Acute-phase protein
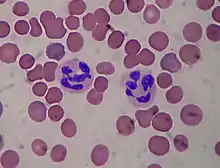
Acute-phase proteins (APPs) are a class of proteins whose concentrations in blood plasma either increase (positive acute-phase proteins) or decrease (negative acute-phase proteins) in response to inflammation. This response is called the acute-phase reaction (also called acute-phase response). The acute-phase reaction characteristically involves fever, acceleration of peripheral leukocytes, circulating neutrophils and their precursors.[1] The terms acute-phase protein and acute-phase reactant (APR) are often used synonymously, although some APRs are (strictly speaking) polypeptides rather than proteins.
In response to injury, local inflammatory cells (neutrophil granulocytes and macrophages) secrete a number of cytokines into the bloodstream, most notable of which are the interleukins IL1, and IL6, and TNF-α. The liver responds by producing many acute-phase reactants. At the same time, the production of a number of other proteins is reduced; these proteins are, therefore, referred to as "negative" acute-phase reactants. Increased acute-phase proteins from the liver may also contribute to the promotion of sepsis.[2]
Regulation of synthesis
TNF-α, IL-1β and IFN-γ are important for the expression of inflammatory mediators such as prostaglandins and leukotrienes, and they also cause the production of platelet-activating factor and IL-6. After stimulation with proinflammatory cytokines, Kupffer cells produce IL-6 in the liver and present it to the hepatocytes. IL-6 is the major mediator for the hepatocytic secretion of APPs. Synthesis of APP can also be regulated indirectly by cortisol. Cortisol can enhance expression of IL-6 receptors in liver cells and induce IL-6-mediated production of APPs.[1]
Positive
Positive acute-phase proteins serve (as part of the innate immune system) different physiological functions within the immune system. Some act to destroy or inhibit growth of microbes, e.g., C-reactive protein, mannose-binding protein,[3] complement factors, ferritin, ceruloplasmin, serum amyloid A and haptoglobin. Others give negative feedback on the inflammatory response, e.g. serpins. Alpha 2-macroglobulin and coagulation factors affect coagulation, mainly stimulating it. This pro-coagulant effect may limit infection by trapping pathogens in local blood clots.[1] Also, some products of the coagulation system can contribute to the innate immune system by their ability to increase vascular permeability and act as chemotactic agents for phagocytic cells.
| Protein | Immune system function |
|---|---|
| C-reactive protein | Opsonin on microbes[4] (not an acute-phase reactant in mice) |
| Serum amyloid P component | Opsonin |
| Serum amyloid A |
|
| Complement factors | Opsonization, lysis and clumping of target cells. Chemotaxis |
| Mannan-binding lectin | Mannan-binding lectin pathway of complement activation |
| Fibrinogen, prothrombin, factor VIII, von Willebrand factor |
Coagulation factors, trapping invading microbes in blood clots. Some cause chemotaxis |
| Plasminogen activator inhibitor-1 (PAI-1) | Prevents the degradation of blood clots by inhibiting tissue Plasminogen Activator (tPA) |
| Alpha 2-macroglobulin |
|
| Ferritin | Binding iron, inhibiting microbe iron uptake |
| Hepcidin[6] | Stimulates the internalization of ferroportin, preventing release of iron bound by ferritin within intestinal enterocytes and macrophages |
| Ceruloplasmin | Oxidizes iron, facilitating for ferritin, inhibiting microbe iron uptake |
| Haptoglobin | Binds hemoglobin, inhibiting microbe iron uptake and prevents kidney damage |
| Orosomucoid (Alpha-1-acid glycoprotein, AGP) |
Steroid carrier |
| Alpha 1-antitrypsin | Serpin, downregulates inflammation |
| Alpha 1-antichymotrypsin | Serpin, downregulates inflammation |
Negative
"Negative" acute-phase proteins decrease in inflammation. Examples include albumin,[7] transferrin,[7] transthyretin,[7] retinol-binding protein, antithrombin, transcortin. The decrease of such proteins may be used as markers of inflammation. The physiological role of decreased synthesis of such proteins is generally to save amino acids for producing "positive" acute-phase proteins more efficiently. Theoretically, a decrease in transferrin could additionally be decreased by an upregulation of transferrin receptors, but the latter does not appear to change with inflammation.[8]
While the production of C3 (a complement factor) increases in the liver, the plasma concentration often lowers because of an increased turn-over, therefore it is often seen as a negative acute-phase protein.
Clinical significance
Measurement of acute-phase proteins, especially C-reactive protein, is a useful marker of inflammation in both medical and veterinary clinical pathology. It correlates with the erythrocyte sedimentation rate (ESR), however not always directly. This is due to the ESR being largely dependent on the elevation of fibrinogen, an acute phase reactant with a half-life of approximately one week. This protein will therefore remain higher for longer despite the removal of the inflammatory stimuli. In contrast, C-reactive protein (with a half-life of 6–8 hours) rises rapidly and can quickly return to within the normal range if treatment is employed. For example, in active systemic lupus erythematosus, one may find a raised ESR but normal C-reactive protein.They may also indicate liver failure.[9]
References
- Jain S, Gautam V, Naseem S (January 2011). "Acute-phase proteins: As diagnostic tool". Journal of Pharmacy & Bioallied Sciences. 3 (1): 118–27. doi:10.4103/0975-7406.76489. PMC 3053509. PMID 21430962.
- Abbas A, Lichtman A, Pillai S (2012). Basic immunology Functions and Disorders of the Immune System (4th ed.). Philadelphia, PA: Saunders/Elsevier. p. 40.
- Herpers BL, Endeman H, de Jong BA, de Jongh BM, Grutters JC, Biesma DH, van Velzen-Blad H (Jun 2009). "Acute-phase responsiveness of mannose-binding lectin in community-acquired pneumonia is highly dependent upon MBL2 genotypes". Clin Exp Immunol. 156 (3): 488–94. doi:10.1111/j.1365-2249.2009.03929.x. PMC 2691978. PMID 19438602.
- Lippincott's Illustrated Reviews: Immunology. Paperback: 384 pages. Publisher: Lippincott Williams & Wilkins; (July 1, 2007). Language: English. ISBN 0-7817-9543-5. ISBN 978-0-7817-9543-2. Page 182
- de Boer JP, Creasey AA, Chang A, Abbink JJ, Roem D, Eerenberg AJ, et al. (December 1993). "Alpha-2-macroglobulin functions as an inhibitor of fibrinolytic, clotting, and neutrophilic proteinases in sepsis: studies using a baboon model". Infection and Immunity. 61 (12): 5035–43. doi:10.1128/iai.61.12.5035-5043.1993. PMC 281280. PMID 7693593.
- Vecchi C, Montosi G, Zhang K, et al. (August 2009). "ER stress controls iron metabolism through induction of hepcidin". Science. 325 (5942): 877–80. Bibcode:2009Sci...325..877V. doi:10.1126/science.1176639. PMC 2923557. PMID 19679815.
- Ritchie RF, Palomaki GE, Neveux LM, Navolotskaia O, Ledue TB, Craig WY (1999). "Reference distributions for the negative acute-phase serum proteins, albumin, transferrin, and transthyretin: a practical, simple and clinically relevant approach in a large cohort". J. Clin. Lab. Anal. 13 (6): 273–9. doi:10.1002/(SICI)1098-2825(1999)13:6<273::AID-JCLA4>3.0.CO;2-X. PMC 6808097. PMID 10633294.
- Chua E, Clague JE, Sharma AK, Horan MA, Lombard M (October 1999). "Serum transferrin receptor assay in iron deficiency anaemia and anaemia of chronic disease in the elderly". QJM. 92 (10): 587–94. doi:10.1093/qjmed/92.10.587. PMID 10627880.
- Ananian P, Hartvigsen J, Bernard D, Le Treut YP (2005). "Serum acute-phase protein level as indicator for liver failure after liver resection". Hepatogastroenterology. 52 (63): 857–61. PMID 15966220.
External links
- http://eclinpath.com/chemistry/proteins/acute-phase-proteins/
- Acute-Phase+Proteins at the US National Library of Medicine Medical Subject Headings (MeSH)