSN 0271-678X. PMC 4794105. PMID 26661236.
- Subramaniyan, Manivannan; Dani, John A. (2015). "Dopaminergic and cholinergic learning mechanisms in nicotine addiction". Annals of the New York Academy of Sciences. 1349 (1): 46–63. Bibcode:2015NYASA1349...46S. doi:10.1111/nyas.12871. ISSN 0077-8923. PMC 4564314. PMID 26301866.
- SGUS 2016, p. 124; Chapter 3.
- Brandon, T. H.; Goniewicz, M. L.; Hanna, N. H.; Hatsukami, D. K.; Herbst, R. S.; Hobin, J. A.; Ostroff, J. S.; Shields, P. G.; Toll, B. A.; Tyne, C. A.; Viswanath, K.; Warren, G. W. (2015). "Electronic Nicotine Delivery Systems: A Policy Statement from the American Association for Cancer Research and the American Society of Clinical Oncology". Clinical Cancer Research. 21 (3): 514–525. doi:10.1158/1078-0432.CCR-14-2544. ISSN 1078-0432. PMID 25573384. S2CID 34471339.
- SGUS 2016, p. 108; Chapter 3.
- Stratton 2018, p. Summary, Conclusion 14-2.; 9.
- Hiemstra, Pieter S.; Bals, Robert (2016). "Basic science of electronic cigarettes: assessment in cell culture and in vivo models". Respiratory Research. 17 (1): 127. doi:10.1186/s12931-016-0447-z. ISSN 1465-993X. PMC 5055681. PMID 27717371.
 This article incorporates text by Pieter S. Hiemstra and Robert Bals available under the CC BY 4.0 license.
This article incorporates text by Pieter S. Hiemstra and Robert Bals available under the CC BY 4.0 license. - Franck, Caroline; Filion, Kristian B.; Kimmelman, Jonathan; Grad, Roland; Eisenberg, Mark J. (2016). "Ethical considerations of e-cigarette use for tobacco harm reduction". Respiratory Research. 17 (1): 53. doi:10.1186/s12931-016-0370-3. ISSN 1465-993X. PMC 4869264. PMID 27184265.
 This article incorporates text by Caroline Franck, Kristian B. Filion, Jonathan Kimmelman, Roland Grad and Mark J. Eisenberg available under the CC BY 4.0 license.
This article incorporates text by Caroline Franck, Kristian B. Filion, Jonathan Kimmelman, Roland Grad and Mark J. Eisenberg available under the CC BY 4.0 license. - Golub, Justin S.; Samy, Ravi N. (2015). "Preventing or reducing smoking-related complications in otologic and neurotologic surgery". Current Opinion in Otolaryngology & Head and Neck Surgery. 23 (5): 334–340. doi:10.1097/MOO.0000000000000184. ISSN 1068-9508. PMID 26339963. S2CID 205830424.
- Toda, Noboru; Toda, Hiroshi (2010). "Nitric oxide-mediated blood flow regulation as affected by smoking and nicotine". European Journal of Pharmacology. 649 (1–3): 1–13. doi:10.1016/j.ejphar.2010.09.042. ISSN 0014-2999. PMID 20868673.
- SA, Meo; SA, Al Asiri (2014). "Effects of electronic cigarette smoking on human health" (PDF). Eur Rev Med Pharmacol Sci. 18 (21): 3315–9. PMID 25487945.
- Machaalani, Rita; Chen, Hui (2018). "Brain derived neurotrophic factor (BDNF), its tyrosine kinase receptor B (TrkB) and nicotine". NeuroToxicology. 65: 186–195. doi:10.1016/j.neuro.2018.02.014. hdl:10453/122789. ISSN 0161-813X. PMID 29499216. S2CID 3688206.
- "Nicotine Side Effects". Drugs.com. 21 January 2019.
- Schraufnagel, Dean E.; Blasi, Francesco; Drummond, M. Bradley; Lam, David C. L.; Latif, Ehsan; Rosen, Mark J.; Sansores, Raul; Van Zyl-Smit, Richard (2014). "Electronic Cigarettes. A Position Statement of the Forum of International Respiratory Societies". American Journal of Respiratory and Critical Care Medicine. 190 (6): 611–618. doi:10.1164/rccm.201407-1198PP. ISSN 1073-449X. PMID 25006874. S2CID 43763340.
- Kandel, Denise; Kandel, Eric (2015). "The Gateway Hypothesis of substance abuse: developmental, biological and societal perspectives". Acta Paediatrica. 104 (2): 130–137. doi:10.1111/apa.12851. ISSN 0803-5253. PMID 25377988. S2CID 33575141.
- Garcia, Alexandra N.; Salloum, Ihsan M. (2015). "Polysomnographic sleep disturbances in nicotine, caffeine, alcohol, cocaine, opioid, and cannabis use: A focused review". The American Journal on Addictions. 24 (7): 590–598. doi:10.1111/ajad.12291. ISSN 1055-0496. PMID 26346395.
- Irish, Leah A.; Kline, Christopher E.; Gunn, Heather E.; Buysse, Daniel J.; Hall, Martica H. (2015). "The role of sleep hygiene in promoting public health: A review of empirical evidence". Sleep Medicine Reviews. 22: 23–36. doi:10.1016/j.smrv.2014.10.001. ISSN 1087-0792. PMC 4400203. PMID 25454674.
- SGUS 2016, p. 5; Chapter 1.
- Collaco, Joseph M.; McGrath-Morrow, Sharon A. (2018). "Electronic Cigarettes: Exposure and Use Among Pediatric Populations". Journal of Aerosol Medicine and Pulmonary Drug Delivery. 31 (2): 71–77. doi:10.1089/jamp.2017.1418. ISSN 1941-2711. PMC 5915214. PMID 29068754.
- "Electronic Cigarettes (E-cigarettes)". National Institute on Drug Abuse. March 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - SGUS 2016, p. 186; Chapter 5.
- Kaisar, Mohammad Abul; Prasad, Shikha; Liles, Tylor; Cucullo, Luca (2016). "A Decade of e-Cigarettes: Limited Research & Unresolved Safety Concerns". Toxicology. 365: 67–75. doi:10.1016/j.tox.2016.07.020. ISSN 0300-483X. PMC 4993660. PMID 27477296.
- Weaver, Michael; Breland, Alison; Spindle, Tory; Eissenberg, Thomas (2014). "Electronic Cigarettes". Journal of Addiction Medicine. 8 (4): 234–240. doi:10.1097/ADM.0000000000000043. ISSN 1932-0620. PMC 4123220. PMID 25089953.
- Jenssen, Brian P.; Boykan, Rachel (2019). "Electronic Cigarettes and Youth in the United States: A Call to Action (at the Local, National and Global Levels)". Children. 6 (2): 30. doi:10.3390/children6020030. ISSN 2227-9067. PMC 6406299. PMID 30791645.
 This article incorporates text by Brian P. Jenssen and Rachel Boykan available under the CC BY 4.0 license.
This article incorporates text by Brian P. Jenssen and Rachel Boykan available under the CC BY 4.0 license. - Kenny, PJ (September 2014). "Genetics of Substance Use Disorders". Dialogues Clin Neurosci. 16 (3): 335–344. doi:10.31887/DCNS.2014.16.3/pkenny. PMC 4214176. PMID 25364284.
- D'Souza, Manoranjan S. (2015). "Glutamatergic transmission in drug reward: implications for drug addiction". Frontiers in Neuroscience. 9: 404. doi:10.3389/fnins.2015.00404. ISSN 1662-453X. PMC 4633516. PMID 26594139.
- MacDonald, K; Pappa, K (April 2016). "WHY NOT POT?: A Review of the Brain-based Risks of Cannabis". Innov Clin Neurosci. 13 (3–4): 13–22. PMC 4911936. PMID 27354924.
- Kishioka, Shiroh; Kiguchi, Norikazu; Kobayashi, Yuka; Saika, Fumihiro (2014). "Nicotine Effects and the Endogenous Opioid System". Journal of Pharmacological Sciences. 125 (2): 117–124. doi:10.1254/jphs.14R03CP. ISSN 1347-8613. PMID 24882143.
- Lee, Peter N.; Fariss, Marc W. (2016). "A systematic review of possible serious adverse health effects of nicotine replacement therapy". Archives of Toxicology. 91 (4): 1565–1594. doi:10.1007/s00204-016-1856-y. ISSN 0340-5761. PMC 5364244. PMID 27699443.
- D'Souza MS, Markou A (2011). "Neuronal mechanisms underlying development of nicotine dependence: implications for novel smoking-cessation treatments". Addict Sci Clin Pract. 6 (1): 4–16. PMC 3188825. PMID 22003417.
- Jackson, K.J.; Muldoon, P.P.; De Biasi, M.; Damaj, M.I. (2015). "New mechanisms and perspectives in nicotine withdrawal". Neuropharmacology. 96 (Pt B): 223–234. doi:10.1016/j.neuropharm.2014.11.009. ISSN 0028-3908. PMC 4444410. PMID 25433149.
- Besson, Morgane; Forget, Benoît (2016). "Cognitive Dysfunction, Affective States, and Vulnerability to Nicotine Addiction: A Multifactorial Perspective". Frontiers in Psychiatry. 7: 160. doi:10.3389/fpsyt.2016.00160. ISSN 1664-0640. PMC 5030478. PMID 27708591.
 This article incorporates text by Morgane Besson and Benoît Forget available under the CC BY 4.0 license.
This article incorporates text by Morgane Besson and Benoît Forget available under the CC BY 4.0 license. - Hadjiconstantinou, Maria; Neff, Norton H. (2011). "Nicotine and endogenous opioids: Neurochemical and pharmacological evidence". Neuropharmacology. 60 (7–8): 1209–1220. doi:10.1016/j.neuropharm.2010.11.010. ISSN 0028-3908. PMID 21108953. S2CID 45539554.
- Korpi, E. R.; den Hollander, B.; Farooq, U.; Vashchinkina, E.; Rajkumar, R.; Nutt, D. J.; Hyytia, P.; Dawe, G. S. (2015). "Mechanisms of Action and Persistent Neuroplasticity by Drugs of Abuse". Pharmacological Reviews. 67 (4): 872–1004. doi:10.1124/pr.115.010967. ISSN 1521-0081. PMID 26403687. S2CID 24802846.
- Yu, Cassie; McClellan, Jon (2016). "Genetics of Substance Use Disorders". Child and Adolescent Psychiatric Clinics of North America. 25 (3): 377–385. doi:10.1016/j.chc.2016.02.002. ISSN 1056-4993. PMID 27338962.
- Wen, L; Yang, Z; Cui, W; Li, M D (2016). "Crucial roles of the CHRNB3–CHRNA6 gene cluster on chromosome 8 in nicotine dependence: update and subjects for future research". Translational Psychiatry. 6 (6): e843. doi:10.1038/tp.2016.103. ISSN 2158-3188. PMC 4931601. PMID 27327258.
- Chen, Li-Shiun; Horton, Amy; Bierut, Laura (2016). "Pathways to precision medicine in smoking cessation treatments". Neuroscience Letters. 669: 83–92. doi:10.1016/j.neulet.2016.05.033. ISSN 0304-3940. PMC 5115988. PMID 27208830.
- Chenoweth, Meghan J.; Tyndale, Rachel F. (2017). "Pharmacogenetic Optimization of Smoking Cessation Treatment". Trends in Pharmacological Sciences. 38 (1): 55–66. doi:10.1016/j.tips.2016.09.006. ISSN 0165-6147. PMC 5195866. PMID 27712845.
- Baraona, L. Kim; Lovelace, Dawn; Daniels, Julie L.; McDaniel, Linda (2017). "Tobacco Harms, Nicotine Pharmacology, and Pharmacologic Tobacco Cessation Interventions for Women". Journal of Midwifery & Women's Health. 62 (3): 253–269. doi:10.1111/jmwh.12616. ISSN 1526-9523. PMID 28556464. S2CID 1267977.
- Di Matteo, Vincenzo; Pierucci, Massimo; Di Giovanni, Giuseppe; Benigno, Arcangelo; Esposito, Ennio (2007). "The Neurobiological Bases for the Pharmacotherapy of Nicotine Addiction". Current Pharmaceutical Design. 13 (12): 1269–1284. doi:10.2174/138161207780618920. ISSN 1381-6128. PMID 17504235.
- "Know The Risks: E-Cigarettes & Young People – Addiction". Surgeon General of the United States. 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Atta-ur- Rahman; Allen B. Reitz (1 January 2005). Frontiers in Medicinal Chemistry. Bentham Science Publishers. pp. 279–. ISBN 978-1-60805-205-9.
- Bruijnzeel, Adrie W. (2012). "Tobacco addiction and the dysregulation of brain stress systems". Neuroscience & Biobehavioral Reviews. 36 (5): 1418–1441. doi:10.1016/j.neubiorev.2012.02.015. ISSN 0149-7634. PMC 3340450. PMID 22405889.
- Alasmari, Fawaz; Al-Rejaie, Salim S.; AlSharari, Shakir D.; Sari, Youssef (2016). "Targeting glutamate homeostasis for potential treatment of nicotine dependence". Brain Research Bulletin. 121: 1–8. doi:10.1016/j.brainresbull.2015.11.010. ISSN 0361-9230. PMC 4783195. PMID 26589642.
- Uchida, Sae; Hotta, Harumi (2009). "Cerebral Cortical Vasodilatation Mediated by Nicotinic Cholinergic Receptors: Effects of Old Age and of Chronic Nicotine Exposure". Biological & Pharmaceutical Bulletin. 32 (3): 341–344. doi:10.1248/bpb.32.341. ISSN 0918-6158. PMID 19252275.
- SGUS 2014, p. 111.
- Dineley, Kelly T.; Pandya, Anshul A.; Yakel, Jerrel L. (2015). "Nicotinic ACh receptors as therapeutic targets in CNS disorders". Trends in Pharmacological Sciences. 36 (2): 96–108. doi:10.1016/j.tips.2014.12.002. ISSN 0165-6147. PMC 4324614. PMID 25639674.
- Caponnetto, P.; Russo, C.; Bruno, C.M.; Alamo, A.; Amaradio, M.D.; Polosa, R. (March 2013). "Electronic cigarette: a possible substitute for cigarette dependence". Monaldi Archives for Chest Disease. 79 (1): 12–19. doi:10.4081/monaldi.2013.104. ISSN 1122-0643. PMID 23741941.
- Rowell, Temperance R; Tarran, Robert (2015). "Will Chronic E-Cigarette Use Cause Lung Disease?". American Journal of Physiology. Lung Cellular and Molecular Physiology. 309 (12): L1398–409. doi:10.1152/ajplung.00272.2015. ISSN 1040-0605. PMC 4683316. PMID 26408554.
- Engel, Jörgen A.; Jerlhag, Elisabet (2014). "Role of Appetite-Regulating Peptides in the Pathophysiology of Addiction: Implications for Pharmacotherapy". CNS Drugs. 28 (10): 875–886. doi:10.1007/s40263-014-0178-y. ISSN 1172-7047. PMC 4181507. PMID 24958205.
- "Nicotine and Tobacco". A.D.A.M. Medical Encyclopedia. Medline Plus. 7 June 2016.
- Khoudigian, S.; Devji, T.; Lytvyn, L.; Campbell, K.; Hopkins, R.; O'Reilly, D. (29 January 2016). "The efficacy and short-term effects of electronic cigarettes as a method for smoking cessation: a systematic review and a meta-analysis". International Journal of Public Health. 61 (2): 257–267. doi:10.1007/s00038-016-0786-z. ISSN 1661-8556. PMID 26825455. S2CID 22227035.
- "Nicotine". National Institute on Drug Abuse. June 2007. Archived from the original on 2019-06-11. Retrieved 2019-09-07.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Shahab, Lion; Brose, Leonie S.; West, Robert (2013). "Novel Delivery Systems for Nicotine Replacement Therapy as an Aid to Smoking Cessation and for Harm Reduction: Rationale, and Evidence for Advantages over Existing Systems". CNS Drugs. 27 (12): 1007–1019. doi:10.1007/s40263-013-0116-4. ISSN 1172-7047. PMID 24114587. S2CID 207486096.
- Vanker, A.; Gie, R.P.; Zar, H.J. (2017). "The Association Between Environmental Tobacco Smoke Exposure and Childhood Respiratory Disease: A Review". Expert Review of Respiratory Medicine. 11 (8): 661–673. doi:10.1080/17476348.2017.1338949. ISSN 1747-6348. PMC 6176766. PMID 28580865.
- Palazzolo, Dominic L. (November 2013). "Electronic cigarettes and vaping: a new challenge in clinical medicine and public health. A literature review". Frontiers in Public Health. 1 (56): 56. doi:10.3389/fpubh.2013.00056. PMC 3859972. PMID 24350225.
- Schroeder, M. J.; Hoffman, A. C. (2014). "Electronic cigarettes and nicotine clinical pharmacology". Tobacco Control. 23 (Supplement 2): ii30–ii35. doi:10.1136/tobaccocontrol-2013-051469. ISSN 0964-4563. PMC 3995273. PMID 24732160.
- Bold, Krysten W.; Sussman, Steve; O'Malley, Stephanie S.; Grana, Rachel; Foulds, Jonathan; Fishbein, Howard; Krishnan-Sarin, Suchitra (2017). "Measuring E-cigarette dependence: Initial guidance". Addictive Behaviors. 79: 213–218. doi:10.1016/j.addbeh.2017.11.015. ISSN 0306-4603. PMC 5807200. PMID 29174664.
- Breland, Alison B.; Spindle, Tory; Weaver, Michael; Eissenberg, Thomas (2014). "Science and Electronic Cigarettes". Journal of Addiction Medicine. 8 (4): 223–233. doi:10.1097/ADM.0000000000000049. ISSN 1932-0620. PMC 4122311. PMID 25089952.
- McNeill 2018, p. 12.
- Cullen, Karen A.; Ambrose, Bridget K.; Gentzke, Andrea S.; Apelberg, Benjamin J.; Jamal, Ahmed; King, Brian A. (2018). "Notes from the Field: Use of Electronic Cigarettes and Any Tobacco Product Among Middle and High School Students — United States, 2011–2018". MMWR. Morbidity and Mortality Weekly Report. 67 (45): 1276–1277. doi:10.15585/mmwr.mm6745a5. ISSN 0149-2195. PMC 6290807. PMID 30439875.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "THE FACTS on e-cigarette use among youth and young adults". Surgeon General of the United States. 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Bhatnagar, A.; Whitsel, L. P.; Ribisl, K. M.; Bullen, C.; Chaloupka, F.; Piano, M. R.; Robertson, R. M.; McAuley, T.; Goff, D.; Benowitz, N. (24 August 2014). "Electronic Cigarettes: A Policy Statement From the American Heart Association". Circulation. 130 (16): 1418–1436. doi:10.1161/CIR.0000000000000107. PMC 7643636. PMID 25156991. S2CID 16075813.
- Hildick-Smith, Gordon J.; Pesko, Michael F.; Shearer, Lee; Hughes, Jenna M.; Chang, Jane; Loughlin, Gerald M.; Ipp, Lisa S. (2015). "A Practitioner's Guide to Electronic Cigarettes in the Adolescent Population". Journal of Adolescent Health. 57 (6): 574–9. doi:10.1016/j.jadohealth.2015.07.020. ISSN 1054-139X. PMID 26422289.
- WHO 2014, p. 6.
- Chapman 2015, p. 5.
- Schraufnagel DE (2015). "Electronic Cigarettes: Vulnerability of Youth". Pediatr Allergy Immunol Pulmonol. 28 (1): 2–6. doi:10.1089/ped.2015.0490. PMC 4359356. PMID 25830075.
- "Teens like different forms of tobacco and nicotine". American Cancer Society. Archived from the original on 20 September 2015.
- Singh, Tushar; Arrazola, René A.; Corey, Catherine G.; Husten, Corinne G.; Neff, Linda J.; Homa, David M.; King, Brian A. (2016). "Tobacco Use Among Middle and High School Students — United States, 2011–2015". MMWR. Morbidity and Mortality Weekly Report. 65 (14): 361–367. doi:10.15585/mmwr.mm6514a1. ISSN 0149-2195. PMID 27077789.
- Chatterjee, Kshitij; Alzghoul, Bashar; Innabi, Ayoub; Meena, Nikhil (2016). "Is vaping a gateway to smoking: a review of the longitudinal studies". International Journal of Adolescent Medicine and Health. 30 (3). doi:10.1515/ijamh-2016-0033. ISSN 2191-0278. PMID 27505084. S2CID 23977146.
- Dinakar, Chitra; Longo, Dan L.; O'Connor, George T. (2016). "The Health Effects of Electronic Cigarettes". New England Journal of Medicine. 375 (14): 1372–1381. doi:10.1056/NEJMra1502466. ISSN 0028-4793. PMID 27705269.
- SGUS 2016, p. 102; Chapter 3.
- Soneji, Samir; Barrington-Trimis, Jessica L.; Wills, Thomas A.; Leventhal, Adam M.; Unger, Jennifer B.; Gibson, Laura A.; Yang, JaeWon; Primack, Brian A.; Andrews, Judy A.; Miech, Richard A.; Spindle, Tory R.; Dick, Danielle M.; Eissenberg, Thomas; Hornik, Robert C.; Dang, Rui; Sargent, James D. (2017). "Association Between Initial Use of e-Cigarettes and Subsequent Cigarette Smoking Among Adolescents and Young Adults". JAMA Pediatrics. 171 (8): 788–797. doi:10.1001/jamapediatrics.2017.1488. ISSN 2168-6203. PMC 5656237. PMID 28654986.
- Kamat, Aarti D.; Van Dyke, Alison L. (2017). "Use of Electronic Nicotine Delivery Systems Among Adolescents: Status of the Evidence and Public Health Recommendations". Pediatric Annals. 46 (2): e69–e77. doi:10.3928/19382359-20170111-01. ISSN 1938-2359. PMID 28192582. S2CID 20909216.
- "Position Statement on Electronic Cigarettes [ECs] or Electronic Nicotine Delivery Systems [ENDS]" (PDF). The International Union against Tuberculosis and Lung Disease. October 2013. Archived from the original (PDF) on 2016-03-05. Retrieved 2019-09-07.
- Korioth, Trisha (4 October 2013). "E-cigarettes easy to buy, can hook kids on nicotine". AAP News: E131004-4. doi:10.1542/aapnews.20133411-24d (inactive 1 August 2023).
{{cite journal}}: CS1 maint: DOI inactive as of August 2023 (link) - Stacy Simon (17 April 2015). "E-Cigarette Use Triples Among Middle and High School Students". American Cancer Society.
- "FDA Warns of Health Risks Posed by E-Cigarettes". United States Food and Drug Administration. 17 September 2013. Reviewed 17 September 2013
- Durmowicz, E. L. (2014). "The impact of electronic cigarettes on the paediatric population". Tobacco Control. 23 (Supplement 2): ii41–ii46. doi:10.1136/tobaccocontrol-2013-051468. ISSN 0964-4563. PMC 3995262. PMID 24732163.
- England, Lucinda J.; Aagaard, Kjersti; Bloch, Michele; Conway, Kevin; Cosgrove, Kelly; Grana, Rachel; Gould, Thomas J.; Hatsukami, Dorothy; Jensen, Frances; Kandel, Denise; Lanphear, Bruce; Leslie, Frances; Pauly, James R.; Neiderhiser, Jenae; Rubinstein, Mark; Slotkin, Theodore A.; Spindel, Eliot; Stroud, Laura; Wakschlag, Lauren (2017). "Developmental toxicity of nicotine: A transdisciplinary synthesis and implications for emerging tobacco products". Neuroscience & Biobehavioral Reviews. 72: 176–189. doi:10.1016/j.neubiorev.2016.11.013. ISSN 0149-7634. PMC 5965681. PMID 27890689.
- WHO 2014, p. 9.
- "Know The Risks: E-Cigarettes & Young People – Use of Two or More Tobacco Products". Surgeon General of the United States. 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - SGUS 2016, p. 107; Chapter 3.
- SGUS 2016, p. 105; Chapter 3.
- Greenhill, Richard; Dawkins, Lynne; Notley, Caitlin; Finn, Mark D.; Turner, John J.D. (2016). "Adolescent Awareness and Use of Electronic Cigarettes: A Review of Emerging Trends and Findings". Journal of Adolescent Health. 59 (6): 612–619. doi:10.1016/j.jadohealth.2016.08.005. ISSN 1054-139X. PMID 27693128.
- "WHO Right to Call for E-Cigarette Regulation". World Lung Federation. 26 August 2014.
- Chapman 2015, p. 6.
- Modesto-Lowe, Vania; Alvarado, Camille (2017). "E-cigs . . . Are They Cool? Talking to Teens About E-Cigarettes". Clinical Pediatrics. 56 (10): 947–952. doi:10.1177/0009922817705188. ISSN 0009-9228. PMID 28443340. S2CID 44423931.
- Wolff, Mary S.; Buckley, Jessie P.; Engel, Stephanie M.; McConnell, Rob S.; Barr, Dana B. (2017). "Emerging exposures of developmental toxicants". Current Opinion in Pediatrics. 29 (2): 218–224. doi:10.1097/MOP.0000000000000455. ISSN 1040-8703. PMC 5473289. PMID 28059904.
- Tobore, Tobore Onojighofia (2019). "On the potential harmful effects of E-Cigarettes (EC) on the developing brain: The relationship between vaping-induced oxidative stress and adolescent/young adults social maladjustment". Journal of Adolescence. 76: 202–209. doi:10.1016/j.adolescence.2019.09.004. ISSN 0140-1971. PMID 31574388. S2CID 203640780.
- "Some E-cigarette Users Are Having Seizures, Most Reports Involving Youth and Young Adults". United States Food and Drug Administration. 3 April 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Smith, L; Brar, K; Srinivasan, K; Enja, M; Lippmann, S (June 2016). "E-cigarettes: How "safe" are they?". J Fam Pract. 65 (6): 380–5. PMID 27474819.
- Lødrup Carlsen, Karin C.; Skjerven, Håvard O.; Carlsen, Kai-Håkon (2018). "The toxicity of E-cigarettes and children's respiratory health". Paediatric Respiratory Reviews. 28: 63–67. doi:10.1016/j.prrv.2018.01.002. ISSN 1526-0542. PMID 29580719. S2CID 4368058.
- Holbrook, Bradley D. (2016). "The effects of nicotine on human fetal development". Birth Defects Research Part C: Embryo Today: Reviews. 108 (2): 181–192. doi:10.1002/bdrc.21128. ISSN 1542-975X. PMID 27297020.
- Makadia, Luv D.; Roper, P. Jervey; Andrews, Jeannette O.; Tingen, Martha S. (2017). "Tobacco Use and Smoke Exposure in Children: New Trends, Harm, and Strategies to Improve Health Outcomes". Current Allergy and Asthma Reports. 17 (8): 55. doi:10.1007/s11882-017-0723-0. ISSN 1529-7322. PMID 28741144. S2CID 22360961.
- Behnke, M.; Smith, V. C. (2013). "Prenatal Substance Abuse: Short- and Long-term Effects on the Exposed Fetus". Pediatrics. 131 (3): e1009–e1024. doi:10.1542/peds.2012-3931. ISSN 0031-4005. PMC 8194464. PMID 23439891. S2CID 135162.
- Kohlmeier, K. A. (2015). "Nicotine during pregnancy: changes induced in neurotransmission, which could heighten proclivity to addict and induce maladaptive control of attention". Journal of Developmental Origins of Health and Disease. 6 (3): 169–181. doi:10.1017/S2040174414000531. ISSN 2040-1744. PMID 25385318. S2CID 29298949.
- Alkam, Tursun; Nabeshima, Toshitaka (2019). "Molecular mechanisms for nicotine intoxication". Neurochemistry International. 125: 117–126. doi:10.1016/j.neuint.2019.02.006. ISSN 0197-0186. PMID 30779928. S2CID 72334402.
- SGUS 2016, p. vii; Preface.
- Drummond, MB; Upson, D (February 2014). "Electronic cigarettes. Potential harms and benefits". Annals of the American Thoracic Society. 11 (2): 236–42. doi:10.1513/annalsats.201311-391fr. PMC 5469426. PMID 24575993.
- "Electronic Nicotine Delivery Systems (ENDS), including E-cigarettes". New Zealand Ministry of Health. 2014. Archived from the original on 2015-05-11.
- "Electronic Cigarettes – An Overview" (PDF). German Cancer Research Center. 2013.
- Li, Gerard; Saad, Sonia; Oliver, Brian; Chen, Hui (2018). "Heat or Burn? Impacts of Intrauterine Tobacco Smoke and E-Cigarette Vapor Exposure on the Offspring's Health Outcome". Toxics. 6 (3): 43. doi:10.3390/toxics6030043. ISSN 2305-6304. PMC 6160993. PMID 30071638.
 This article incorporates text by Gerard Li, Sonia Saad, Brian G. Oliver, and Hui Chen available under the CC BY 4.0 license.
This article incorporates text by Gerard Li, Sonia Saad, Brian G. Oliver, and Hui Chen available under the CC BY 4.0 license. - "Electronic Cigarettes – What are the health effects of using e-cigarettes?" (PDF). Centers for Disease Control and Prevention. 22 February 2018.
- Greene, Robert M.; Pisano, M. Michele (2019). "Developmental toxicity of e-cigarette aerosols". Birth Defects Research. 111 (17): 1294–1301. doi:10.1002/bdr2.1571. ISSN 2472-1727. PMID 31400084. S2CID 199518879.