Intensive care medicine
Intensive care medicine, also called critical care medicine, is a medical specialty that deals with seriously or critically ill patients who have, are at risk of, or are recovering from conditions that may be life-threatening.[1] It includes providing life support, invasive monitoring techniques, resuscitation, and end-of-life care.[2] Doctors in this specialty are often called intensive care physicians, critical care physicians or intensivists.
 A patient being managed in an intensive care unit | |
| Focus | Organ dysfunction, life support |
|---|---|
| Significant diseases | Respiratory failure, Organ failure, Multiorgan failure |
| Specialist | Intensive care physician Critical care physician Intensivist |
| Occupation | |
|---|---|
Occupation type | Specialty |
Activity sectors | Medicine |
| Description | |
Education required |
|
Fields of employment | Hospitals, Clinics |
Related jobs | Anesthesiologist |
Intensive care relies on multidisciplinary teams composed of many different health professionals. Such teams often include doctors, nurses, physical therapists, respiratory therapists, and pharmacists, among others.[3] They usually work together in intensive care units (ICUs) within a hospital.[1]
Scope

Patients are admitted to the intensive care unit if their medical needs are greater than what the general hospital ward can provide. Indications for the ICU include blood pressure support for cardiovascular instability (hypertension/hypotension), sepsis, post-cardiac arrest syndrome or certain cardiac arrhythmias.[4] Other ICU needs include airway or ventilator support due to respiratory compromise. The cumulative effects of multiple organ failure, more commonly referred to as multiple organ dysfunction syndrome, also requires advanced care.[4] Patients may also be admitted to the ICU for close monitoring or intensive needs following a major surgery.[5]
There are two common ICU structures: closed and open.[5] In a closed unit, the intensivist takes on the primary role for all patients in the unit.[5] In an open ICU, the primary physician, who may or may not be an intensivist, can differ for each patient.[5][6] There is increasingly strong evidence that closed units provide better patient outcomes.[7][8] Patient management in intensive care differs between countries. Open units are the most common structure in the United States, but closed units are often found at large academic centers.[5] Intermediate structures that fall between open and closed units also exist.[5]
Types of intensive care units
Intensive care is usually provided in a specialized unit of a hospital called the intensive care unit (ICU) or critical care unit (CCU). Many hospitals also have designated intensive care areas for certain specialities of medicine.[9] The naming is not rigidly standardized, and types of units are dictated by the needs and available resources of each hospital. These include:
- coronary intensive care unit (CCU or sometimes CICU) for heart disease
- medical intensive care unit (MICU)
- surgical intensive care unit (SICU)
- pediatric intensive care unit (PICU)
- neuroscience critical care unit (NCCU)
- overnight intensive-recovery (OIR)
- shock/trauma intensive-care unit (STICU)
- neonatal intensive care unit (NICU)
- ICU in the emergency department (E-ICU)[10]
Medical studies suggest a relation between ICU volume and quality of care for mechanically ventilated patients.[11] After adjustment for severity of illness, demographic variables, and characteristics of the ICUs (including staffing by intensivists), higher ICU volume was significantly associated with lower ICU and hospital mortality rates. For example, adjusted ICU mortality (for a patient at average predicted risk for ICU death) was 21.2% in hospitals with 87 to 150 mechanically ventilated patients annually, and 14.5% in hospitals with 401 to 617 mechanically ventilated patients annually. Hospitals with intermediate numbers of patients had outcomes between these extremes. ICU delirium, formerly and inaccurately referred to as ICU psychosis, is a syndrome common in intensive care and cardiac units where patients who are in unfamiliar, monotonous surroundings develop symptoms of delirium (Maxmen & Ward, 1995). This may include interpreting machine noises as human voices, seeing walls quiver, or hallucinating that someone is tapping them on the shoulder.[12] There exists systematic reviews in which interventions of sleep promotion related outcomes in the ICU have proven impactful in the overall health of patients in the ICU.[13]
History
The English nurse Florence Nightingale pioneered efforts to use a separate hospital area for critically injured patients. During the Crimean War in the 1850s, she introduced the practice of moving the sickest patients to the beds directly opposite the nursing station on each ward so that they could be monitored more closely.[14] In 1923, the American neurosurgeon Walter Dandy created a three-bed unit at the Johns Hopkins Hospital. In these units, specially trained nurses cared for critically ill postoperative neurosurgical patients.[15][14]
The Danish anaesthesiologist Bjørn Aage Ibsen became involved in the 1952 poliomyelitis epidemic in Copenhagen, where 2722 patients developed the illness in a six-month period, with 316 of those developing some form of respiratory or airway paralysis.[16] Some of these patients had been treated using the few available negative pressure ventilators, but these devices (while helpful) were limited in number and did not protect the patient's lungs from aspiration of secretions. Ibsen changed the management directly by instituting long-term positive pressure ventilation using tracheal intubation, and he enlisted 200 medical students to manually pump oxygen and air into the patients' lungs round the clock.[17] At this time, Carl-Gunnar Engström had developed one of the first artificial positive-pressure volume-controlled ventilators, which eventually replaced the medical students. With the change in care, mortality during the epidemic declined from 90% to around 25%.[18][19] Patients were managed in three special 35-bed areas, which aided charting medications and other management.
In 1953, Ibsen set up what became the world's first intensive care unit in a converted student nurse classroom in Copenhagen Municipal Hospital. He provided one of the first accounts of the management of tetanus using neuromuscular-blocking drugs and controlled ventilation.[20] The following year, Ibsen was elected head of the department of anaesthesiology at that institution. He jointly authored the first known account of intensive care management principles in the journal Nordisk Medicin, with Tone Dahl Kvittingen from Norway.[21]
For a time in the early 1960s, it was not clear that specialized intensive care units were needed, so intensive care resources were brought to the room of the patient that needed the additional monitoring, care, and resources. It became rapidly evident, however, that a fixed location where intensive care resources and dedicated personnel were available provided better care than ad hoc provision of intensive care services spread throughout a hospital. In 1962, in the University of Pittsburgh, the first critical care residency was established in the United States. In 1970, the Society of Critical Care Medicine was formed.[22]
Monitoring
Monitoring refers to various tools and technologies used to obtain information about a patient's condition. These can include tests to evaluate blood flow and gas exchange in the body, or to assess the function of organs such as the heart and lungs.[23] Broadly, there are two common types of monitoring in the ICU: noninvasive and invasive.[1]
Noninvasive monitoring
Noninvasive monitoring does not require puncturing the skin and usually does not cause pain. These tools are more inexpensive, easier to perform, and faster to result.[1]
- Vital signs which includes heart rate, blood pressure, breathing rate, body temperature
- Echocardiogram to evaluate the function and structure of the heart
- Electroencephalography (EEG) to assess electrical activity of the brain
- Electrocardiogram to detect abnormal heart rhythms, electrolyte disturbances, and coronary blood flow
- Pulse oximetry for monitoring oxygen levels in the blood
- Thoracic electric bioimpedance (TEB) cardiography to monitor fluid status and heart function
- Ultrasound to evaluate internal structures including the heart, lungs, gallbladder, liver, kidneys, bladder, and blood vessels
Invasive monitoring
Invasive monitoring generally provides more accurate measurements, but these tests may require blood draws, puncturing the skin, and can be painful or uncomfortable.[1]
- Arterial line to directly monitor blood pressure and obtain arterial blood gas measurements
- Blood draws or venipucture to monitor various blood components as well as administer therapeutic treatments
- Intracranial pressure monitoring to assess pressures inside the skull and on the brain
- Intravesicular manometry (bladder pressure) measurements to assess for intra-abdominal pressure
- Central line and peripherally inserted central catheter (PICC) lines for drug infusions, fluids or total parenteral nutrition
- Bronchoscopy to look at lungs and airways and sample fluid within the lungs
- Pulmonary artery catheter to monitor the function of the heart, blood volume, and tissue oxygenation
Procedures and treatments
Intensive care usually takes a system-by-system approach to treatment.[9] In alphabetical order, the nine key systems considered in the intensive care setting are: cardiovascular system, central nervous system, endocrine system, gastro-intestinal tract (and nutritional condition), hematology, integumentary system, microbiology (including sepsis status), renal (and metabolic), and respiratory system. As such, the nine key systems are each considered on an observation–intervention–impression basis to produce a daily plan.
Cardiovascular
- Temporary cardiac pacing catheters for atrial, ventricular, or dual-chamber pacing
- Intra-aortic balloon pumping to stabilize patients with cardiogenic shock
- Ventricular assist device to aid in the function of the left ventricle, commonly in patients with advanced heart failure
Gastro-intestinal tract
- Feeding tube for artificial nutrition
- Nasogastric intubation can be used to deliver artificial nutrition, but can also be used to remove stomach and intestinal contents
- Peritoneal aspiration and lavage to sample fluid in the abdominal cavity
Renal
Respiratory
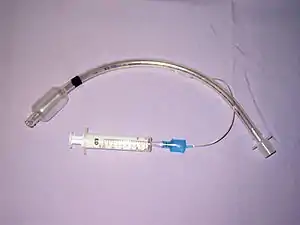
- Mechanical ventilation to assist breathing and oxygenation through an endotracheal tube, tracheotomy (invasive) or mask, helmet (non-invasive).
- Thoracentesis or tube thoracostomy to remove fluid or air in the pleural cavity
Drugs
A wide array of drugs including but not limited to: inotropes, sedatives, broad spectrum antibiotics and analgesics.
Common complications in the ICU
Intensive care units are associated with increased risk of various complications that may lengthen a patient's hospitalization.[9] Common complications in the ICU include:
- Acute renal failure
- Catheter-associated blood stream infection
- Catheter-associated urinary tract infection
- Delirium
- Gastrointestinal bleeding
- Pressure ulcer
- Venous thromboembolism
- Ventilator-associated pneumonia
- Ventilator-induced barotrauma
- Death
Training
ICU care requires more specialized patient care; this need has led to the use of a multidisciplinary team to provide care for patients.[4][1] Staffing between Intensive care units by country, hospital, unit, or institution.[5]
Medicine
Critical care medicine is an increasingly important medical specialty. Physicians with training in critical care medicine are referred to as intensivists.[26]
Most medical research has demonstrated that ICU care provided by intensivists produces better outcomes and more cost-effective care.[27] This has led the Leapfrog Group to make a primary recommendation that all ICU patients be managed or co-managed by a dedicated intensivist who is exclusively responsible for patients in one ICU.
In Australia
In Australia, the training in intensive care medicine is through College of Intensive Care Medicine.
In the United Kingdom
In the UK, doctors can only enter intensive care medicine training after completing two foundation years and core training in either emergency medicine, anaesthetics, acute medicine or core medicine. Most trainees dual train with one of these specialties; however, it has recently become possible to train purely in intensive care medicine. It has also possible to train in sub-specialties of intensive care medicine including pre-hospital emergency medicine.
In the United States
In the United States, the specialty requires additional fellowship training for physicians having completed their primary residency training in internal medicine, pediatrics, anesthesiology, surgery or emergency medicine. US board certification in critical care medicine is available through all five specialty boards. Intensivists with a primary training in internal medicine sometimes pursue combined fellowship training in another subspecialty such as pulmonary medicine, cardiology, infectious disease, or nephrology. The American Society of Critical Care Medicine is a well-established multi professional society for practitioners working in the ICU including nurses, respiratory therapists, and physicians.
Intensive care physicians have some of the highest percentages of physician burnout among all medical specialties, at 48 percent. [28]
Nursing
Nurses that work in the critical care setting are typically registered nurses.[5] Nurses may pursue additional education and training in critical care medicine leading to certification as a CCRN by the American Association of Critical Care Nurses a standard that was begun in 1975.[29] These certifications became more specialized to the patient population in 1997 by the American Association of Critical care Nurses, to include pediatrics, neonatal and adult.[29]
Nurse practitioners and physician assistants
Nurse practitioners and physician assistants are other types of non-physician providers that care for patients in ICUs.[4] These providers have fewer years of in-school training, typically receive further clinical on the job education, and work as part of the team under the supervision of physicians.
Pharmacists
Critical care pharmacists work with the medical team in many aspects, but some include, monitoring serum concentrations of medication, past medication use, current medication use, and medication allergies.[6] Their typically round with the team, but it may differ by institution.[6] Some pharmacist after attaining their doctorate or pharmacy may pursue additional training in a postgraduate residency and become certified as critical care pharmacists.[6] Pharmacists help manage all aspects of drug therapy and may pursue additional credentialing in critical care medicine as BCCCP by the Board of Pharmaceutical Specialties. Many critical care pharmacists are a part of the multi-professional Society of Critical Care Medicine.[6] Inclusion of pharmacist decreases drug reactions and poor outcomes for patients.[4]
Registered dietitians
Nutrition in intensive care units presents unique challenges due to changes in patient metabolism and physiology while critically ill.[30] Critical care nutrition is rapidly becoming a subspecialty for dieticians who can pursue additional training and achieve certification in enteral and parenteral nutrition through the American Society for Parenteral and Enteral Nutrition (ASPEN).
Respiratory therapists
Respiratory therapists often work in intensive care units to monitor how well a patient is breathing.[31] Respiratory therapists may pursue additional education and training leading to credentialing in adult critical care (ACCS) and neonatal and pediatric (NPS) specialties. These therapists have been trained to monitor a patient's breathing, provide treatments to help their breathing and evaluate for respiratory improvement.[31] They may be involved in emergency care like managing an airway, humidification of oxygen, administering diagnostic test, invasive or non-invasive mechanical ventilation management, training patients weaning the ventilator, aerosol therapy, inhaled Nitric oxide therapy, artery blood gas analysis and providing physiotherapy.[32]
Ethical and medicolegal issues
Economics
In general, it is the most expensive, technologically advanced and resource-intensive area of medical care. In the United States, estimates of the 2000 expenditure for critical care medicine ranged from US$19–55 billion. During that year, critical care medicine accounted for 0.56% of GDP, 4.2% of national health expenditure and about 13% of hospital costs.[33] In 2011, hospital stays with ICU services accounted for just over one-quarter of all discharges (29.9%) but nearly one-half of aggregate total hospital charges (47.5%) in the United States. The mean hospital charge was 2.5 times higher for discharges with ICU services than for those without.[34]
See also
Notes
- Civetta, Taylor, & Kirby's critical care. Gabrielli, Andrea., Layon, A. Joseph., Yu, Mihae., Civetta, Joseph M., Taylor, Robert W. (Robert Wesley), 1949-, Kirby, Robert R. (4th ed.). Philadelphia: Lippincott Williams & Wilkins. 2009. ISBN 978-0-7817-6869-6. OCLC 253189100.
{{cite book}}: CS1 maint: others (link) - "About Intensive Care | the Faculty of Intensive Care Medicine".
- "Critical Care Medicine Specialty Description". American Medical Association. Retrieved 24 October 2020.
- Basics of anesthesia. Pardo, Manuel Jr., 1965-, Miller, Ronald D., 1939-, Preceded by (work): Miller, Ronald D., 1939- (Seventh ed.). Philadelphia, PA. 26 June 2017. ISBN 9780323401159. OCLC 989157369.
{{cite book}}: CS1 maint: others (link) - Principles of critical care. Hall, Jesse B.,, Schmidt, Gregory A.,, Kress, John P. (Fourth ed.). New York. 2 June 2015. ISBN 9780071738811. OCLC 906700899.
{{cite book}}: CS1 maint: others (link) - Evidence-based practice of critical care. Deutschman, Clifford S.,, Neligan, Patrick J. (Third ed.). Philadelphia, PA. 29 August 2019. ISBN 978-0-323-64069-5. OCLC 1118693260.
{{cite book}}: CS1 maint: others (link) - Manthous, CA; Amoateng-Adjepong, Y; Al-Kharrat, T; Jacob, B; Alnuaimat, HM; Chatila, W; Hall, JB (1997). "Effects of a medical intensivist on patient care in a community teaching hospital". Mayo Clinic Proceedings (Abstract). 72 (5): 391–9. doi:10.4065/72.5.391. PMID 9146680.
- Hanson CW; Deutschman, CS; Anderson, HL; Reilly, PM; Behringer, EC; Schwab, CW; Price, J (1999). "Effects of an organized critical care service on outcomes and resource utilization: a cohort study". Critical Care Medicine (Abstract). 27 (2): 270–4. doi:10.1097/00003246-199902000-00030. PMID 10075049.
- Critical care medicine : principles of diagnosis and management in the adult. Parrillo, Joseph E., Dellinger, R. Phillip. (3rd ed.). Philadelphia, PA: Mosby Elsevier. 2008. ISBN 978-0-323-07095-9. OCLC 324998024.
{{cite book}}: CS1 maint: others (link) - Yim, KM; Ko, HF; Yang, Marc LC; Li, TY; Ip, S; Tsui, J (20 June 2018). "A paradigm shift in the provision of improved critical care in the emergency department". Hong Kong Medical Journal. 24 (3): 293–297. doi:10.12809/hkmj176902. PMID 29926792.
- Kahn, JM; Goss, CH; Heagerty, PJ; Kramer, AA; O'Brien, CR; Rubenfeld, GD (2006). "Hospital volume and the outcomes of mechanical ventilation" (PDF). The New England Journal of Medicine. 355 (1): 41–50. doi:10.1056/NEJMsa053993. PMID 16822995. S2CID 26611094. Archived from the original (PDF) on 29 July 2020.
- Nolen-Hoeksema, Susan. "Neurodevelopmental and Neurocognitive Disorders." (Ab)normal Psychology. Sixth ed. New York City: McGraw-Hill Education, 2014. 314. Print.
- Flannery, Alexander H.; Oyler, Douglas R.; Weinhouse, Gerald L. (December 2016). "The Impact of Interventions to Improve Sleep on Delirium in the ICU". Critical Care Medicine. 44 (12): 2231–2240. doi:10.1097/ccm.0000000000001952. ISSN 0090-3493. PMID 27509391. S2CID 24494855.
- Vincent, Jean-Louis (2013). "Critical care – where have we been and where are we going?". Critical Care. 17 (S1): S2. doi:10.1186/cc11500. ISSN 1364-8535. PMC 3603479. PMID 23514264.
- Miller's Anesthesia. Gropper, Michael A., 1958-, Miller, Ronald D., 1939- (Ninth ed.). Philadelphia, PA. 7 October 2019. ISBN 978-0-323-61264-7. OCLC 1124935549.
{{cite book}}: CS1 maint: others (link) - Woollam, C. H. M. (1976). "The development of apparatus for intermittent negative pressure respiration (2) 1919–1976, with special reference to the development and uses of cuirass respirators". Anaesthesia. 31 (5): 666–685. doi:10.1111/j.1365-2044.1976.tb11849.x. ISSN 0003-2409. PMID 779520.
- Reisner-Sénélar, Louise (2011). "The Birth of Intensive Care Medicine: Björn Ibsen's Records" Archived 6 October 2012 at the Wayback Machine (PDF format).Intensive Care Medicine. Retrieved 2 October 2012.
- US US2699163A, Engström, Carl Gunnar, "Respirator", issued 1951-06-25
- Engstrom, C.-G. (1954). "Treatment of Severe Cases of Respiratory Paralysis by the Engstrom Universal Respirator". BMJ. 2 (4889): 666–669. doi:10.1136/bmj.2.4889.666. ISSN 0959-8138. PMC 2079443. PMID 13190223.
- Berthelsen, P.G.; Cronqvist, M. (2003). "The first intensive care unit in the world: Copenhagen 1953". Acta Anaesthesiologica Scandinavica. 47 (10): 1190–1195. doi:10.1046/j.1399-6576.2003.00256.x. ISSN 0001-5172. PMID 14616314. S2CID 40728057.
- Ibsen, B; Kvittingen, T.D. (1958). "Arbejdet på en Anæsthesiologisk Observationsafdeling" [Work in an Anaesthesiological Observation Unit]. Nordisk Medicin (in Danish). 60 (38): 1349–55. PMID 13600704.
- history reference: Brazilian Society of Critical Care SOBRATI Video:ICU History Historical photos
- Huygh J (December 2016). "Hemodynamic monitoring in the critically ill: an overview of current cardiac output monitoring methods". F1000Research. 5: 2855. doi:10.12688/f1000research.8991.1. PMC 5166586. PMID 28003877.
- Doiron, Katherine A.; Hoffmann, Tammy C.; Beller, Elaine M. (March 2018). "Early intervention (mobilization or active exercise) for critically ill adults in the intensive care unit". The Cochrane Database of Systematic Reviews. 3 (12): CD010754. doi:10.1002/14651858.CD010754.pub2. ISSN 1469-493X. PMC 6494211. PMID 29582429.
- Sommers, Juultje; Engelbert, Raoul HH; Dettling-Ihnenfeldt, Daniela; Gosselink, Rik; Spronk, Peter E; Nollet, Frans; van der Schaaf, Marike (November 2015). "Physiotherapy in the intensive care unit: an evidence-based, expert driven, practical statement and rehabilitation recommendations". Clinical Rehabilitation. 29 (11): 1051–1063. doi:10.1177/0269215514567156. ISSN 0269-2155. PMC 4607892. PMID 25681407.
- "What – or Who -- Is an Intensivist?". Healthcare Financial Management Association. Archived from the original on 27 September 2009.
- "Association between Critical Care Physician Management and Patient Mortality in the Intensive Care Unit". Annals of Internal Medicine. 3 June 2008. Volume 148, Issue 11. pp. 801–809.
- "Physician burnout: It's not you, it's your medical specialty". American Medical Association. 3 August 2018. Retrieved 7 July 2020.
- Pediatric critical care. Fuhrman, Bradley P.,, Zimmerman, Jerry J.,, Clark, Robert S. B., 1962-, Relvas, Monica S.,, Thompson, Ann E.,, Tobias, Joseph D. (Fifth ed.). Philadelphia, PA. 8 December 2016. ISBN 978-0-323-37839-0. OCLC 966447977.
{{cite book}}: CS1 maint: others (link) - Current surgical therapy. Cameron, John L.,, Cameron, Andrew M. (Andrew MacGregor) (12th ed.). Philadelphia, PA. 2017. ISBN 978-0-323-37691-4. OCLC 966447396.
{{cite book}}: CS1 maint: others (link) - Total burn care. Herndon, David N. (Fifth ed.). Edinburgh. 10 October 2017. ISBN 978-0-323-49742-8. OCLC 1012122839.
{{cite book}}: CS1 maint: others (link) - Gomella, Leonard G. (2007). Clinician's pocket reference. Haist, Steven A., University of Kentucky. College of Medicine. (11th ed.). New York: McGraw-Hill Companies, Inc. ISBN 978-0-07-145428-5. OCLC 85841308.
- Halpern, Neil A.; Pastores, Stephen M.; Greenstein, Robert J. (June 2004). "Critical care medicine in the United States 1985–2000: An analysis of bed numbers, use, and costs". Critical Care Medicine. 32 (6): 1254–1259. doi:10.1097/01.CCM.0000128577.31689.4C. PMID 15187502. S2CID 26028283.
- Barrett ML; Smith MW; Elizhauser A; Honigman LS; Pines JM (December 2014). "Utilization of Intensive Care Services, 2011". HCUP Statistical Brief #185. Rockville, MD: Agency for Healthcare Research and Quality. PMID 25654157.
References
- Intensive Care Medicine by Irwin and Rippe
- Civetta, Taylor, and Kirby's Critical Care
- The ICU Book by Marino
- Procedures and Techniques in Intensive Care Medicine by Irwin and Rippe
- Halpern NA, Pastores SM, Greenstein RJ (June 2004). "Critical care medicine in the United States 1985–2000: an analysis of bed numbers, use, and costs". Critical Care Medicine. 32 (6): 1254–9. doi:10.1097/01.CCM.0000128577.31689.4C. PMID 15187502. S2CID 26028283..
- History references:
- Society of Critical Care Medicine
- Reynolds, H.N.; Rogove, H.; Bander, J.; McCambridge, M.; et al. (December 2011). "A working lexicon for the tele-intensive care unit: We need to define tele-intensive care unit to grow and understand it" (PDF). Telemedicine and e-Health. 17 (10): 773–783. doi:10.1089/tmj.2011.0045. hdl:2027.42/90470. PMID 22029748.
- Olson, Terrah; Brasel, Karen; Redmann, Andrew; Alexander, G.; Schwarze, Margaret (January 2013). "Surgeon-Reported Conflict With Intensivists About Postoperative Goals of Care". JAMA Surgery. 148 (1): 29–35. doi:10.1001/jamasurgery.2013.403. PMC 3624604. PMID 23324837.
Further reading
- Lois Reynolds; Tilli Tansey, eds. (2011). History of British Intensive Care, c. 1950–c. 2000. Wellcome Witnesses to Contemporary Medicine. History of Modern Biomedicine Research Group. ISBN 978-0-902238-75-6. Wikidata Q29581786..
External links
- College of Intensive Care Medicine - Australia and New Zealand
- Australia and New Zealand Intensive Care Society
- Society of Critical Care Medicine
- Veterinary Emergency And Critical Care Society
- ESICM: European Society of Intensive Care Medicine
- ESPNIC: The society for paediatric and neonatal intensive care healthcare professionals in Europe
- UK Intensive Care Society
- Scottish Intensive Care Society
- Hong Kong Society of Critical Care Medicine
- Chinese Society of Critical Care Medicine
- Taiwan Society of Critical Care Medicine
- From Iron Lungs to Intensive Care, Royal Institution debate, February 2012