Trousseau sign of malignancy
The Trousseau sign of malignancy or Trousseau's syndrome is a medical sign involving episodes of vessel inflammation due to blood clot (thrombophlebitis) which are recurrent or appearing in different locations over time (thrombophlebitis migrans or migratory thrombophlebitis). The location of the clot is tender and the clot can be felt as a nodule under the skin.[1] Trousseau's syndrome is a rare variant of venous thrombosis that is characterized by recurrent, migratory thrombosis in superficial veins and in uncommon sites, such as the chest wall and arms. This syndrome is particularly associated with pancreatic, gastric and lung cancer and Trousseau's syndrome can be an early sign of cancer[2][3] sometimes appearing months to years before the tumor would be otherwise detected.[4] Heparin therapy is recommended to prevent future clots.[5] The Trousseau sign of malignancy should not be confused with the Trousseau sign of latent tetany caused by low levels of calcium in the blood.
| Trousseau sign of malignancy | |
|---|---|
| Differential diagnosis | thrombophlebitis migrans |
History
Armand Trousseau first described this finding in the 1860s; he later found the same sign in himself, was subsequently diagnosed with gastric cancer and died soon thereafter.[6] Trousseau presciently attributed thromboembolism in malignancy to changes in blood composition rather than local inflammatory or mechanical forces. By correlating clinical observation with surgical and autopsy findings, Trousseau recognized that a localized cancer could induce a generalized hypercoagulable state in which thrombosis could occur elsewhere in the body, such as in extremities with visceral malignancy. Trousseau described several cases in which recurrent thrombosis was the presenting feature of visceral cancer, and his confidence in the utility of this connection led him to say, "So great, in my opinion, is the semiotic value of phlegmasia in the cancerous cachexia, that I regard this phlegmasia as a sign of the cancerous diathesis as certain as sanguinolent effusion into the serous cavities."
Pathophysiology
Some malignancies, especially gliomas (25%), as well as adenocarcinomas of the pancreas and lung, are associated with hypercoagulability (the tendency to form blood clots) for reasons that are incompletely understood, but may be related to factors secreted by the tumors, in particular a circulating pool of cell-derived tissue factor-containing microvesicles.[7] Some adenocarcinomas secrete mucin that can interact with selectin found on platelets, thereby causing small clots to form.[8][9] Moreover, most malignant tumors overexpress and secrete heparanase,[10] an enzyme that degrade heparan sulfate [11] and endogenous heparin,[12] and thus contribute to the hypercoagulable state in cancer patients.[13][14][15]
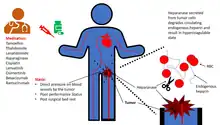
In patients with malignancy-associated hypercoagulable states, the blood may spontaneously form clots in the portal vessels (portal vein thrombosis), the deep veins of the limbs (deep vein thrombosis), or the superficial veins (superficial vein thrombosis) anywhere on the body. These clots present as visibly swollen blood vessels (thrombophlebitis), especially the veins, or as intermittent pain in the affected areas.
References
- Trousseau's sign of visceral malignancy in GPnotebook, retrieved November 2012
- Caine, Graham (Nov 2002). "The Hypercoagulable State of Malignancy: Pathogenesis and Current Debate". Neoplasia. 4 (6): 465–473. doi:10.1038/sj.neo.7900263. PMC 1550339. PMID 12407439.
- Callander, N; S I Rapaport (1993). "Trousseau's syndrome". Western Journal of Medicine. 158 (4): 364–371. ISSN 0093-0415. PMC 1022062. PMID 8317122.
- "Trousseau sign" at Dorland's Medical Dictionary
- Callander, N; S I Rapaport (1993). "Trousseau's syndrome". Western Journal of Medicine. 158 (4): 364–371. ISSN 0093-0415. PMC 1022062. PMID 8317122.
- Samuels MA, King ME, Balis U (2002). "Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 31-2002. A 61-year-old man with headache and multiple infarcts". N. Engl. J. Med. 347 (15): 1187–94. doi:10.1056/NEJMcpc020117. PMID 12374880.
- Del Conde I, Bharwani LD, Dietzen DJ, Pendurthi U, Thiagarajan P, López JA (2007). "Microvesicle-associated tissue factor and Trousseau's syndrome". J Thromb Haemost. 5 (1): 70–4. doi:10.1111/j.1538-7836.2006.02301.x. PMC 3410746. PMID 17239164.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Wahrenbrock M, Borsig L, Le D, Varki N, Varki A (2003). "Selectin-mucin interactions as a probable molecular explanation for the association of Trousseau syndrome with mucinous adenocarcinomas". J Clin Invest. 112 (6): 853–862. doi:10.1172/jci200318882. PMC 193671. PMID 12975470.
- Varki, Ajit (2007). "Trousseau's syndrome: multiple definitions and multiple mechanisms". Blood. 110 (6): 1723–1729. doi:10.1182/blood-2006-10-053736. ISSN 0006-4971. PMC 1976377. PMID 17496204.
- Edovitsky, Evgeny; Elkin, Michael; Zcharia, Eyal; Peretz, Tamar; Vlodavsky, Israel (2004-08-18). "Heparanase gene silencing, tumor invasiveness, angiogenesis, and metastasis". Journal of the National Cancer Institute. 96 (16): 1219–1230. doi:10.1093/jnci/djh230. ISSN 1460-2105. PMID 15316057.
- Vlodavsky, I.; Friedmann, Y.; Elkin, M.; Aingorn, H.; Atzmon, R.; Ishai-Michaeli, R.; Bitan, M.; Pappo, O.; Peretz, T.; Michal, I.; Spector, L. (July 1999). "Mammalian heparanase: gene cloning, expression and function in tumor progression and metastasis". Nature Medicine. 5 (7): 793–802. doi:10.1038/10518. ISSN 1078-8956. PMID 10395325. S2CID 38895589.
- Nasser, N. J.; Sarig, G.; Brenner, B.; Nevo, E.; Goldshmidt, O.; Zcharia, E.; Li, J. P.; Vlodavsky, I. (March 2006). "Heparanase neutralizes the anticoagulation properties of heparin and low-molecular-weight heparin". Journal of Thrombosis and Haemostasis. 4 (3): 560–565. doi:10.1111/j.1538-7836.2006.01792.x. ISSN 1538-7933. PMID 16460439.
- Nasser, Nicola J.; Na'amad, Mira; Weinberg, Ido; Gabizon, Alberto A. (January 2015). "Pharmacokinetics of low molecular weight heparin in patients with malignant tumors". Anti-Cancer Drugs. 26 (1): 106–111. doi:10.1097/CAD.0000000000000176. ISSN 1473-5741. PMID 25280062. S2CID 6639067.
- Rickles, F. R. (March 2006). "If heparanase is the answer, what is the question?". Journal of Thrombosis and Haemostasis. 4 (3): 557–559. doi:10.1111/j.1538-7836.2006.01828.x. ISSN 1538-7933. PMID 16460438. S2CID 5631803.
- Nasser, Nicola J.; Fox, Jana; Agbarya, Abed (2020-02-29). "Potential Mechanisms of Cancer-Related Hypercoagulability". Cancers. 12 (3): 566. doi:10.3390/cancers12030566. ISSN 2072-6694. PMC 7139427. PMID 32121387.