Common bile duct
The common bile duct, sometimes abbreviated as CBD,[2] is a duct in the gastrointestinal tract of organisms that have a gallbladder. It is formed by the confluence of the common hepatic duct and cystic duct and terminates by uniting with pancreatic duct, forming the ampulla of Vater. The flow of bile from the ampulla of Vater into the duodenum is under the control of the sphincter of Oddi.
| Common bile duct | |
|---|---|
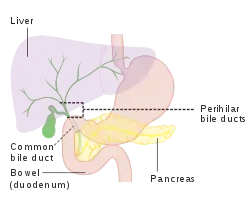 Diagram of the biliary tree showing the common bile duct | |
| Details | |
| Part of | Biliary tract |
| Identifiers | |
| Latin | ductus choledochus |
| Acronym(s) | CBD |
| MeSH | D003135 |
| TA98 | A05.8.02.013 |
| TA2 | 3103 |
| FMA | 14667 |
| Anatomical terminology | |

9. Gallbladder, 10–11. Right and left lobes of liver. 12. Spleen.
13. Esophagus. 14. Stomach. 15. Pancreas: 16. Accessory pancreatic duct, 17. Pancreatic duct.
18. Small intestine: 19. Duodenum, 20. Jejunum
21–22. Right and left kidneys.
The front border of the liver has been lifted up (brown arrow).[1]
When the sphincter of Oddi is closed, newly synthesized bile from the liver is forced into storage in the gallbladder. When open, the stored and concentrated bile (now mixed with pancreatic secretions) exits into the duodenum and takes part in digestion. This conduction of bile is the main function of the common bile duct. The hormone cholecystokinin, when stimulated by a fatty meal, promotes bile secretion by increased production of hepatic bile, contraction of the gallbladder, and relaxation of the sphincter of Oddi.
Clinical significance
Several problems can arise within the common bile duct, usually related to its obstruction. Opinions vary slightly on the maximum calibre of a normal CBD, but 6mm is one accepted upper limit of normal [3] with a further 1mm diameter allowed for each decade over 60 years.
It normally gets slightly dilated after cholecystectomy, with upper limit (95% prediction interval) being about 10 mm after a few months.[4]
On abdominal ultrasonography, the common bile duct is most readily seen in the porta hepatis (where the CBD lies anterior to the portal vein and hepatic artery). The absence of Doppler signal distinguishes it from the portal vein and hepatic artery.
 Borderline of a dilated perihilar bile duct, measuring 8 mm.
Borderline of a dilated perihilar bile duct, measuring 8 mm. Dilatation of CBD due to Ampullary tumor.
Dilatation of CBD due to Ampullary tumor.
If obstructed by a gallstone, a condition called choledocholithiasis can result.[5] In this obstructed state, the duct is especially vulnerable to an infection called ascending cholangitis. One form of treatment is a cholecystenterostomy. Rare deformities of the common bile duct are cystic dilations (4 cm), choledochoceles (cystic dilation of the ampula of Vater (3–8 cm)), and biliary atresia.
History
Obstruction of the common bile duct and related jaundice has been documented since at least since the time of Erasistratus.[6]
Additional images
 The gall-bladder and bile ducts laid open.
The gall-bladder and bile ducts laid open.
See also
- Choledochoduodenostomy - a surgical procedure to create a connection between the common bile duct (CBD) and an alternative portion of the duodenum.
References
- Standring S, Borley NR, eds. (2008). Gray's anatomy : the anatomical basis of clinical practice. Brown JL, Moore LA (40th ed.). London: Churchill Livingstone. pp. 1163, 1177, 1185–6. ISBN 978-0-8089-2371-8.
- Agabegi, Steven S.; Agabegi, Elizabeth D. (23 August 2012). Step-Up to Medicine. Lippincott Williams & Wilkins. p. 136. ISBN 9781609133603.
- Oh, Lawrence. "Common bile duct | Radiology Reference Article | Radiopaedia.org". Radiopaedia. Retrieved 2021-08-30.
- Feng, B; Song, Q (1995). "Does the common bile duct dilate after cholecystectomy? Sonographic evaluation in 234 patients". American Journal of Roentgenology. 165 (4): 859–861. doi:10.2214/ajr.165.4.7676981. ISSN 0361-803X. PMID 7676981.
- Humes, H. David (2001). Kelley's Essentials of Internal Medicine. Lippincott Williams & Wilkins. p. 229. ISBN 978-0781719377.
- Bateson, Malcolm C., ed. (1986). Gallstone Disease and its Management. Dordrecht: Springer Netherlands. p. Epidemiology (chapter). ISBN 9400941730.
- Miederer, S.; Lindstaedt, H.; Siedek, M.; Franken, Th. (1978). "Endoskopische transpapilläre Spaltung einer Choledochocele" [Endoscopic transpapillary Splitting of a choledochocele]. Deutsche Medizinische Wochenschrift (in German). 103 (5): 216–219. doi:10.1055/s-0028-1104409. PMID 631041.
External links
- Anatomy figure: 38:06-08 at Human Anatomy Online, SUNY Downstate Medical Center - "The gallbladder and extrahepatic bile ducts."
- Anatomy image:8336 at the SUNY Downstate Medical Center
- Anatomy image:7957 at the SUNY Downstate Medical Center
- liver at The Anatomy Lesson by Wesley Norman (Georgetown University) (biliarysystem)