Gluten-sensitive enteropathy–associated conditions
Gluten-sensitive enteropathy–associated conditions are comorbidities or complications of gluten-related gastrointestinal distress (that is, gluten-sensitive enteropathy or GSE). GSE has key symptoms typically restricted to the bowel and associated tissues; however, there are a wide variety of associated conditions. These include bowel disorders (diarrhoea, constipation, irritable bowel), eosinophilic gastroenteritis and increase with coeliac disease (CD) severity. With some early onset and a large percentage of late onset disease, other disorders appear prior to the celiac diagnosis[1] or allergic-like responses (IgE or IgA, IgG) markedly increased in GSE. Many of these disorders persist on a strict gluten-free diet (GF diet or GFD), and are thus independent of coeliac disease after triggering. For example, autoimmune thyroiditis is a common finding with GSE.
However, GSEs' association with disease is not limited to common autoimmune diseases. Coeliac disease has been found at increased frequency on followup to many autoimmune diseases, some rare. Complex causes of autoimmune diseases often demonstrates only weak association with coeliac disease. The frequency of GSE is typically around 0.3 to 1% and lifelong risk of this form of gluten sensitivity increases in age, possibly as high as 2% for people over 60 years of age.[2] This coincides with the period in life when late-onset autoimmune diseases also rise in frequency.
Genetic studies indicate that coeliac disease genetically links to loci shared by linkage with other autoimmune diseases.[3] These linkages may be coincidental with how symptomatic disease is selected from a largely asymptomatic population.
Associated blood disorders
Deficiencies
Avitaminosis. Avitaminosis caused by malabsorption in GSE can result in decline of fat soluble vitamins and vitamin B, as well as malabsorption of essential fatty acids. This can cause a wide variety of secondary problems. Hypocalcinemia is also associated with GSE.[4] In treated GSE, the restrictions on diet as well as reduced absorption as a result of prolonged damage may result in post treatment deficiencies.[5]
- Vitamin A – Poor absorption of vitamin A has been seen in coeliac disease.[6] and it has been suggested that GSE-associated cancers of the esophagus may be related to vitamin A deficiency[7][8]
- Folate deficiency – Folate deficiency is believed to be primary to the following secondary conditions:
- Megaloblastic anemia
- Calcification of brain channels – epilepsy, dementia, visual manifestations.
- B6 deficiency. Vitamin B6 deficiency can result in neuropathies and increases in pain sensitivity.[9] may explain some of the peripheral neuropathies, pain and depression associated with GSE.[10]
- B12 deficiency
- Vitamin D deficiency. Vitamin D deficiency can result in osteopenia and osteoporosis
- Vitamin K – Coeliac disease has been identified in patients with a pattern of bleeding that treatment of vitamin K increased levels of prothrombin.[12]
- Vitamin E – deficiency of vitamin E can lead to CNS problems[13] and possibly associated with myopathy[14]
Mineral deficiencies. GSE is associated with the following mineral deficiencies:
- Calcium – Hypocalcemia[11] causing Oesteopenia
- Magnesium – hypomagnesemia,[15] may lead to parathyroid abnormalities.
- Iron – Iron deficiency anemia
- Phosphorus – hypophosphatemia,[16] causing Oesteopenia
- Zinc – Zinc deficiencies[17] are believed to be associated with increased risk of Esophagus Carcinoma[8]
- Copper – deficiency[17]
- Selenium – deficiency[18] – Selenium and Zinc deficiencies may play a role increasing risk of cancer.[19] Selenium deficiency may also be an aggravating factor for autoimmune hyperthyroidism (Graves disease).[20]
Blood factors
Anemia
Megaloblastic anemia (MA) is associated with GSE and is believed to be the result of B12 and folate deficiency.[23] In GSE, it appears to be associated with the IgA-less phenotype.[24] Unlike other forms of megaloblastic anemia, GSEA MA is not a form of autoimmune gastritis.[25]
Pernicious anemia (PA). Pernicious anemia is associated with GSE and is believed to result primarily from malabsorption phenomena.[23]
Iron-deficiency anemia. Iron-deficiency anemia (IDA) may be the only symptom for CD,[26] detected in subclinical CD[27] and is accompanied by a decrease in serum ferritin levels.[28] This can cause addition problems (see:symptoms of IDA and certain conditions like such as Paterson-Brown Kelly (Plummer-Vinson).[29] Whereas IDA is corrected on GF diet, refractory disease or gluten-sensitive malignancies can cause persistent IDA.[30]
Clotting abnormalities
Thromboembolism is a well-described complication of IBD, with a clinical incidence of up to 6% and a three-fold higher risk of disease,[31][32] and the Factor V Leiden mutation further increases the risk of venous thrombosis.[33] Recent studies describe the co-occurrence between coeliac disease, in which IBD is common in venous thrombosis.[34][35]
Dermatitis
A study of patients with dermatitis herpetiformis or coeliac disease revealed significantly more gluten in the blood than controls.[36] This increases the risk of asthma, anaphylaxis and dermatological conditions.
Dermatitis herpetiformis
Triticeae glutens are the primary cause of dermatitis herpetiformis (DH). Epidermal transglutaminase (eTG) is related to tTG and is the autoantigen of DH. It appears that all DH patients have or are susceptible on wheat ingestion to CD. Within CD DH is relatively rare or underdiagnosed with about 5% of patients having DH. Aphthous stomatitis is a common mouth lesion found with celiac disease.
Atopy, urticaria, eczema
Chronic urticaria has been seen in a few cases of CD.[37] and are likely the result of fortuitous allergies to wheat, or allergies secondary to GSE. Atopy disorders have been found to be more common in celiacs and in first degree relatives.[38] Celiac disease is associated with a number of epidermal conditions including Psoriasis[39][40]
Rare dermatitis
Prurigo nodularis. Prurigo nodularis has been identified with coeliac disease.[41][42] Rothmund-Thomson syndrome. Rothmund-Thomson syndrome, or poikiloderma congenitale, is a rare disorder, generally attributed to mutations of the RECQL4 helicase gene on 8q24 with features that include photosensitivity and poikilodermatous skin changes, etc., and has been reported in one celiac patient.[43]
Alopecia areata
GSE has been found to be associated with alopecia areata (patchy baldness)[44] whereas regrowth did not necessarily occur on a gluten free diet.[45][46]
Endocrine disorders
Autoimmune thyroidosis
[Section under construction] Grave's Disease, Hashimoto's thyroiditis. Grave's disease and Hashimoto's thyroiditis are greatly increased in patients with CD.[47] Grave's disease is an autoimmune hyperthyroidism, as GSE is a potentiator for autoimmune disease, but GD is more commonly found and avitaminosis of selenium and other minerals may be a factor in this increase.
Diabetes
Type 1 (Juvenile onset). The incidence of juvenile Type 1 Diabetes (T1D) is about 1:500 in the U.S. population, and is the result of autoimmune damage to the Islets of Langerhans cells in the pancreas. The level of adult onset T1D plus ambiguous T1D/T2D is unknown. It is unclear how large a role Triticeae has in T1D, which also shows strong linkage to DQ2.5 and DQ8. Childhood (male) Type 1 diabetes increases the risk for GSE and vice versa[48] and it now appears that GSE precedes T1D in many cases[49] and an active search for coeliac disease in early juvenile diabetes patients revealed that GF diet resulted in some improvements.[50] A high frequency of diabetes patients have anti-transglutaminase antibodies[51] along with increased levels of gluten specific T-cells in T1D patients. From an evolutionary point of view it is difficult to explain the high association of T1D and DQ2.5 given negatively selective nature of the disease in NW European population given the number of studies suggesting that the "Super B8" haplotypes has been under positive selection, and appears to be the most characteristic HLA type in NW Europeans indicating an advanced natural history of the haplotype. A T. aesitivum storage globulin, Glb-1 (locus), was identified that is similar to the hypersensitizing peanut protein Ara h 1 and other known plant hypersensitizing proteins. Antibodies to this protein correlated with levels of lymphocyte infiltration into Islet regions of the pancreas.[52] Gastrointestinal viruses may play a role.[53][54][55][56]
Addison's disease
Studies from Sweden suggest that persons with Coeliac disease are 11 times more likely to have Addison's disease (primary adrenal insufficiency) relative to the normal population.[57]
Infertility
GSE can result in high risk pregnancies[58] and infertility. Some infertile women have GSE and iron deficiency anemia[59] others have zinc deficiency[60] and birth defects may be attributed to folic acid deficiencies. It has also been found to be a rare cause of amenorrhea.[61]
Gastrointestinal diseases
While GI disease is one of the major symptoms of GSE that are characterized by increased levels of IgA/IgG to food proteins,[62] many conditions like chronic constipation and irritable bowel disease persist after GF diet. Some of this may be due to persistent undetected food allergies, increased sensitivity of the damaged gut, or problems masked by GSE itself.
Irritable bowel (IBS)
In diarrhea dominant IB is a common symptom of GSE, increased celiac disease-associated serum IgG was found in treated and untreated CD patients. The IgG was most common in untreated patients with more active DQ2 expression that dropped on GF diet.[63] Some irritable bowel can be the result of other food intolerances, such as casein intolerance, lactose intolerance, or intolerances to non-dextrose sugars in other foods. It can also be result of overgrowth of yeast or bacteria as a result of excesses of unabsorbed nutrients. IB may not resolve on GF diet and may become more severe in rare cases because it may not have initially been directly linked to gluten consumption.
Inflammatory bowel disease (IBD)
A recent study of inflammatory bowel disease and Coeliac disease found that anti-tTG was increased in inflammatory bowel disease although most cases were not clinical CD. IBD was increased 10 fold in coeliac disease.[64] Inflammatory bowel disease consists of Crohn's disease, ulcerative colitis and microscopic colitis.
Gastroesophageal reflux disease
Gastroesophageal reflux disease (GERD) is the indirect result of many factors and some autoimmune diseases like schleroderma. GSE can cause inflammation and delayed gastric emptying, which can persist through most of the sleeping hours causing GERD. GSE is associated with an increase of food allergies, in some patients this can cause diarrhea, but in others constipation. In some patients, food allergies and GERD are an apparent symptom of GSE, but these allergies and GERD often persist on a GF diet. While GERD associated with GSE can be treated with acid blockers, it is most effectively treated with proper eating habits and elimination diet. The more powerful acid blockers (omeprazole, esomeprezole) can interfere with calcium adsorption and can aggravate preexisting hypocalcaemia and hypomagnesemia, which are more common GSE[65]
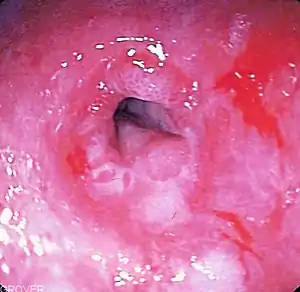
Eosinophilic oesophagitis
A high proportion of children in Italy who were diagnose with eosinophilic oesophagitis were found to have coeliac disease.[66] All patients appeared to improve on either a gluten-free or allergen free diet.
Diseases of the pancreas, gall bladder, bile duct
Primary biliary cirrhosis. CD is prevalent in primary biliary cirrhosis (PBC).[67][68] In PBC anti-mitochondrial antibodies are directed toward 3 mitochondrial autoantigens (pyruvate dehydrogenase, oxoglutarate dehydrogenase, branched-chain alpha-keto acid dehydrogenase), 2 or more nuclear proteins (nucleoporin 210kDa, nucleoporin 62kDa, centromere protein, and sp100), and 57% of acute liver failure patients have anti-transglutaminase antibodies.
Cholangitis. CD also found at higher than expected frequencies in autoimmune cholangitis and primary sclerosing cholangitis.[68] CD is frequently linked to pancreatitis but also to papillary stenosis[69] and, in India, tropical calcific pancreatitis appears also to be associated with CD.[70]
Neurological disorders
Neuropathies tend to be associated with late-onset celiac disease. Dementia and ataxia appear to be more common. A recent study of children with neuropathies revealed no increase of CD in early-onset neuropathies.[71] Although many studies link CD to various neuropathies such as migraine, encephalopathy, chorea, brain stem dysfunction, myelopathy, mononeuritis multiplex, Guillain–Barré-like syndrome, and antiganglioside-positive neuropathy with antibodies, strong associations remain largely unconfirmed in epidemiologic studies.[72] A recent study looking for changes in the physiology of the brain found regional cerebral hypoperfusion in 73% of untreated CD.[73] The calcification of channels at the surface of the brain appears to be a leading phenomenon associated with migraine, visual, auditory, schizophrenia, epilepsy, dementia. The problem is that while these are found increased in GSE, the cause of these calcifications is unclear and this may extend beyond GSE to other immunological or allergic phenomena. A 2007 study in Sweden of 14,000 GSE patients revealed no association of CD with multiple sclerosis, Parkinson's disease, Alzheimer's disease, hereditary ataxia, ataxia (the symptom), Huntington's disease, myasthenia gravis, or spinal muscular atrophy, but prior polyneuropathy was associated with subsequent CD.[74] However, a 2009 study of myasthenics revealed that 1 in 23 had high levels of anti-transglutaminase.[75]
Peripheral neuropathies
Peripheral neuropathies are greatly increased in people who have GSE. In clinical CD there is an obvious reason; avitaminosis and the inability to adsorb essential fatty acids and vitamins can lead to nervous system problems, including sensitivity of the peripheral nervous system. In addition to these problems there are a number or rare autoimmune conditions, secondary autoimmunities, such as fibromyalgia that are more frequent in GSE than in the normal population. Gulliane-Barre syndrome is associated with peripheral neuropathies, and it has been found that anti-ganglioside autoantibodies take part in the binding to axons and schwann cells. Antibodies to these gangliosides have been found elevated in coeliac disease[76]
Ataxia
A sizable fraction of individuals who have gluten ataxia have signs of GSE (either CD or elevated intraepitheal lymphocytes) and ataxia is a common symptom in GSE.[77] Studies of clinically undefinable ataxia generally had higher proportion of late onset gait ataxia, mild upper limb symptoms, and evidence of peripheral neuropathy, questions were raised about the specificity of testing and false positives. Patients with ataxia and CD have antibodies that react with Purkinje fibers but is restricted to the anti-gliadin IgA/IgG.[78] A recent Swedish study of 14,000 registered celiacs showed no association of GSE with Ataxia.[74]
Dementia and epilepsy
Epilepsy has been noticed in a sampling of coeliac disease patients.[79] One prime example is calcium channel obstruction in the brain and dementia.[80][81] There is a growing body of evidence suggesting that subclinical cases in older adults will typically progress toward dementia,[82] a large number of studies in Italy and Spain have documented earlier onset cases, though the autoimmune condition is not known, folic acid malabsorption may be the cause.
Visual and auditory disturbances
According to recent studies, calcifications of channels seen in dementia can also occur in specific brain areas such as the visual complex in the occipital lobe. Such calcium channel blockages can cause visual problems or partial field hallucinations (Paroxysmal visual manifestations).[83] Other papers show a link between migraine, visual aura and cerebral calcifications.[84] Disturbances may be followed by convulsions and associated with gastrointestinal phenomena.
White matter lesions
Ten (of 75) young patients had neurologic findings such as febrile seizures, single generalized seizures, mild ataxia, and muscular hypotonia with retarded motor development, but magnetic resonance imaging detected unilateral and bilateral T2-hyperintensive white-matter lesions in 15 patients (20%)[85]
Depression
Depression in GSE has several causes; in the more severe CD, depression can be the result of lower vitamin adsorption[10] and essential fatty acid adsorption (see section on autism). Depression and anger may also be the result of lower quality of life issues as a result of gluten-free diet.[86] Depression appears to persist on gluten free diet in a sizable fraction of GSE.[87] Elevated anger has been noted also with GSE.
Anxiety
Anxiety is a common feature of GSE; treatment on a gluten-free diet is effective at reducing anxiety, some aspect of which may be due to malabsorption phenomena and cytokine activity (i.e. constant stress).[87]
Fibromyalgia
Fibromyalgia was found in 9% of adult patients relative to 0.03% in the general population with a link common to IBD.[88] Concurrent IBS is found in 30% to 70%. Small intestinal bacterial overgrowth is associated is common with a transient response to antimicrobial therapy.[89]
Chronic fatigue
Chronic fatigue associated with GSE is a systemic disorder, however there are neurological components that are especially manifest in blood deficiencies like avitaminosis, amineralosis and anemia. Reduced iron and the lack of vitamins folate, B6, B12 and malabsorption of essential fatty acids can cause depression and chronic fatigue.[90] Anti-gliadin antibodies correlate with higher risk for chronic-fatique when no clinical finding of CD is present.[91] While fatigue is reduced on gluten-free diet, bouts of depression can become worse. [90]
Connective tissue disorders
Arthritis
Some instance of arthritis with small bowel villous atrophy have been found to resolve on gluten free diet,[92] and anti-connective tissue antibodies have been found in increased levels in celiac disease.[93] Anti-rheumatoid factor antibodies are also increased.[94] In addition, cross-reactive anti-beef-collagen antibodies (IgG) may explain some rheumatoid arthritis (RA) incidences.[95] Although the presence of anti-beef collagen antibodies does not necessarily lead to RA, the RA association with Triticeae consumption is secondary to GSE and involves DRB1*0401/4 linkages to DQ8[96] and is debatable. In one instance rheumatoid arthritis was tied directly to refractory disease.[97]
Still's disease
Still's disease (AOSD) is a rheumatic disorder of unknown etiology characterized by a triad of fever, polyarthritis and evanescent rash. An idiopathic case has been reported with celiac disease.[98]
Myositis
Some myopathies may be the indirect result of malabsorption of fat soluble vitamins such as vitamin E.[14]
GSEA Nephritis
Celiac disease is associated with immune complex glomerulonephritis.[101] Anti-gliadin IgA antibodies are found also more commonly in patients with IgA Nephropathy. The paper finds a link between GSE and IgA Nephropathy, but not between CD and Nephropathy.[102] Calcium oxalate correlates with severity of fat malabsorption in celiac disease.[103][104]
Precancerous states
CD is associated with two grades of disease linked precancerous states. This condition is known as refractory celiac disease (RCD), defined as malabsorption due to gluten-related enteropathy (villous atrophy or elevated intraepitheal lymphocytes) after initial or subsequent failure of a strict gluten-free diet (usually 1 year) and after exclusion of any disorder mimicking coeliac disease.[105][106]
- RCD 1 involves precancerous tissues in which transformed T-cells continue to produce a response even though gluten is no longer present.[107] Some RCD1 patients have been treated successfully with immunosuppressants (azathioprine, prednisone) when caught early.[106] Elemental diet (proteins digested to amino acids) seems to be an effective alternative diet,[108] indicating other proteins are stimulating the IEL. 5 year viability is high when treated. DQ representation is similar to non-RCD celiacs.
- RCD 2 involves neoplastic tissues that the lack of surface expression of usual T-cell markers.[109]
- Increased expression of: Intracytoplasmic CD3e, Surface CD103
- Decreased expression of: CD8, CD4, TCR-alpha/beta
- Clonal T-cell expansion in RCD2 is not manageable with steroids (see: RCD 1) and sometimes manageable with chemotherapeutic drugs,[110] however, more aggressive therapies seem more affective.[107] A high percentage of RCD 2 patients spontaneously develop lymphoma (EATL),[110] the 5 year survival rate is markedly lower than RCD1 but higher than lymphoma. DQ2.5/DQ2 individuals are more frequently found.[111]
Causes of RCD.
- Coeliac disease
- Age at CD/GSE diagnosis – most people are over the age of 50 when first diagnosed at RCD
- Dietary noncompliance – Some EATL appears years after diagnosis with non-GF diets.
- Length of latency – The length of time, often unknown in which the person is GSE+.
- Severity – The severity of the microscopic destruction appears to be a factor, and genetics appears now to play a role.[112]
- Genetics – For RCD 2 and EATL, genetics plays large role DQ2.5/DQ2+ individuals are over-represented in the patient set[110][111]
Cancers
GSE, particularly coeliac disease, increases the risk of cancers of specific types.[113] There are two predominant cancers associated with coeliac disease, cancer of the esophagus and lymphoproliferative diseases such as gluten-sensitive enteropathy-associated T-cell lymphoma (EATL).[114] For non-EATL cancers it is thought the mineralemias such as zinc and selenium may play a role in increasing risk.[19] GSE associated cancers are invariably associated with advanced coeliac disease, however, in de-novo EATL, the cancer is frequently detected in advance of the coeliac diagnosis, also EATL is the most common neoplasm.[7]
Esophageal cancer
Squamous carcinoma of the esophagus is more prevalent in coeliac disease.[114][115] The increased prevalence may be secondary to GERD that results from chronic delayed gastric emptying. Other studies implicate the malabsorption of vitamin A and zinc as a result of multi-vitamin and mineral deficiencies seen in Coeliac disease.[7][8]
References
- Cooper BT, Holmes GK, Cooke WT (1978). "Coeliac disease and immunological disorders". British Medical Journal. 1 (6112): 537–539. doi:10.1136/bmj.1.6112.537. PMC 1603223. PMID 630212.
- Vilppula A, Collin P, Mäki M, et al. (May 2008). "Undetected coeliac disease in the elderly A biopsy-proven population-based study". Dig Liver Dis. 40 (10): 809–813. doi:10.1016/j.dld.2008.03.013. PMID 18467196.
- Hunt KA, Zhernakova A, Turner G, Heap GA, Franke L, Bruinenberg M, et al. (April 2008). "Newly identified genetic risk variants for celiac disease related to the immune response". Nat. Genet. 40 (4): 395–402. doi:10.1038/ng.102. PMC 2673512. PMID 18311140.
- Rakover Y, Hager H, Nussinson E, Luboshitzky R (1994). "Celiac disease as a cause of transient hypocalcemia and hypovitaminosis D in a 13 year-old girl". The Journal of Pediatric Endocrinology. 7 (1): 53–5. doi:10.1515/JPEM.1994.7.1.53. PMID 8186825. S2CID 33701186.
- Hallert C, Grant C, Grehn S, et al. (2002). "Evidence of poor vitamin status in coeliac patients on a gluten-free diet for 10 years". Aliment. Pharmacol. Ther. 16 (7): 1333–1339. doi:10.1046/j.1365-2036.2002.01283.x. PMID 12144584. S2CID 20758464.
- Johnson EJ, Krasinski SD, Howard LJ, Alger SA, Dutta SK, Russell RM (1992). "Evaluation of vitamin A absorption by using oil-soluble and water-miscible vitamin A preparations in normal adults and in patients with gastrointestinal disease". Am. J. Clin. Nutr. 55 (4): 857–64. doi:10.1093/ajcn/55.4.857. PMID 1550069.
- Wright DH (1995). "The major complications of coeliac disease". Baillière's Clinical Gastroenterology. 9 (2): 351–369. doi:10.1016/0950-3528(95)90035-7. PMID 7549031.
- Mellow MH, Layne EA, Lipman TO, Kaushik M, Hostetler C, Smith JC (1983). "Plasma zinc and vitamin A in human squamous carcinoma of the esophagus". Cancer. 51 (9): 1615–1620. doi:10.1002/1097-0142(19830501)51:9<1615::AID-CNCR2820510911>3.0.CO;2-O. PMID 6831364.
- Reinken L, Zieglauer H (1978). "Vitamin B-6 absorption in children with acute celiac disease and in control subjects". J. Nutr. 108 (10): 1562–5. doi:10.1093/jn/108.10.1562. PMID 702197.
- Hallert C, Aström J, Walan A (1983). "Reversal of psychopathology in adult coeliac disease with the aid of pyridoxine (vitamin B6)". Scand. J. Gastroenterol. 18 (2): 299–304. doi:10.3109/00365528309181597. PMID 6369511.
- Shaker JL, Brickner RC, Findling JW, et al. (1997). "Hypocalcemia and skeletal disease as presenting features of celiac disease". Arch. Intern. Med. 157 (9): 1013–1016. doi:10.1001/archinte.157.9.1013. PMID 9140273.
- Mitterstieler G, Zieglauer H (1978). "[Vitamin K deficiency bleeding as a leading symptom in celiac disease (author's transl)]". Pädiatrie und Pädologie (in German). 13 (2): 175–82. PMID 643295.
- Mauro A, Orsi L, Mortara P, Costa P, Schiffer D (1991). "Cerebellar syndrome in adult celiac disease with vitamin E deficiency". Acta Neurol. Scand. 84 (2): 167–170. doi:10.1111/j.1600-0404.1991.tb04927.x. PMID 1950453. S2CID 19090624.
- Kleopa KA, Kyriacou K, Zamba-Papanicolaou E, Kyriakides T (2005). "Reversible inflammatory and vacuolar myopathy with vitamin E deficiency in celiac disease". Muscle Nerve. 31 (2): 260–265. doi:10.1002/mus.20144. PMID 15389648. S2CID 34027981.
- Rude RK, Olerich M (1996). "Magnesium deficiency: possible role in osteoporosis associated with gluten-sensitive enteropathy". Osteoporosis International. 6 (6): 453–461. doi:10.1007/BF01629578. PMID 9116391. S2CID 10964149.
- Van Dyk D, Inbal A, Kraus L, Grifel B, Ravid M (1981). "The watery diarrhea syndrome with hypercalcemia--a symptomatic response to phosphate buffer". Hepatogastroenterology. 28 (1): 58–9. PMID 7216140.
- Solomons NW, Rosenberg IH, Sandstead HH (1976). "Zinc nutrition in celiac sprue". Am. J. Clin. Nutr. 29 (4): 371–5. doi:10.1093/ajcn/29.4.371. PMID 1266787.
- Yüce A, Demir H, Temizel IN, Koçak N (2004). "Serum carnitine and selenium levels in children with celiac disease". Indian Journal of Gastroenterology. 23 (3): 87–8. PMID 15250563.
- Hinks LJ, Inwards KD, Lloyd B, Clayton BE (1984). "Body content of selenium in coeliac disease". British Medical Journal (Clinical Research Ed.). 288 (6434): 1862–1863. doi:10.1136/bmj.288.6434.1862. PMC 1441793. PMID 6428578.
- Kucharzewski M, Braziewicz J, Majewska U, Góźdź S (2002). "Concentration of selenium in the whole blood and the thyroid tissue of patients with various thyroid diseases". Biological Trace Element Research. 88 (1): 25–30. doi:10.1385/BTER:88:1:25. PMID 12117262. S2CID 1448985.
- Várkonyi A, Boda M, Endreffy E, Németh I, Timár E (1998). "Coeliac disease: always something to discover". Scand. J. Gastroenterol. Suppl. 33 (228): 122–129. doi:10.1080/003655298750026651. PMID 9867122.
- Wilcox GM, Mattia AR (2006). "Celiac sprue, hyperhomocysteinemia, and MTHFR gene variants". J. Clin. Gastroenterol. 40 (7): 596–601. doi:10.1097/00004836-200608000-00007. PMID 16917400. S2CID 27387815.
- Forshaw J, Harwood L (1971). "Diagnostic value of the serum folate assay". J. Clin. Pathol. 24 (3): 244–249. doi:10.1136/jcp.24.3.244. PMC 476963. PMID 5573438.
- Hauser GJ, Heiman I, Laurian L, Diamant S, Spirer Z (1981). "Selective IgA deficiency with multiple autoimmune disorders". Journal of Clinical & Laboratory Immunology. 6 (1): 81–5. PMID 7196455.
- Dickey W (2002). "Low serum vitamin B12 is common in coeliac disease and is not due to autoimmune gastritis". European Journal of Gastroenterology & Hepatology. 14 (4): 425–427. doi:10.1097/00042737-200204000-00016. PMID 11943958. S2CID 24979028.
- Depla AC, Bartelsman JF, Mulder CJ, Tytgat GN (1990). "Anemia: monosymptomatic celiac disease. A report of 3 cases". Hepatogastroenterology. 37 (1): 90–1. PMID 2312047.
- Corazza GR, Valentini RA, Andreani ML, et al. (1995). "Subclinical coeliac disease is a frequent cause of iron-deficiency anaemia". Scand. J. Gastroenterol. 30 (2): 153–156. doi:10.3109/00365529509093254. PMID 7732338.
- Ståhlberg MR, Savilahti E, Siimes MA (1991). "Iron deficiency in coeliac disease is mild and it is detected and corrected by gluten-free diet". Acta Paediatrica Scandinavica. 80 (2): 190–193. doi:10.1111/j.1651-2227.1991.tb11832.x. PMID 2035309. S2CID 19745356.
- Dickey W, McConnell B (1999). "Celiac disease presenting as the Paterson-Brown Kelly (Plummer-Vinson) syndrome". Am. J. Gastroenterol. 94 (2): 527–529. doi:10.1111/j.1572-0241.1999.889_r.x. PMID 10022662. S2CID 35004650.
- Kingham JG, Ramanaden D, Dawson A (1998). "Metachronous small-bowel adenocarcinoma in coeliac disease: gluten-free diet is not protective". Scand. J. Gastroenterol. 33 (2): 218–222. doi:10.1080/00365529850166987. PMID 9517536.
- Talbot RW, Heppell J, Dozois RR, Beart RW (1986). "Vascular complications of inflammatory bowel disease". Mayo Clin. Proc. 61 (2): 140–5. doi:10.1016/S0025-6196(12)65200-8. PMID 3080643.
- Srirajaskanthan R, Winter M, Muller AF (2005). "Venous thrombosis in inflammatory bowel disease". European Journal of Gastroenterology & Hepatology. 17 (7): 697–700. doi:10.1097/00042737-200507000-00001. PMID 15947544. S2CID 31333056.
- Liebman HA, Kashani N, Sutherland D, McGehee W, Kam AL (1998). "The factor V Leiden mutation increases the risk of venous thrombosis in patients with inflammatory bowel disease". Gastroenterology. 115 (4): 830–834. doi:10.1016/S0016-5085(98)70253-7. PMID 9753484.
- Casella G, Perego D, Baldini V, Monti C, Crippa S, Buda CA (2002). "A rare association between ulcerative colitis (UC), celiac disease (CD), membranous glomerulonephritis, leg venous thrombosis, and heterozygosity for factor V Leiden". J. Gastroenterol. 37 (9): 761–762. doi:10.1007/s005350200126. PMID 12375154. S2CID 6734431.
- Mari T, Zullo A, Hassan C, Di Giulio L, Morini S (2006). "Genetic association between factor V Leiden and coeliac disease". Gut. 55 (11): 1677–1678. doi:10.1136/gut.2006.104786. PMC 1860115. PMID 17047127.
- Lane AT, Huff JC, Weston WL (1982). "Detection of gluten in human sera by an enzyme immunoassay: comparison of dermatitis herpetiformis and celiac disease patients with normal controls". J. Invest. Dermatol. 79 (3): 186–189. doi:10.1111/1523-1747.ep12500053. PMID 7050253.
- Haussmann J, Sekar A (2006). "Chronic urticaria: a cutaneous manifestation of celiac disease". Can. J. Gastroenterol. 20 (4): 291–3. doi:10.1155/2006/871987. PMC 2659909. PMID 16609761.
- Hodgson HJ, Davies RJ, Gent AE (1976). "Atopic disorders and adult coeliac disease". Lancet. 1 (7951): 115–117. doi:10.1016/S0140-6736(76)93155-X. PMID 54635. S2CID 24439525.
- Abenavoli L, Leggio L, Gasbarrini G, Addolorato G (2007). "Celiac disease and skin: Psoriasis association". World J. Gastroenterol. 13 (14): 2138–9. doi:10.3748/wjg.v13.i14.2138. PMC 4319141. PMID 17465464.
- Abenavoli L, Proietti I, Leggio L, Ferrulli A, Vonghia L, Capizzi R, Rotoli M, Amerio PL, Gasbarrini G, Addolorato G (2006). "Cutaneous manifestations in celiac disease". World J. Gastroenterol. 12 (6): 843–52. doi:10.3748/wjg.v12.i6.843. PMC 4066147. PMID 16521210.
- McKenzie AW, Stubbing DG, Elvy BL (1976). "Prurigo nodularis and gluten enteropathy". Br. J. Dermatol. 95 (1): 89–92. PMID 952746.
- Francesco Stefanini G, Resta F, Marsigli L, et al. (1999). "Prurigo nodularis (Hyde's prurigo) disclosing celiac disease". Hepatogastroenterology. 46 (28): 2281–4. PMID 10521982.
- Popadić S, Nikolić M, Gajić-Veljić M, Bonaci-Nikolić B (2006). "Rothmund-Thomson syndrome. The first case with plantar keratoderma and the second with coeliac disease". Acta Dermatovenerologica Alpina, Pannonica et Adriatica. 15 (2): 90–3. PMID 16998609.
- Corazza GR, Andreani ML, Venturo N, Bernardi M, Tosti A, Gasbarrini G (1995). "Celiac disease and alopecia areata: report of a new association". Gastroenterology. 109 (4): 1333–1337. doi:10.1016/0016-5085(95)90597-9. PMID 7557104.
- Bardella MT, Marino R, Barbareschi M, Bianchi F, Faglia G, Bianchi P (2000). "Alopecia areata and coeliac disease: no effect of a gluten-free diet on hair growth". Dermatology. 200 (2): 108–10. doi:10.1159/000018340. PMID 10773696. S2CID 44430157.
- Bondavalli P, Quadri G, Parodi A, Rebora A (1998). "Failure of gluten-free diet in celiac disease-associated alopecia areata". Acta Derm. Venereol. 78 (4): 319. doi:10.1080/000155598442098. PMID 9689318.
- Wortsman J, Kumar V (1994). "Case report: idiopathic hypoparathyroidism co-existing with coeliac disease: immunologic studies". Am. J. Med. Sci. 307 (6): 420–427. doi:10.1097/00000441-199406000-00008. PMID 8198149.
- Lampasona V, Bonfanti R, Bazzigaluppi E, Venerando A, Chiumello G, Bosi E, Bonifacio E (1999). "Antibodies to tissue transglutaminase C in type I diabetes". Diabetologia. 42 (10): 1195–1198. doi:10.1007/s001250051291. PMID 10525659.
- Ludvigsson J, Ludvigsson J, Ekbom A, Montgomery S (2006). "Celiac disease and risk of subsequent type 1 diabetes: a general population cohort study of children and adolescents". Diabetes Care. 29 (11): 2483–2488. doi:10.2337/dc06-0794. PMID 17065689.
- Hansen D, Brock-Jacobsen B, Lund E, Bjørn C, Hansen L, Nielsen C, Fenger C, Lillevang S, Husby S (2006). "Clinical benefit of a gluten-free diet in type 1 diabetic children with screening-detected celiac disease: a population-based screening study with 2 years' follow-up". Diabetes Care. 29 (11): 2452–2456. doi:10.2337/dc06-0990. PMID 17065683.
- Bao F, Yu L, Babu S, Wang T, Hoffenberg EJ, Rewers M, Eisenbarth GS (1999). "One third of HLA DQ2 homozygous patients with type 1 diabetes express celiac disease-associated transglutaminase autoantibodies". J. Autoimmun. 13 (1): 143–148. doi:10.1006/jaut.1999.0303. PMID 10441179.
- MacFarlane AJ, Burghardt KM, Kelly J, et al. (2003). "A type 1 diabetes-related protein from wheat (Triticum aestivum). cDNA clone of a wheat storage globulin, Glb1, linked to islet damage". J. Biol. Chem. 278 (1): 54–63. doi:10.1074/jbc.M210636200. PMID 12409286.
- Van Der Werf, Nienke (2007). "Viral infections as potential triggers of type 1 diabetes". Diabetes Metab Res Rev. 23 (3): 169–183. doi:10.1002/dmrr.695. PMID 17103489. S2CID 31145812.
- Mäkelä M, Oling V, Marttila J, Waris M, Knip M, Simell O, Ilonen J (2006). "Rotavirus-specific T cell responses and cytokine mRNA expression in children with diabetes-associated autoantibodies and type 1 diabetes". Clin Exp Immunol. 145 (2): 261–270. doi:10.1111/j.1365-2249.2006.03146.x. PMC 1809689. PMID 16879245.
- Mäkelä M, Vaarala O, Hermann R, Salminen K, Vahlberg T, Veijola R, Hyöty H, Knip M, Simell O, Ilonen J (2006). "Enteral virus infections in early childhood and an enhanced type 1 diabetes-associated antibody response to dietary insulin". J Autoimmun. 27 (1): 54–61. doi:10.1016/j.jaut.2006.04.003. PMID 16757149.
- Collin P, Reunala T, Pukkala E, Laippala P, Keyriläinen O, Pasternack A (1994). "Coeliac disease--associated disorders and survival". Gut. 35 (9): 1215–1218. doi:10.1136/gut.35.9.1215. PMC 1375696. PMID 7959226.
- Elfström P, Montgomery SM, Kämpe O, Ekbom A, Ludvigsson JF (2007). "Risk of primary adrenal insufficiency in patients with celiac disease". Journal of Clinical Endocrinology & Metabolism. 92 (9): 3595–3598. doi:10.1210/jc.2007-0960. PMID 17595243.
- Ogborn AD (1975). "Pregnancy in patients with coeliac disease". British Journal of Obstetrics and Gynaecology. 82 (4): 293–6. doi:10.1111/j.1471-0528.1975.tb00637.x. PMID 1125150. S2CID 37897288.
- Collin P, Vilska S, Heinonen PK, Hällström O, Pikkarainen P (1996). "Infertility and coeliac disease". Gut. 39 (3): 382–384. doi:10.1136/gut.39.3.382. PMC 1383343. PMID 8949641.
- Jameson S (1976). "Zinc deficiency in malabsorption states: a cause of infertility?". Acta Med. Scand. Suppl. 593: 38–49. doi:10.1111/j.0954-6820.1976.tb12825.x. PMID 1067747.
- Pradhan M, Manisha, Singh R, Dhingra S (2007). "Celiac disease as a rare cause of primary amenorrhea: a case report". The Journal of Reproductive Medicine. 52 (5): 453–5. PMID 17583254.
- Ratnaike RN, Wangel AG (1977). "Immunological abnormalities in coeliac disease and their response to dietary restriction. I. Serum immunoglobulins, antibodies and complement". Australian and New Zealand Journal of Medicine. 7 (4): 349–52. doi:10.1111/j.1445-5994.1977.tb04393.x. PMID 270982.
- Wahnschaffe U, Schulzke JD, Zeitz M, Ullrich R (2007). "Predictors of Clinical Response to Gluten-Free Diet in Patients Diagnosed With Diarrhea-Predominant Irritable Bowel Syndrome". Clinical Gastroenterology and Hepatology. 5 (7): 844–850. doi:10.1016/j.cgh.2007.03.021. PMID 17553753.
- Leeds JS, Höroldt BS, Sidhu R, et al. (2007). "Is there an association between coeliac disease and inflammatory bowel diseases? A study of relative prevalence in comparison with population controls". Scand. J. Gastroenterol. 42 (10): 1214–20. doi:10.1080/00365520701365112. PMID 17918008. S2CID 25575750.
- Robb-Nicholson C (2007). "By the way, doctor. I heard that taking a proton-pump inhibitor could cause hip fractures. I've been taking 20 mg of Prilosec every day for a year. Should I be concerned?". Harvard Women's Health Watch. 14 (7): 8. PMID 17396273.
- Quaglietta L, Coccorullo P, Miele E, Pascarella F, Troncone R, Staiano A (2007). "Eosinophilic oesophagitis and coeliac disease: is there an association?". Alimentary Pharmacology & Therapeutics. 26 (3): 487–493. doi:10.1111/j.1365-2036.2007.03388.x. PMID 17635383. S2CID 25628864.
- Logan RF, Ferguson A, Finlayson ND, Weir DG (1978). "Primary biliary cirrhosis and coeliac disease: an association?". Lancet. 1 (8058): 230–233. doi:10.1016/S0140-6736(78)90480-4. PMID 74661. S2CID 54278759.
- Volta U, Rodrigo L, Granito A, et al. (2002). "Celiac disease in autoimmune cholestatic liver disorders". Am. J. Gastroenterol. 97 (10): 2609–13. doi:10.1111/j.1572-0241.2002.06031.x. PMID 12385447. S2CID 17375127.
- Patel RS, Johlin FC, Murray JA (1999). "Celiac disease and recurrent pancreatitis". Gastrointest. Endosc. 50 (6): 823–827. doi:10.1016/S0016-5107(99)70166-5. PMID 10570344.
- Nanda R, Anand BS (1993). "Celiac disease and tropical calcific pancreatitis". Am. J. Gastroenterol. 88 (10): 1790–2. PMID 8213729.
- Lahat E, Broide E, Leshem M, Evans S, Scapa E (2000). "Prevalence of celiac antibodies in children with neurologic disorders". Pediatr. Neurol. 22 (5): 393–396. doi:10.1016/S0887-8994(00)00129-6. PMID 10913732.
- Bushara KO (2005). "Neurologic presentation of celiac disease". Gastroenterology. 128 (4 Suppl 1): S92–S97. doi:10.1053/j.gastro.2005.02.018. PMID 15825133.
- Addolorato G, Di Giuda D, De Rossi G, et al. (2004). "Regional cerebral hypoperfusion in patients with celiac disease". Am. J. Med. 116 (5): 312–317. doi:10.1016/j.amjmed.2003.09.037. PMID 14984816.
- Ludvigsson JF, Olsson T, Ekbom A, Montgomery SM (2007). "A population-based study of coeliac disease, neurodegenerative and neuroinflammatory diseases". Aliment. Pharmacol. Ther. 25 (11): 1317–1327. doi:10.1111/j.1365-2036.2007.03329.x. PMID 17509100. S2CID 20170972.
- Freeman HJ, Gillett HR, Gillett PM, Oger J (October 2009). "Adult celiac disease with acetylcholine receptor antibody positive myasthenia gravis". World J. Gastroenterol. 15 (38): 4741–4. doi:10.3748/wjg.15.4741. PMC 2761549. PMID 19824105.
- Volta U, De Giorgio R, Granito A, et al. (2006). "Anti-ganglioside antibodies in coeliac disease with neurological disorders". Dig Liver Dis. 38 (3): 183–7. doi:10.1016/j.dld.2005.11.013. PMID 16458087.
- Hadjivassiliou M, Grünewald RA, Chattopadhyay AK, et al. (1998). "Clinical, radiological, neurophysiological, and neuropathological characteristics of gluten ataxia". Lancet. 352 (9140): 1582–5. doi:10.1016/S0140-6736(98)05342-2. PMID 9843103. S2CID 21937254.
- Hadjivassiliou M, Boscolo S, Davies-Jones GA, et al. (2002). "The humoral response in the pathogenesis of gluten ataxia". Neurology. 58 (8): 1221–6. doi:10.1212/wnl.58.8.1221. PMID 11971090.
- Chapman RW, Laidlow JM, Colin-Jones D, Eade OE, Smith CL (1978). "Increased prevalence of epilepsy in coeliac disease". British Medical Journal. 2 (6132): 250–251. doi:10.1136/bmj.2.6132.250. PMC 1606375. PMID 678891.
- Molteni N, Bardella MT, Baldassarri AR, Bianchi PA (1988). "Celiac disease associated with epilepsy and intracranial calcifications: report of two patients". Am. J. Gastroenterol. 83 (9): 992–4. PMID 3414652.
- Gobbi G, Ambrosetto P, Zaniboni MG, Lambertini A, Ambrosioni G, Tassinari CA (1992). "Celiac disease, posterior cerebral calcifications and epilepsy". Brain Dev. 14 (1): 23–9. doi:10.1016/S0387-7604(12)80275-0. PMID 1590524. S2CID 4782109.
- Hu WT, Murray JA, Greenaway MC, Parisi JE, Josephs KA (2006). "Cognitive impairment and celiac disease". Arch. Neurol. 63 (10): 1440–1446. doi:10.1001/archneur.63.10.1440. PMID 17030661.
- Pfaender M, D'Souza WJ, Trost N, Litewka L, Paine M, Cook M (2004). "Visual disturbances representing occipital lobe epilepsy in patients with cerebral calcifications and coeliac disease: a case series". J. Neurol. Neurosurg. Psychiatry. 75 (11): 1623–1625. doi:10.1136/jnnp.2003.031229. PMC 1738780. PMID 15489401.
- D'Amico D, Rigamonti A, Spina L, Bianchi-Marzoli S, Vecchi M, Bussone G (2005). "Migraine, celiac disease, and cerebral calcifications: a new case". Headache. 45 (9): 1263–1267. doi:10.1111/j.1526-4610.2005.00253_2.x. PMID 16178961. S2CID 38602698.
- Kieslich M, Errázuriz G, Posselt HG, Moeller-Hartmann W, Zanella F, Boehles H (2001). "Brain white-matter lesions in celiac disease: a prospective study of 75 diet-treated patients". Pediatrics. 108 (2): e21. doi:10.1542/peds.108.2.e21. PMID 11483831.
- Ciacci C, Iavarone A, Siniscalchi M, Romano R, De Rosa A (2002). "Psychological dimensions of celiac disease: toward an integrated approach". Dig. Dis. Sci. 47 (9): 2082–2087. doi:10.1023/A:1019637315763. PMID 12353859. S2CID 10308376.
- Addolorato G, Capristo E, Ghittoni G, et al. (2001). "Anxiety but not depression decreases in coeliac patients after one-year gluten-free diet: a longitudinal study". Scand. J. Gastroenterol. 36 (5): 502–506. doi:10.1080/00365520119754. PMID 11346203. S2CID 210160.
- Zipser RD, Patel S, Yahya KZ, Baisch DW, Monarch E (2003). "Presentations of adult celiac disease in a nationwide patient support group". Dig. Dis. Sci. 48 (4): 761–764. doi:10.1023/A:1022897028030. PMID 12741468. S2CID 37702479.
- Wallace DJ, Hallegua DS (2004). "Fibromyalgia: the gastrointestinal link". Current Pain and Headache Reports. 8 (5): 364–368. doi:10.1007/s11916-996-0009-z. PMID 15361320. S2CID 34122137.
- Siniscalchi M, Iovino P, Tortora R, et al. (2005). "Fatigue in adult coeliac disease". Aliment. Pharmacol. Ther. 22 (5): 489–494. doi:10.1111/j.1365-2036.2005.02619.x. PMID 16128688. S2CID 43543388.
- Arnason JA, Gudjónsson H, Freysdóttir J, Jónsdóttir I, Valdimarsson H (1992). "Do adults with high gliadin antibody concentrations have subclinical gluten intolerance?". Gut. 33 (2): 194–197. doi:10.1136/gut.33.2.194. PMC 1373929. PMID 1541415.
- Pinals RS (1986). "Arthritis associated with gluten-sensitive enteropathy". J. Rheumatol. 13 (1): 201–4. PMID 3701733.
- Williamson N, Asquith P, Stokes L, Jowett W, Cooke WT (1976). "Anticonnective tissue and other antitissue 'antibodies' in the sera of patients with coeliac disease compared with the findings in a mixed hospital population". J. Clin. Pathol. 29 (6): 484–494. doi:10.1136/jcp.29.6.484. PMC 476105. PMID 939804.
- Sökjer M, Jónsson T, Bödvarsson S, Jónsdóttir I, Valdimarsson H (1995). "Selective increase of IgA rheumatoid factor in patients with gluten sensitivity". Acta Derm. Venereol. 75 (2): 130–2. doi:10.2340/0001555575130132 (inactive 31 July 2022). PMID 7604641.
{{cite journal}}: CS1 maint: DOI inactive as of July 2022 (link) - Dieterich W, Esslinger B, Trapp D, Hahn E, Huff T, Seilmeier W, Wieser H, Schuppan D (2006). "Cross linking to tissue transglutaminase and collagen favours gliadin toxicity in coeliac disease". Gut. 55 (4): 478–484. doi:10.1136/gut.2005.069385. PMC 1856150. PMID 16188922.
- Molberg O, Sollid LM (2006). "A gut feeling for joint inflammation - using coeliac disease to understand rheumatoid arthritis". Trends Immunol. 27 (4): 188–194. doi:10.1016/j.it.2006.02.006. PMID 16530013.
- Volta U, De Angelis GL, Granito A, et al. (2006). "Autoimmune enteropathy and rheumatoid arthritis: a new association in the field of autoimmunity". Digestive and Liver Disease. 38 (12): 926–929. doi:10.1016/j.dld.2006.02.003. PMID 16920048.
- Kumar S, Gupta N, Jhamb R, Mishra D (2007). "Celiac disease: Association with adult-onset Still's disease: Apropos of a clinical case". Indian Journal of Medical Sciences. 61 (7): 414–7. doi:10.4103/0019-5359.33191. PMID 17611347.
- Marie I, Lecomte F, Hachulla E, et al. (2001). "An uncommon association: celiac disease and dermatomyositis in adults". Clin. Exp. Rheumatol. 19 (2): 201–3. PMID 11326486.
- Song MS, Farber D, Bitton A, Jass J, Singer M, Karpati G (2006). "Dermatomyositis associated with celiac disease: response to a gluten-free diet". Can. J. Gastroenterol. 20 (6): 433–5. doi:10.1155/2006/574074. PMC 2659927. PMID 16779462.
- Katz A, Dyck RF, Bear RA (1979). "Celiac disease associated with immune complex glomerulonephritis". Clin. Nephrol. 11 (1): 39–44. PMID 428155.
- Almroth G, Axelsson T, Müssener E, Grodzinsky E, Midhagen G, Olcén P (2006). "Increased Prevalence of Anti-Gliadin IgA-Antibodies with Aberrant Duodenal Histopathological Findings in Patients with IgA-Nephropathy and Related Disorders". Ups. J. Med. Sci. 111 (3): 339–352. doi:10.3109/2000-1967-060. PMID 17578801. S2CID 25201041.
- McDonald GB, Earnest DL, Admirand WH (1977). "Hyperoxaluria correlates with fat malabsorption in patients with sprue". Gut. 18 (7): 561–566. doi:10.1136/gut.18.7.561. PMC 1411579. PMID 873337.
- Stauffer JQ (1977). "Hyperoxaluria and intestinal disease. The role of steatorrhea and dietary calcium in regulating intestinal oxalate absorption". The American Journal of Digestive Diseases. 22 (10): 921–8. doi:10.1007/BF01076170. PMID 920694. S2CID 5804667.
- Daum S, Cellier C, Mulder CJ (2005). "Refractory coeliac disease". Best Practice & Research. Clinical Gastroenterology. 19 (3): 413–424. doi:10.1016/j.bpg.2005.02.001. PMID 15925846.
- Goerres MS, Meijer JW, Wahab PJ, et al. (2003). "Azathioprine and prednisone combination therapy in refractory coeliac disease". Aliment. Pharmacol. Ther. 18 (5): 487–494. doi:10.1046/j.1365-2036.2003.01687.x. PMID 12950421. S2CID 137361.
- Al-Toma A, Verbeek WH, Mulder CJ (2007). "Update on the management of refractory coeliac disease". Journal of Gastrointestinal and Liver Diseases. 16 (1): 57–63. PMID 17410290.
- Olaussen RW, Løvik A, Tollefsen S, et al. (2005). "Effect of elemental diet on mucosal immunopathology and clinical symptoms in type 1 refractory celiac disease". Clin. Gastroenterol. Hepatol. 3 (9): 875–885. doi:10.1016/S1542-3565(05)00295-8. PMID 16234025.
- Krauss N, Schuppan D (2006). "Monitoring nonresponsive patients who have celiac disease". Gastrointest. Endosc. Clin. N. Am. 16 (2): 317–327. doi:10.1016/j.giec.2006.03.005. PMID 16644460.
- Al-Toma A, Goerres MS, Meijer JW, et al. (2006). "Cladribine therapy in refractory celiac disease with aberrant T cells". Clin. Gastroenterol. Hepatol. 4 (11): 1322–1327. doi:10.1016/j.cgh.2006.07.007. PMID 16979946.
- Al-Toma A, Goerres MS, Meijer JW, Peña AS, Crusius JB, Mulder CJ (2006). "Human leukocyte antigen-DQ2 homozygosity and the development of refractory celiac disease and enteropathy-associated T-cell lymphoma". Clin. Gastroenterol. Hepatol. 4 (3): 315–319. doi:10.1016/j.cgh.2005.12.011. PMID 16527694.
- Jores RD, Frau F, Cucca F, et al. (2007). "HLA-DQB1*0201 homozygosis predisposes to severe intestinal damage in celiac disease". Scand. J. Gastroenterol. 42 (1): 48–53. doi:10.1080/00365520600789859. PMID 17190762. S2CID 7675714.
- Holmes GK, Stokes PL, Sorahan TM, Prior P, Waterhouse JA, Cooke WT (1976). "Coeliac disease, gluten-free diet, and malignancy". Gut. 17 (8): 612–619. doi:10.1136/gut.17.8.612. PMC 1411326. PMID 789184.
- Ferguson A, Kingstone K (1996). "Coeliac disease and malignancies". Acta Paediatrica Supplement. 412: 78–81. doi:10.1111/j.1651-2227.1996.tb14259.x. PMID 8783767. S2CID 156686.
- Selby WS, Gallagher ND (1979). "Malignancy in a 19-year experience of adult celiac disease". Dig. Dis. Sci. 24 (9): 684–688. doi:10.1007/BF01314465. PMID 487922. S2CID 3200328.
- Petreshock EP, Pessah M, Menachemi E (1975). "Adenocarcinoma of the jejunum associated with nontropical sprue". The American Journal of Digestive Diseases. 20 (8): 796–802. doi:10.1007/BF01070840. PMID 1155420. S2CID 1201520.