Health communication
Health communication is the study and practice of communicating promotional health information, such as in public health campaigns, health education, and between doctor and patient.[1] The purpose of disseminating health information is to influence personal health choices by improving health literacy. Health communication is a unique niche in healthcare that allows professionals to use communication strategies to inform and influence decisions and actions of the public to improve health.
Because effective health communication must be tailored for the audience and the situation,[2] research into health communication seeks to refine communication strategies to inform people about ways to enhance health or to avoid specific health risks.[3] Academically, health communication is a discipline within communication studies.[1]
Health communication may variously seek to:
- increase audience knowledge and awareness of a health issue[4]
- influence behaviors and attitudes toward a health issue
- demonstrate healthy practices
- demonstrate the benefits of behavior changes to public health outcomes
- advocate a position on a health issue or policy
- increase demand or support for health services
- argue against misconceptions about health[5]
- improve patient-provider dialogue[6]
- enhance effectiveness in health care teams[7]
Definition and Origins
Health communication is an area of research that focuses on the scope and implications of meaningful expressions and messages in situations or circumstances associated with health and health care.[8] Health communication is considered an interdisciplinary field of research, encompassing medical science, public health, and communication studies.
General health communication has origins dating as far back as the 4th century BC. Ancient Greek physician Hippocrates first began writing about the connection between diseases and the environment, laying the foundation for the modern understanding of transmittable diseases. Additionally, during the late 18th century, British Navy surgeon James Lind began formally documenting mortality among sailors in his medical publication Treatise of the Scurvy in 1753.[9]
The term health communications was used in 1961 when the National Health Council organized a National Health Forum to discuss challenges faced in the communications of health information (Helen, 1962).[10] The term was used again in 1962 when Surgeon General Luther Terry organized a conference on health communication to discuss how various techniques can make health information available to the public (US Department of Health Education and Welfare, 1963).[11] The term was adopted by members of an interest group at ICA, International Communication Association in 1975. The research of health communication surrounds the development of effective messages about health, the dissemination of health-related information through broadcast, print, and electronic media, and the role of inter personal relationships in health communities. At the core of all of the communication is the idea of health and the emphasis of health. The goal of health communication research is to identify and provide better and more effective communication strategies that will improve the overall health of society. (Atkin & Silk, page 489)[12]
Research
There are many purposes and reasons why health communication research is important and how it betters the health care field. The training programs of Health Care Professionals, or HCP, can be adapted and developed based on health communication research. (Atkin & Silk, 495)[12] One major example of a specialized research program is the Health Communication Research Unit at the University of Witwatersrand in Johannesburg, South Africa, aimed at studying the challenges to heath communication faced by cultural diversity.[13] Due to there being a diverse culture that makes up the group of patients within the health care field, communication to other cultures has been taught and has been made a focus in health care training classes. Research suggests that nonverbal and verbal communication between health care professionals and patient can lead to improved patient outcomes.[14] According to Atkin and Silk on page 496[12] some health care facilities, like hospitals are providing training and education materials to patients. The goal of hospitals doing this is to allow for patients to have a better outcome due to better communication skills. Over the years, there has been much research done on health communication. For example, researchers want to know if people are more effectively motivated by a positive message versus a negative message. Researchers examine ideas like, are people better motivated by ideas of wealth and safety or an idea of illness and death. Researchers are examining which dimensions of persuasive incentives are most influential: physical health versus economic, versus psychological, versus moral, versus social. (Atkin & Silk, 497)[12] Impact of the Health Campaign-After research has been conducted and analyzed on the effects of health communication, it can be concluded that a health communication campaign that is requiring a behavior change causes the desired behavior change in about 7%-10% or more in the people who are in the campaign site than those who are in the control group. Also, the effects are stronger for adoption of a new behavior than cessation of a current behavior, about 12% higher.
When assessing how affective a health campaign is, the key determinant is the degree of audience reception, the quality and quantity of the message, the dissemination channels, and the larger communication environment. It is possible that an audience can be more receptive to some messages than others. The media channel and how the message is reached by the audience can affect the effectiveness of the health campaign. (Atkin & Silk, page 498)[12]
The efforts and effects of health messages and communication are often counter affected by alcohol and tobacco commercials. The advertisement for these items is often made to be glamorous and will contradict what was said in the health campaign. This can lead to the efforts of the health communication seem to be pointless.
Training
Health communication professionals are specifically trained in methods and strategies for effective communication of public health messages, with qualifications in research, strategic development, and evaluating effectiveness.[2] Health communication is taught in master's and doctoral programs.[5][15] The Coalition for Health Communication maintains a list of such programs.[16]
The International Association for Communication in Healthcare (EACH) is a global organization aimed at improving the health communication sector between practitioners and patients. One major program EACH offers is "tEACH". tEACH is a specific subgroup focused on aiding teachers across the globe with tools and resources for promoting proper healthcare communication. The program consists of training modules, organized conferences, as well as project support.[17]
Scholars and practitioners in health communication are often trained in disciplines such as communication studies, sociology, psychology, public health, or medicine and then focus within their field on either health or communication. Practitioners are pragmatic and draw from social-scientific scholarship, theories from the humanities, and professional fields such as education, management, law and marketing (Maibach 2008). Professionals trained in health communication encounter a wide range of employment opportunities spanning between the public, private, and volunteer sectors and have the opportunity for a large amount of career mobility.[15] Examples of jobs in each of these categories include federal, state, and local health departments in the public sector, Pharmaceutical companies and large corporations in the private sector, and various non-profit organizations such as the American Cancer Society and the American Heart Association in the volunteer sector.
Overview
International Communication Association officially recognized health communication in 1975; in 1997, the American Public Health Association categorised health communication as a discipline of Public Health Education and Health Promotion.[5]
Careers in the field of health communication range widely between the public, private, and volunteer sectors and professionals of health communication are distinctively trained to conduct communication research, develop successful and repeatable campaigns for health promotion and advocacy, and to evaluate how effective these strategies have been for future campaigns.[2]
Clear communication is essential to successful public health practice at every level of the ecological model: intrapersonal, interpersonal, group, organizational, and societal. In each instance of health communication, there must be careful deliberation concerning the appropriate channel for messages to best reach the target audience, ranging from face-to-face interactions to television, Internet, and other forms of mass media.[18] The recent explosion of new Internet communication technologies, particularly through the development of health websites (such as MedlinePlus, Healthfinder, and WebMD), online support groups (such as the Association for Cancer Online Resources), web portals, tailored information systems, telehealth programs, electronic health records, social networking, and mobile devices (cell phones, PDAs, etc.) means that the potential media are ever changing.
The social and cultural contexts in which health communication occurs are also widely diverse and can include (but are not limited to) homes, schools, doctor's offices, and workplaces, and messages must consider the variant levels of health literacy and education of their audience, as well as demographics, values, socioeconomic issues, and many other factors that may influence effective communication.[2]
During the Covid-19 pandemic, it became clear that major topics in health communication include misinformation as well as the role of communication in addressing health inequities. Misinformation[19] had a major impact on vaccine acceptance and people’s adoption of pandemic prevention measures. Not only does misinformation contribute to vaccine hesitancy, social discrimination and stigma, but is also affected by the ongoing global trust[20] crisis in science and official sources. This further contributes to behavioural and social divides and to increasing long-standing inequities.[21] A narrative shift is essential to address these issues.
Critical Health Communication
Critical Health Communication refers to scholarship that interrogates "how meanings and enactments of health are tied to issues of power through the systematic construction and maintenance of inequalities."[22] It examines links with culture, resources, and other social structures.[22] It is distinct from mainstream Health Communication in its emphasis on qualitative and interpretive methods, and its attention to the ideological processes that underpin shared understandings of health. Unlike much mainstream Health Communication, most Critical Health Communication holds that simply circulating better quality, or more visible message about health is not enough to meaningfully influence health outcomes or correct health care disparities. The first comprehensive review of Critical Health Communication was published in 2008,[23] and since then the volume of Health Communication research taking a critical approach has steadily increased.
Strategies and methods
Tailoring a health message is one strategy for persuasive health communication.[24] For messages of health communication to reach selected audiences accurately and quickly, health communication professionals must assemble a collection of superior and audience appropriate information that target population segments. Understanding the audience for the information is critical to effective delivery.
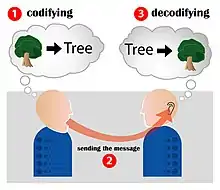
Communication is an enigma that is detrimental to the healthcare world and to the resulting health of a patient. Communication is an activity that involves oral speech, voice, tone, nonverbal body language, listening and more. It is a process for a mutual understanding to come at hand during interpersonal connections. A patient's communication with their healthcare team and vice versa, affects the outcome of their health. Strong, clear, and positive relationships with physicians can chronically improve and increase the condition of a certain patient. Through two approaches, the biomedical model and the biopsychosocial model; this can be successfully achieved. Evidence has shown that communication and its traditions have altered throughout the years. With the use of many new discoveries and the changes within our technology market, communication has severely improved and become instantaneous.
Communicators need to continually synthesize knowledge from a range of other scholarly disciplines including marketing, psychology, and behavioural sciences.[2] Once this information has been collected, professionals can choose from a variety of methods and strategies of communication that they believe would best convey their message. These methods include campaigns, entertainment advocacy, media advocacy, new technologies, and interpersonal communication.[5]
Campaigns
Health Communication campaigns are arguably the most utilized and effective method for spreading public health messages, especially in endorsing disease prevention (e.g. cancer, HIV/AIDS) and in general health promotion and wellness (e.g. family planning, reproductive health).[18] The Institute of Medicine argues that health communication campaigns tend to organize their message for a diverse audience in one of three ways:[5]
- By catering to the common denominator within the audience
- By creating one central message and then later making systematic alterations in order to better reach a certain audience segment, while retaining the same central message
- By creating distinctly different messages for different audience segments
Both the Centers for Disease Control and Prevention and scholars of health communication emphasize the importance of strategic planning throughout a campaign. This includes a variety of steps to ensure a well-developed message is being communicated:[3]
- Reviewing background information to define what the problem is and who is affected by the problem
- Setting communication objectives and proposing a plan to meet the wanted outcome
- Analyze the target audience by determining interests, attitudes, behaviors, benefits, and barriers
- Select channels and materials for communication in relation to what will most effectively reach audiences
- Develop and pretest message concepts to determine understanding, acceptance, and reaction to the message
- Implement communication with selected audience and monitor exposures and reactions to the message
- Ensure information is available in the language of intended audiences[25]
- Assess the outcome and evaluate the effectiveness and impact of the campaign, noting if changes need to be made
Historical campaigns
2014 African Ebola Outbreak
In 2018, four years after the first major outbreak of Ebola in Western Africa, the Democratic Republic of Congo and UNICEF partnered together to raise awareness about the deadly virus in a multi-national effort reaching around 800,000 people in affected areas. Communication efforts about preventive measures and safe practices regarding the virus included home visits by nurses, campaigns in major cities and markets, and broadcasting through mass media.[26]
China's 2019 "Zero-COVID" Policy
Following the global outbreak of the Covid-19 Pandemic in 2019, the Chinese government under Xi Jinping issued a major health communication campaign titled the "Zero-COVID" policy. This new set of restrictions included lockdowns, stricter contact-tracing mechanisms, and increased testing to Chinese citizens was aimed at attempting to stop the spread of Covid-19. The policy was relatively successful at slowing the spread of the virus, however, it did cause major food shortages and other problems.[27]
World Health Organization's (WHO) Heatwave Initiative
The WHO's "Heatwave and Health" initiative was launched in 2021 in co-partnership with the Pan American Health Organization aimed at educating the public in South and Central-American countries about the hazards present from heatwaves. Awareness including what to do before and during a heatwave was communicated in the form of webinars, information YouTube videos, and website articles. The campaign additionally focused on developing and/or strengthening local governments knowledge on the matter and establishing public safety plans when heatwaves are imminent.[28]
American smallpox epidemic
In 1721, health communication was used to mitigate the smallpox epidemic in Boston. Cotton Mather, a political leader, used pamphlets and speeches to promote inoculation of smallpox.[29]
Alcohol abuse
Alcohol abuse has been a problem within society for about as long as alcohol has been around. In the 19th century, the Women's Christian Temperance Union led a movement against alcohol abuse. They utilized mass communication to communicate the desired message. News papers and magazines allowed for the promotion of the anti-alcohol movement.[30]
Cardiovascular disease
Three-community study and the five-city project were experimental campaigns to inform middle-aged men about the causes of cardiovascular disease. Health messages were communicated via television, radio, newspaper, cookbooks, booklets, and bus cards. The three "communities" comprised three experimental communication strategies: a media-only campaign, a media campaign supplemented with face-to-face communication, and a no-intervention control group. The experimented revealed that after one year, the most informed at-risk men were those in the second experimental group: they men consumed the media campaign and were attended by a health care provider.
Entertainment media
Using the entertainment industry as a platform for advocating health information and education is a communication strategy that has become increasingly popular. The most utilized strategy is for health communication professionals to create partnerships with storyline creators so that public health information can be incorporated into within the plot of a television show. The Centers for Disease Control and Prevention has formed a strong partnership with Hollywood, Health, and Society, at the University of Southern California Norman Lear Center to continue to produce new storylines on television and in film studios that will help to promote public health information.[3] Some of the resources provided with this partnership include comprehensive "tip sheets" to provide writers with easy to access and trustworthy information on health issues, and meetings and panels to discuss new information and resources. Some of the most notable examples of this method of communication in recent years have been with the films Contagion and I Am Legend in understanding the spread of disease, NBC's series Parenthood in Asperger's Syndrome, and with the CW's series 90210 and spreading cancer awareness. More recently, film festivals and competitions focused specifically on health films have been organised by the American Public Health Association, the International Health Film Festival, the Global Health Film Initiative of the Royal Society of Medicine and the Public Health Film Society.[31][32][33][34]
Writers and storyline developers have an increased motivation to continue to incorporate public health information into their scripts with the creation of the Sentinel for Health Awards in 2000, which honors storylines that effectively promote health topics and audience awareness of public health issues.[3] Surveys conducted by Porter Novelli in 2001 reported many interesting statistics on the effectiveness of this strategy, such as that over half of regular prime time and daytime drama viewers have reported that they have learned something about health promotion or disease prevention from a TV show.[5] Amongst this data, minority groups are significantly represented with well over half of African American and Hispanic viewers stating that they had either taken some form of preventative action after hearing about a health issue on TV, or that a TV storyline helped them to provide vital health information to a friend or family member.
Direct marketing

Media advocacy use strategic mass media tools combined with widespread organization in order to advocate for healthy public policies or lifestyles.[5] This can include the use of text messaging and email to spread messages from person to person, and using social networking venues to promote health information to a wide-ranging audience. As technologies expand, the platforms for health communication through media advocacy will undoubtedly expand as well.
Interpersonal communication
Health communication relies on strong interpersonal communication in order to influence health decisions and behaviours. The most important of these relationships are the connection and interaction between an individual and their health care provider (e.g., physician, therapist, pharmacist) and an individual's social support system (family, friends, community). These connections can positively influence the individual's decision to make healthy choices.[5] Patients are more prone to listen when they feel invested emotionally into the situation. If they feel as if they understand what is being said, they are more prone to make objective decisions based on the information heard. Two of the most prominent areas of study in interpersonal health communication are the patient-centered and the relationship centered models of care.[35]
Applications
Health communication has become essential in promoting the general public health in myriad situations. One of health communication's most important applications has been throughout major Environmental events (e.g. hurricanes, flooding, tornados) and addressing the affected audience's questions and needs quickly and efficiently, keeping the protection of public health and the forefront of their message.[2] Health communication professionals are constantly working to improve this type of risk communication in order to be prepared in the case of an emergency.
Another increasingly important application of health communication has been in reaching students in the college community. The National College Health Assessment has measured that 92.5% of college students reported being in "good, very good, or excellent health", however college students seem to battle serious problems with stress, depression, substance abuse, and a general lack of nutrition in comparison to other age groups and audiences.[36] Professionals in health communication are actively striving for new ways to reach this at-risk audience in order to raise standards of public health in the college setting and to promote a healthier life style amongst students.
Challenges
There are many challenges in communicating information about health to individuals. Some of the most essential issues have to do with the gap between individual health literacy and healthcare workers and institutions, as well as flaws in communicating health information through mass media.
Health communication is additionally influenced by cultural values which in some cases can create a barrier in effective health communication. When the sender and receiver are from contrasting socioeconomic backgrounds, of a different race, or even vastly different ages, effective health communication declines. This is a result of the fact that people tend to trust and be more open to ideas coming from someone similar to themselves.[37]
Literacy-communication gap
One problem that health communication seeks to address is the gap that has formed between health literacy and the use of health communication.[38] While the goal is that health communication will effectively lead to health literacy, issues such as the use of unexplained medical jargon, ill-formed messages, and often a general educational gap have created barriers to patient healthcare literacy. Specifically, studies have been done amongst elderly populations in America to illustrate a common audience who is left at a disadvantage due to this issue.[39] The older adults comprise an age group that generally has the most chronic health conditions in comparison to other age groups, however studies have shown that this group has difficulty understanding written health materials, understanding health care and policies, and generally do not comprehend medical jargon. Such shortcomings of health communication may lead to increased hospitalizations, the inability to respond to and manage a disease or medical condition, and a generally declining health status.
To redress these problems, health communication professionals have recommended programs for improving physician communication with patients. One recommendation is to improve medical student training by adding lectures, workshops, and supervised encounters with patients to teach interpersonal and communication skills as a core competency.[40] It is also recommended that practicing physicians improve their communication skills by attending webinars and on-site customized training programs. If physicians can improve their communication skills, they can ameliorate the problem of patient healthcare illiteracy and contribute to better patient adherence to medical advice.
In some populations, health-related websites (e.g., WebMD) and online support groups (e.g., Association for Cancer Online Resources) have increased access to health information.[5] The role of language in communication, especially related to the patients' preferred language physicians use to communicate with them in, also plays a role. Results of a 2019 systematic review found that limited English proficient (LEP) patients have improved health outcomes when they receive care from physicians fluent in the patients' own preferred language.[41] The National Institute for Health and Care Research (NIHR) has published review of research for providers of health information, on what happens when health information is not clear, how to help people understand health information, and which groups of the population may need extra support understanding health content.[42] It covers research on using simple, balanced language, finding the correct focus, alternative formats (e.g. videos, visuals), and online information.
Mass media
Mass communication is used to promote beneficial changes in behavior among members of populations.[43] A major criticism of the use of mass media as a method of health communication is the unfortunate ability for false and misinformed messages to spread quickly through the mass media, before they have the chance to be disputed by professionals. This issue may generate unwarranted panic amongst those who receive the messages and be an issue as technology continues to advance. An example of this may be observed in the ongoing distrust of vaccinations due to the publication of numerous messages that wrongly link the childhood measles-mumps-rubella (MMR) vaccination with the development and onset of Autism.[44] The speed with which this message spread due to new social networking technologies caused many parents to distrust vaccinations and therefore forgo having their children receive the vaccine. Although this panic is based on false information, many still harbor a lingering suspicion towards vaccinations and refuse them, which has caused a public health concern.
Historical timeline
The following are some key events in the development of health communication as a formal discipline since the 1970s.[45]
- International Communication Association establishes the Therapeutic Communication Interest Group (which later became the "Health Communication" Division)
- The American Academy on Physician and Patient (later renamed the American Academy on Communication in Healthcare) was established to promote research, education, and professional standards in patient-clinician communication.
- Health communication textbooks begin appearing: Kreps & Thornton (1984), Sharf (1984), and Northhouse & Northhouse (1985)
- National Communication Association forms the Commission for Health Communication, which later became the Health Communication Division
- First peer reviewed journal devoted to health communication, Health Communication. Followed in 1996 by the Journal of Health Communication
- Undergraduate and graduate health communication majors begin to be offered. Tufts University School of Medicine offers the first Master of Science in health communication together with Emerson College
- The Health Communication Working Group of the American Public Health Association was established to examine the role of health communication in public health promotion.
- The National Cancer Institute (National Institutes of Health) establishes the Health Communication and Informatics Research Branch (HCIRB) in their Behavioral Research Program, Division of Cancer Prevention and Control. The National Cancer Institute identifies health communication as an extraordinay research opportunity for promoting cancer prevention and control.
- The National Cancer Institute establishes the Health Communication Intervention research program, funding seven multi-year research projects to study innovative strategies for communicating cancer information to diverse populations.
- The Journal of Medical Internet Research is established to study health and health care in the Internet age.
- The National Cancer Institute establishes the Health Information National Trends Survey (HINTS) biennial representative national survey of consumer health information seeking, acquisition, and use to evaluate progress in cancer communication and to guide health communication intervention.
- The National Cancer Institute announced establishment of four national Centers of Excellent in Cancer Communication Research (CECCRs) providing five year funding for research centers at the University of Pennsylvania, University of Wisconsin, University of Michigan, and Saint Louis University. The CECCR program was designed to make major advances in health communication research and application, as well as to train the next generation of health communication scholars.
- The Centers for Disease Control and Prevention (CDC) establishes the National Center for Health Marketing (NCHM)for promoting and conducting health marketing and communication research to support national health promotion efforts.
- The Coalition for Health Communication (CHC) is established as an inter-organizational task force whose mission is to strengthen the identity and advance the field of health communication. CHC represents the ICA and NCA Health Communication Divisions and the APHA Health Communication Working Group.
- The first dedicated Ph.D. program in Health and Strategic Communication is offered by the George Mason University Department of Communication.
- The National Cancer Institute announced re-issuing of the national Centers of Excellent in Cancer Communication Research (CECCRs) program. They provided five years of funding for five research centers (at the University of Pennsylvania, University of Wisconsin, University of Michigan, Washington University in St. Louis, and Kaiser Permanente, Colorado. The new CECCR program was designed to continue progress in advancing in health communication research and application, as well as to train the next generation of health communication scholars.
- First serious efforts put forth by Home Controls' HealthComm Systems to educate consumers regarding affordable, unobtrusive home technology allowing the aging to remain at home for months or years longer than ever before
- The Society for Participatory Medicine (SPM) is established to promote participatory medicine by and among patients, caregivers and their medical teams and to promote clinical transparency among patients and their physicians through the exchange of information, via conferences, as well through the distribution of correspondence and other written materials. The SPM publishes the Journal of Participatory Medicine.
- The Murrow Center for Media and Health Promotion is established at Washington State University.
- The Center for Health Communication is established in the Moody College of Communication at the University of Texas at Austin.
- The Public Health Film Society (PHFS), an independent charity is established to promote conversations between the health and artistic communities about public health messages in film, and to promote transparency in the portray of health messages to the general public through film festivals, international film competitions, as well through the distribution of correspondence and peer-reviewed research.[31][34]
See also
References
Notes
- "What is Communication?". National Communication Association. Retrieved 30 May 2013.
- Beato, Ricardo R.; Jana Telfer (July–August 2010). "Communication as an Essential Component of Environmental Health Science" (PDF). Journal of Environmental Health. 73 (1): 24–25. PMID 20687329. Retrieved 24 March 2013.
- Centers for Disease Control and Prevention. "Health Communication Basics". Retrieved 24 March 2013.
- Gwyn, Richard (2002). Communicating health and illness. London: Sage Publications Ltd. ISBN 978-0761964759.
- Freimuth, Vicki S.; Sandra Crouse Quinn (December 2004). "The Contributions of Health Communication to Eliminating Health Disparities". American Journal of Public Health. 94 (12): 2053–2055. doi:10.2105/ajph.94.12.2053. PMC 1448587. PMID 15569949.
- Dutta-Bergman, Mohan J. (2005). "The Relation Between Health-Orientation, Provider-Patient Communication, and Satisfaction: An Individual-Difference Approach". Health Communication. 18 (3): 291–303. doi:10.1207/s15327027hc1803_6. ISSN 1041-0236. PMID 16187933. S2CID 23884129.
- Fox, Stephanie; Gaboury, Isabelle; Chiocchio, François; Vachon, Brigitte (2021-01-28). "Communication and Interprofessional Collaboration in Primary Care: From Ideal to Reality in Practice". Health Communication. 36 (2): 125–135. doi:10.1080/10410236.2019.1666499. ISSN 1041-0236. PMID 31580162. S2CID 203653041.
- Thompson, Teresa (2000). Whaley, B.B. (ed.). The nature and language of illness explanations. Mahwah, NJ: Erlbaum. pp. 3–40.
- Dlima, Schenelle (2021-01-29). "The History of Health Communication". Saathealth Spotlight. Retrieved 2023-04-09.
- Neal, H. (Ed.). (1962). Better communications for better health. New York, NY: Columbia University Press.
- USPHS. (1963). Surgeon General's Conference on Health Communications November 5–8, 1962. PHS publication, 5-8.
- Atkin, Charles; Silk, Kami (2009). "Health Communication". In Stacks, Don W.; Salwen, Michael B. (eds.). An Integrated Approach to Communication Theory and Research. Communication Theory and Methodology (Second ed.). Routledge. pp. 489–503. doi:10.4324/9780203887011. ISBN 978-0-8058-6381-9.
- "Home - Wits University". www.wits.ac.za. Retrieved 2023-04-20.
- Grossbach, Irene; Stranberg, Sarah; Chlan, Linda (2011-06-01). "Promoting Effective Communication for Patients Receiving Mechanical Ventilation". Critical Care Nurse. 31 (3): 46–60. doi:10.4037/ccn2010728. ISSN 0279-5442. PMID 20807893.
- Edgar, Timothy; James N. Hyde (November 2004). "An Alumni-Based Evaluation of Graduate Training in Health Communication: Results of a Survey on Careers, Salaries, Competencies, and Emerging Trends". Journal of Health Communication. 10 (1): 5–25. doi:10.1080/10810730590904553. PMID 15764441. S2CID 11085610.
- "Graduate Programs in Health Communication". Archived from the original on 7 November 2018. Retrieved 2 March 2013.
- "Teaching - EACH". EACH. Retrieved 2023-04-11.
- Parvis, Leo (Jul–Aug 2002). "How to Benefit From Health Communication". Journal of Environmental Health. 65 (1): 41. PMID 12148326.
- Schiavo, Renata (2021-10-02). "Telling our own stories: The role of narrative in confronting stigma and misinformation". Journal of Communication in Healthcare. 14 (4): 269–270. doi:10.1080/17538068.2021.2002592. ISSN 1753-8068. S2CID 244775363.
- Schiavo, Renata; Eyal, Gil; Obregon, Rafael; Quinn, Sandra C.; Riess, Helen; Boston-Fisher, Nikita (2022-10-10). "The science of trust: future directions, research gaps, and implications for health and risk communication". Journal of Communication in Healthcare. 15 (4): 245–259. doi:10.1080/17538068.2022.2121199. ISSN 1753-8068. PMID 36911900. S2CID 252838082.
- Schiavo, Renata; Wye, Gretchen Van; Manoncourt, Erma (2022-01-02). "COVID-19 and health inequities: the case for embracing complexity and investing in equity- and community-driven approaches to communication". Journal of Communication in Healthcare. 15 (1): 1–6. doi:10.1080/17538068.2022.2037349. ISSN 1753-8068. S2CID 247453892.
- ""Doing" Critical Health Communication. A Forum on Methods | Frontiers Research Topic". Retrieved 2018-11-29.
- Zoller, Heather M.; Kline, Kimberly N. (January 2008). "Theoretical Contributions of Interpretive and Critical Research in Health Communication". Annals of the International Communication Association. 32 (1): 89–135. doi:10.1080/23808985.2008.11679076. ISSN 2380-8985. S2CID 148377352.
- Noar, Seth M.; Christina N. Benac; Melissa S. Harris (2007). "Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions". Psychological Bulletin. 133 (4): 673–693. doi:10.1037/0033-2909.133.4.673. PMID 17592961.
- "Advancing Equity In The Pandemic Treaty". 2023-05-09. doi:10.1377/forefront.20230504.241626.
{{cite journal}}: Cite journal requires|journal=(help) - "More than 300,000 people reached with awareness-raising campaign to contain deadly Ebola outbreak in DRC". www.unicef.org. Retrieved 2023-04-08.
- "What Is China's 'Zero-COVID' Policy?". VOA. 28 November 2022. Retrieved 2023-04-08.
- "Heatwaves and Health - PAHO/WHO | Pan American Health Organization". www.paho.org. Retrieved 2023-04-08.
- "When Cotton Mather Fought The Smallpox | AMERICAN HERITAGE". www.americanheritage.com. Retrieved 2018-10-12.
- "When Cotton Mather Fought The Smallpox | AMERICAN HERITAGE". www.americanheritage.com. Retrieved 2018-10-12.
- Botchway, Stella; Hoang, Uy (2016). "Reflections on the United Kingdom's first public health film festival". Perspectives in Public Health. 136 (1): 23–24. doi:10.1177/1757913915619120. PMID 26702114. S2CID 21969020.
- "The APHA Global Public Health Film Festival".
- "Global Health Film | Home".
- Hoang, U.; Luna, P.; Russell, P.; Bergonzi-King, L.; Ashton, J.; McCarthy, C.; Donovan, H.; Inman, P.; Seminog, O.; Botchway, S. (2018). "First International Public Health Film Competition 2016—reflections on the development and use of competition judging criteria". Journal of Public Health. 40: 169–174. doi:10.1093/pubmed/fdx022. PMID 28369436. S2CID 4055604.
- Apker, Julie (2011). Communication in health organizations (1 ed.). Cambridge, UK: Polity Press. ISBN 978-0-745-64754-8.
- Baxter, Leslie; Nichole Egbert; Evelyn Ho (Jan–Feb 2008). "Everyday Health Communication Experiences of College Students". Journal of American College Health. 56 (4): 427–435. doi:10.3200/jach.56.44.427-436. PMID 18316288. S2CID 19254752.
- Kreuter, Matthew W.; McClure, Stephanie M. (2004-04-01). "The Role of Culture in Health Communication". Annual Review of Public Health. 25 (1): 439–455. doi:10.1146/annurev.publhealth.25.101802.123000. ISSN 0163-7525. PMID 15015929.
- Viswanath K, Finnegan JR (1996). ".". In Burleson, B (ed.). Communication Yearbook 19. SAGE Publications. pp. 187–227.
- Hester, Eva Jackson (February 2009). "An Investigation of the Relationship Between Health Literacy and Social Communication Skills in Older Adults". Communication Disorders Quarterly. 30 (2): 112–119. CiteSeerX 10.1.1.666.701. doi:10.1177/1525740108324040. S2CID 143464629.
- Christianson JB (2012). Physician Communication with Patients: Research Findings and Challenges. University of Michigan Press. pp. 222–238.
- Diamond, Lisa; Izquierdo, Karen; Canfield, Dana; Matsoukas, Konstantina; Gany, Francesca (2019). "A Systematic Review of the Impact of Patient–Physician Non-English Language Concordance on Quality of Care and Outcomes". Journal of General Internal Medicine. 34 (8): 1591–1606. doi:10.1007/s11606-019-04847-5. ISSN 0884-8734. PMC 6667611. PMID 31147980.
- "Health information: are you getting your message across?". NIHR Evidence. 13 June 2022. doi:10.3310/nihrevidence_51109. S2CID 249946766.
- Abroms, LC; Maibach, EW (2008). "The effectiveness of mass communication to change public behavior". Annual Review of Public Health. 29: 219–34. doi:10.1146/annurev.publhealth.29.020907.090824. PMID 18173391.
- Brauser, Deborah (January 6, 2001). "Autism and MMR Vaccine Study an 'Elaborate Fraud,' Charger BMJ".
- Kreps et al. 1998
Sources
- U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2010. Volumes 1 and 2, Chapt. 11, p 11–20. https://web.archive.org/web/20100122053253/http://www.healthypeople.gov/document/HTML/Volume1/11HealthCom.htm.
- Cline R., American Public Health Association (APHA) Health Communication Working Group Brochure, 2003. https://web.archive.org/web/20190119083227/http://www.healthcommunication.net/APHA/APHA.html. Retrieved in January 2010.
- Schiavo, R. Health Communication: From Theory to Practice. San Francisco: Jossey-Bass, 2007.
- Thompson, Teresa; Roxanne Parrott; Jon Nussbaum (2011). The Routledge Handbook of Health Communication (2 ed.). ISBN 978-0-203-84606-3.
- Kreps, G. L.; et al. (1998). "The History and Developments of the Field of Health Communication". Health communication research : a guide to developments and directions. Westport, Conn.: Greenwood Press. doi:10.1145/1125451.1125549.
- Rimal, R. N.; Lapinski (2009). Why Health Communication is Important in Public Health. PMC 2672574. Archived from the original on April 14, 2009.
- Maibach, E. W. (2008). Communication for Health.
- Ringo Ma. (Ed.) (2009). Jiankang chuanbo yu gonggong weisheng [Health communication and public health]. Hong Kong: Hong Kong Educational. (in Chinese and English)
- Ringo Ma. (Ed.) (2009). Yi bing goutong zhi duoshao [How much do you know about doctor-patient communication?]. Hong Kong: KAI Education. (in Chinese and English)
- Teresa L. Thompson; Alicia Dorsey; Roxanne Parrott; Katherine Miller (1 April 2003). The Handbook of Health Communication. Lawrence Erlbaum Assoc. ISBN 978-1-4106-0768-3. Retrieved 30 May 2013.
External links
| Library resources about Health communication |
- American Public Health Association Health Communication Working Group
- The Annenberg Public Policy Center, Health Communication
- Applied Research on Communication in Health Group, University of Otago, Wellington
- Center for Communication and Health, Northwestern University Archived 2016-04-09 at the Wayback Machine
- Center for Excellence in Health Communication to Underserved Populations, The University of Kansas William Allen White School of Journalism and Mass Communications Archived 2015-09-06 at the Wayback Machine
- Center for Health Communication, Moody College of Communication, The University of Texas at Austin
- Center for Health Communication, Harvard T.H. Chan School of Public Health
- Center for Health Communication Intervention
- Center for Health Communications Research, University of Michigan
- Center for Health Literacy, MAXIMUS
- The Center for Health & Risk Communication, George Mason University
- Center for Health and Risk Communication, University of Maryland
- Center for Public Health Readiness and Communication, Drexel University School of Public Health
- Coalition for Healthcare Communication
- Ebola Communication Network
- FHI 360 Center for Global Health Communication and Marketing
- Centre for Health Communication and Participation, La Trobe University
- Gateway to Health Communication & Social Marketing Practice, Centers for Disease Control and Prevention
- Health Communication Partnership
- Health Communication Research Centre, Cardiff School of English, Communication & Philosophy
- Health and Science Communications Association
- Health Communication Research Center, The Missouri School of Journalism
- Health information: are you getting your message across?
- International Communication Association, Health Communication Section
- Institute for Healthcare Communication
- International Communication Association
- Johns Hopkins University Center for Communication Programs
- Lerner Center for Public Health Promotion, Columbia University Mailman School of Public Health
- Office of Disease Prevention and Health Promotion Health Communication Activities
- University of Georgia Center for Health and Risk Communications Archived 2017-11-13 at the Wayback Machine
- Graduate Program in Health Communication, Tufts University School of Medicine
- Journal of Health Communication Archived 2013-05-02 at the Wayback Machine
- Public Health Film Society