Pernicious anemia
Pernicious anemia is a type of vitamin B12 deficiency anemia, a disease in which not enough red blood cells are produced due to the malabsorption of vitamin B12.[7] Malabsorption in pernicious anemia results from the lack or loss of intrinsic factor needed for the absorption of vitamin B12.[4][8] Anemia is defined as a condition in which the blood has a lower than normal amount of red blood cells or hemoglobin.[9] The disease may come on slowly and insidiously.[10]
| Pernicious anemia | |
|---|---|
| Other names | Vitamin B12 deficiency anemia, Biermer's anemia,[1] Addison's anemia,[2] Addison–Biermer anemia[3] |
 | |
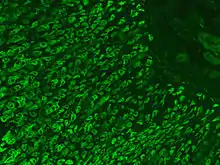
| Micrograph showing nodular enterochromaffin-like cell hyperplasia, as demonstrated with chromogranin A immunostaining, in the body of the stomach. Parietal cells are not readily apparent. These changes are in keeping with autoimmune metaplastic atrophic gastritis, a histologic correlate of vitamin B12 deficiency anemia. | |
| Specialty | Hematology |
| Symptoms | Feeling tired, weak, shortness of breath, lightheadedness, pale skin, abnormal sensations, depression, confusion, changes in reflexes[4] |
| Usual onset | > 60 years old[1] |
| Causes | Malabsorption of vitamin B12 resulting from lack of intrinsic factor[4] |
| Diagnostic method | Blood tests, bone marrow tests[5] |
| Treatment | Vitamin B12 pills or injections[4] |
| Prognosis | With treatment a normal life[4] |
| Frequency | 1 per 1000 people[6] |
The most common initial symptoms are tiredness, and weakness. Other signs and symptoms of anemia include breathlessness, dizziness, a sore red tongue, lightheadedness, headaches, poor ability to exercise, cold hands and feet, low blood pressure, pale or yellow skin, chest pain, and an irregular heartbeat.[9][11] The digestive tract may also be disturbed giving symptoms that can include nausea and vomiting, heartburn, upset stomach and loss of appetite.[4][10] Pernicious anemia can cause osteoporosis and may lead to bone fractures.[12] Symptoms of severe vitamin B12 deficiency can include tingling or numbness in the hands and feet, memory problems, blurred vision, unsteady walking, poor balance, muscle weakness, impaired sense of taste and smell, poor reflexes, clumsiness, depression, and confusion.[4] Without treatment, some of these problems may become permanent.[13]
Pernicious anemia occurs due to an autoimmune response that produces antibodies that attack the parietal cells in the stomach lining and prevents them from creating intrinsic factor.[4] Malabsorption may also result from the surgical removal of all or part of the stomach or small intestine; from an inherited disorder or from certain drugs or illnesses that damage the stomach lining.[14] Other causes of low vitamin B12 include not enough dietary intake (which can be a risk in a vegan diet), celiac disease, or tapeworm infection.[14] When suspected, diagnosis is made by blood tests initially a complete blood count, and occasionally, bone marrow tests.[4] Blood tests may show fewer but larger red blood cells, low numbers of young red blood cells, low levels of vitamin B12, and antibodies to intrinsic factor.[5]
Pernicious anemia can be treated with intramuscular injections or pills of vitamin B12.[4] Nasal sprays and gels are also available for those who have trouble swallowing pills. Treatment may need to be lifelong.[4]
Pernicious anemia due to autoimmune problems occurs in about one per 1000 people in the USA. Among those over the age of 60, about 2% have the condition.[6] It more commonly affects people of northern European descent.[2] Women are more commonly affected than men.[15] With proper treatment, most people live normal lives.[6] Due to a higher risk of stomach cancer, those with pernicious anemia should be checked regularly for this.[4] The first clear description was by Thomas Addison in 1849.[16][17] The term "pernicious" means "deadly", and this term came into use because before the availability of treatment the disease was often fatal.[13][18]
Signs and symptoms
Pernicious anemia often presents slowly, and can cause harm insidiously and unnoticeably. Untreated, it can lead to neurological complications, and in serious cases, death.[19] It can take several years for pernicious anemia to appear, and the disease often goes unrecognized, as the body becomes used to feeling unwell.[20] The onset may be vague and slow, as the same symptoms are often also present with anemia; in 81.1% of cases of cobalamin deficiency, pernicious anemia is not observed.[21] Pernicious anemia may be present without a person experiencing symptoms at first, over time, feeling tired and weak, lightheadedness, dizziness, headaches, rapid or irregular heartbeat, breathlessness, glossitis (a sore red tongue), poor ability to exercise, low blood pressure, cold hands and feet, pale or yellow skin, easy bruising and bleeding, low-grade fevers, shakiness, cold sensitivity, chest pain, upset stomach, nausea, loss of appetite, heartburn, weight loss, diarrhea, constipation, severe joint pain, feeling abnormal sensations including tingling or numbness to the fingers and toes (pins and needles), and tinnitus, may occur.[22][23][24][25][26] Anemia may present with a number of further common symptoms,[22][27] including hair thinning and loss, early greying of the hair, mouth ulcers, bleeding gums,[23] angular cheilitis, a look of exhaustion with pale and dehydrated or cracked lips and dark circles around the eyes, as well as brittle nails.[24]
In more severe or prolonged cases of pernicious anemia, nerve cell damage may occur,[20] which can lead to more severe symptoms, including sense loss, difficulty in proprioception, neuropathic pain, unsteady walking (ataxia), poor balance, loss of sensation in the feet, muscle weakness, blurred vision (either due to retinopathy[28] or optic neuropathy[29]), impaired urination, fertility problems, decreased sense of taste and smell, decreased level of consciousness, changes in reflexes, memory loss, mood swings, depression, irritability, slurred speech, cognitive impairment, confusion, anxiety, clumsiness, psychosis, and, in more severe cases, dementia.[22][23][24][25][26][30][31] Anemia may also lead to cardiac murmurs[25][24] and/or altered blood pressure (low or high). The deficiency may also present with thyroid disorders.[22] In severe cases, the anemia may cause congestive heart failure.[27] A complication of severe chronic PA is subacute combined degeneration of spinal cord, which leads to distal sensory loss (posterior column), absent ankle reflex, increased knee reflex response, and extensor plantar response.[32] Other than anemia, hematological symptoms may include cytopenias, intramedullary hemolysis, and pseudothrombotic microangiopathy.[1] Vitamin B12 deficiency, which is reversible, is occasionally confused with acute myeloid leukemia, which is an irreversible autoimmune condition presenting with some of the same hematological symptoms, including hypercellular bone marrow with blastic differentiation and hypersegmented neutrophils.[33] Pernicious anemia can contribute to a delay in physical growth in children, and may also be a cause for delay in puberty for adolescents.[4]
Causes
Vitamin B12 cannot be produced by the human body, and must be obtained from the diet. When foods containing B12 are eaten, the vitamin is usually bound to protein and is released by proteases released by the pancreas into the small bowel. Following its release, most B12 is absorbed by the body in the small bowel (ileum) after binding to a protein known as intrinsic factor. Intrinsic factor is produced by parietal cells of the gastric mucosa (stomach lining) and the intrinsic factor-B12-complex is absorbed by enterocytes in the ileum's cubam receptors.[34][35] PA is characterised by B12 deficiency caused by the absence of intrinsic factor.[36] Other disorders that can disrupt the absorption of vitamin B12 in the small intestine include celiac disease, surgical removal of crohn's disease, and HIV.[37]

PA may be considered as an end stage of autoimmune atrophic gastritis, a disease characterised by stomach atrophy and the presence of antibodies to parietal cells and intrinsic factor.[38][39] Autoimmune atrophic gastritis, is localised to the body of the stomach, where parietal cells are located.[36] Antibodies to intrinsic factor and parietal cells cause the destruction of the oxyntic gastric mucosa, in which the parietal cells are located, leading to the subsequent loss of intrinsic factor synthesis. Without intrinsic factor, the ileum can no longer absorb the B12.[40] Atrophic gastritis is often a precursor to gastric cancer.[39]
Although the exact role of Helicobacter pylori infection in PA remains controversial, evidence indicates H. pylori is involved in the pathogenesis of the disease. A long-standing H. pylori infection may cause gastric autoimmunity by a mechanism known as molecular mimicry. Antibodies produced by the immune system can be cross-reactive and may bind to both H. pylori antigens and those found in the gastric mucosa. The antibodies are produced by activated B cells that recognise both pathogen and self-derived peptides. The autoantigens believed to cause the autoreactivity are the alpha and beta subunits of the sodium-potassium pump.[40][41] In a study, B12 deficiency caused by Helicobacter pylori was positively correlated with CagA positivity and gastric inflammatory activity, rather than gastric atrophy.[42] Less commonly, H. pylori and Zollinger-Ellison syndrome may cause a form of nonautoimmune gastritis that can lead to pernicious anemia.[43]
Impaired B12 absorption can also occur following gastric removal (gastrectomy) or gastric bypass surgery. In these surgeries, either the parts of the stomach that produce gastric secretions are removed or they are bypassed. This means intrinsic factor, as well as other factors required for B12 absorption, are not available. However, B12 deficiency after gastric surgery does not usually become a clinical issue. This is probably because the body stores many years' worth of B12 in the liver and gastric surgery patients are adequately supplemented with the vitamin.[44][45]
Although no specific PA susceptibility genes have been identified, a genetic factor likely is involved in the disease. Pernicious anemia is often found in conjunction with other autoimmune disorders, suggesting common autoimmune susceptibility genes may be a causative factor.[36] In spite of that, previous family studies and case reports focusing on PA have suggested that there is a tendency of genetic heritance of PA in particular, and close relatives of the PA patients seem to have higher incidence of PA and associated PA conditions.[46][47][48] Moreover, it was further indicated that the formation of antibodies to gastric cells was autosomal dominant gene determined, and the presence of antibodies to the gastric cells might not be necessarily related to the occurrence of atrophic gastritis related to PA.[46][48]
Pathophysiology
Although the healthy body stores three to five years' worth of B12 in the liver, the usually undetected autoimmune activity in one's gut over a prolonged period of time leads to B12 depletion and the resulting anemia; pernicious anemia refers to one of the hematologic manifestations of chronic auto-immune gastritis, in which the immune system targets the parietal cells of the stomach or intrinsic factor itself, leading to decreased absorption of vitamin B12.
B12 is required by enzymes for two reactions: the conversion of methylmalonyl-CoA to succinyl-CoA, and the conversion of homocysteine to methionine. In the latter reaction, the methyl group of levomefolic acid is transferred to homocysteine to produce tetrahydrofolate and methionine. This reaction is catalyzed by the enzyme methionine synthase with B12 as an essential cofactor. During B12 deficiency, this reaction cannot proceed, which leads to the accumulation of levomefolic acid. This accumulation depletes the other types of folate required for purine and thymidylate synthesis, which are required for the synthesis of DNA. Inhibition of DNA replication in maturing red blood cells results in the formation of large, fragile megaloblastic erythrocytes. The neurological aspects of the disease are thought to arise from the accumulation of methylmalonyl- CoA due to the requirement of B12 as a cofactor to the enzyme methylmalonyl-CoA mutase.[49][50][51][52]
Diagnosis
Pernicious anemia is thought mainly to be an autoimmune disorder that attacks the gastric parietal cells that produce intrinsic factor resulting in impaired absorption of B12. However, pernicious anemia may also have a genetic component, potentially running in families.[20] Pernicious anemia may be suspected when a blood smear shows large, brittle, immature, erythrocytes, known as megaloblasts. To make a diagnosis a full blood count, and blood smear, with the following tests included is needed:[5][49]
- A complete blood count and blood smear evaluates the mean corpuscular volume (MCV) and the mean corpuscular hemoglobin concentration (MCHC) to demonstrate megaloblastic anemia.[20] PA is identified with a high MCV (macrocytic anemia) and a normal MCHC (normochromic anemia).[53] Ovalocytes are also typically seen on the blood smear, and a pathognomonic feature of megaloblastic anemias (which include PA and others) is hypersegmented neutrophils.[24]
- Vitamin B12 serum levels are used to detect its deficiency,[20] but do not distinguish its causes. Vitamin B12 levels can be falsely high or low and data for sensitivity and specificity vary widely. Normal serum levels may be found in cases of deficiency where myeloproliferative disorders, liver disease, transcobalamin II deficiency, or small intestinal bacterial overgrowth are present.[54][55]
- Intrinsic factor and parietal cell antibodies – the blood is checked for antibodies against IF and parietal cells in the stomach. The presence of antibodies to gastric parietal cells and IF is common in PA. Parietal cell antibodies are found in other autoimmune disorders and also in up to 10% of healthy individuals. However, around 85% of PA patients have parietal cell antibodies, which means they are a sensitive marker for the disease. Intrinsic factor antibodies are much less sensitive than parietal cell antibodies, but they are much more specific. They are found in about half of PA patients and are very rarely found in other disorders. These antibody tests can distinguish between PA and food-B12 malabsorption.[55][56]
- Methylmalonic acid and/or homocysteine – vitamin B12 plays an important role in metabolic processes and cellular functions. Therefore, its deficiency leads to the accumulation of some metabolic products. Methylmalonic acid and/or homocysteine is one of the metabolic products that can be measured in the blood. as the increase in the levels of both helps differentiate between vitamin B12 deficiency and folic acid deficiency, because homocysteine alone increases in the latter.[55][56]
Elevated gastrin levels can be found in around 80–90% of PA cases, but they may also be found in other forms of gastritis. Decreased pepsinogen I levels or a decreased pepsinogen I to pepsinogen II ratio may also be found, although these findings are less specific to PA and can be found in food-B12 malabsorption and other forms of gastritis.[56]
The diagnosis of atrophic gastritis type A should be confirmed by gastroscopy and stepwise biopsy.[57] About 90% of individuals with PA have antibodies for parietal cells; however, only 50% of all individuals in the general population with these antibodies have pernicious anemia.[58]
Forms of vitamin B12 deficiency other than PA must be considered in the differential diagnosis of megaloblastic anemia. For example, a B12-deficient state which causes megaloblastic anemia and which may be mistaken for classical PA may be caused by infection with the tapeworm Diphyllobothrium latum, possibly due to the parasite's competition with host for vitamin B12.[59]
The classic test for PA, the Schilling test, is no longer widely used, as more efficient methods are available. This historic test consisted, in its first step, of taking an oral dose of radiolabelled vitamin B12, followed by quantitation of the vitamin in the patient's urine over a 24-hour period via measurement of the radioactivity. A second step of the test repeats the regimen and procedure of the first step, with the addition of oral intrinsic factor. A patient with PA presents lower than normal amounts of intrinsic factor; hence, addition of intrinsic factor in the second step results in an increase in vitamin B12 absorption (over the baseline established in the first). The Schilling test distinguished PA from other forms of B12 deficiency,[49] specifically, from Imerslund–Gräsbeck syndrome, a B12-deficiency caused by mutations in CUBN that codes for cubilin the cobalamin receptor.[60]
Treatment

Pernicious anemia may not be diagnosed at first.[1] More in-depth diagnosis may be required.[1] Pernicious anemia caused by a loss of intrinsic factor cannot be prevented.[13] If there are other, reversible causes of low vitamin B12 levels, the cause must be treated.[14] Pernicious anemia is usually easily treated by providing the necessary level of vitamin B12 supplementation.[4] Severe cases can be treated with intramuscular injections of vitamin B12.[4] Less severe cases may be treated with high doses of oral supplemenation of vitamin B12.[4] A nasal spray, gel, and sublingual preparation are also available for people who may have difficulty in swallowing. Folate supplementation may affect the course and treatment of pernicious anemia, therefore vitamin B12 replacement is often recommended initially.[61] In some severe cases of anemia, a blood transfusion may be needed to resolves haematological effects.[13] Often treatment will be needed for life.[13][62]
Prognosis
A person with well-treated PA can live a healthy life. Failure to diagnose and treat in time, however, may result in permanent neurological damage, excessive fatigue, depression, memory loss, and other complications. In severe cases, the neurological complications of pernicious anemia can lead to death – hence the name, "pernicious", meaning deadly.
There is an increased risk of gastric cancer in those with pernicious anemia linked to the common feature of atrophic gastritis.[63][64]
Epidemiology
PA is estimated to affect 0.1% of the general population and 1.9% of those over 60, accounting for 20–50% of B12 deficiency in adults.[1] A review of literature shows that the prevalence of PA is higher in Northern Europe, especially in Scandinavian countries, and among people of African descent, and that increased awareness of the disease and better diagnostic tools might play a role in apparently higher rates of incidence.[65]
History
A case of anemia with a first recognition of associated atrophic gastritis a feature of pernicious anemia, was first described in 1824 by James Combe. This was fully investigated in 1849, by British physician Thomas Addison, from which it acquired the common name of Addison's anemia. In 1871, the first accurate description of the disease in Europe was by Michael Anton Biermer, a German physician who referred to the insidious course of the condition, and because it was untreatable and fatal at the time, he first referred to it as "pernicious" anemia.[66][67] In 1900 Russell coined the term subacute combined degeneration of spinal cord.[68]
In 1907, Richard Clarke Cabot reported on a series of 1200 patients with PA; their average survival was between one and three years.[69] Pernicious anemia was a fatal disease before about the year 1920, until the importance of the liver in hematopoiesis was recognized, the treatment of pernicious anemia was unsuccessful and arbitrary. It may have motivated George Whipple, who had a keen interest in liver diseases, to investigate the liver's role in hematopoiesis. Whipple began evaluating the effects of treatments for anemia caused by chronic blood loss. Whipple, Huber, and Robchett have studied the effects on hemoglobin and blood regeneration of a variety of treatments – among which only raw liver has shown real promise.[67] Serendipity is said to have played a role in this discovery. Whipple observed that blood regeneration was poor in dogs fed cooked liver after chronic blood loss, had it not been that a lazy laboratory technician had given the dogs raw liver, the much more dramatic response might not have been discovered at that point in history.[67]

Around 1926, George Minot and William P. Murphy, who learned of Whipple's discovery, sought raw liver as a treatment for pernicious anemia. They later suggested a high-protein diet with high amounts of raw liver. This caused a rapid improvement in symptoms and a simultaneous rise in red blood cell counts.[70] Fruit and iron were also part of the diet, and it appears that at this point, Minot and Murphy were not quite sure that the liver was a very important factor. It was thought that iron in liver tissue, not liver juice-soluble factor, cured hemorrhagic anemia in dogs. Thus, the discovery of liver juice as a treatment for pernicious anemia had been by coincidence. However, Minot, Murphy, and Whipple received the joint Nobel Prize for discovering a cure for a previously fatal disease of unknown cause in 1934, becoming the first Americans to be awarded the Nobel Prize in Physiology and Medicine.[67][71]
It is not easy to eat uncooked liver, and extracts were developed as a concentrate of liver juice for intramuscular injection. In 1928, chemist Edwin Cohn prepared an extract that was 50 to 100 times stronger than obtained from raw liver. This became part of the standard management of pernicious anemia until the 1950s. The active ingredient in the liver remained unknown until 1948.[68] The anti-pernicious anemia factor was only isolated from the liver by Smith, Rex and others. The substance was cobalamin, which the discoverers called "vitamin B12".[67] They showed that giving a few micrograms could prevent relapse in the disease. Dorothy Hodgkin and co-workers went on to use X-ray crystallography to elucidate the structure of cobalamin for which she, too, was awarded a Nobel Prize.[72]
Understanding of the pathogenesis of pernicious anaemia increased over subsequent decades. It had long been known that the disease was associated with defects in the gastrointestinal tract: patients had chronic gastritis and lack of acid secretion (achlorhydria). It is known that transport of physiological amounts of vitamin B12 depends on the combined actions of gastric, ileal and pancreatic components. The gastric moiety was discovered and named 'intrinsic factor' by William Castle in 1930. A further important advance was made in the early 1960s by Doniach with the recognition that pernicious anemia is an autoimmune disease.[67] Pernicious anemia is eventually treated with either injections or large oral doses of B12, typically between 1 and 4 mg daily.
A medical author takes the view that Mary Todd Lincoln, the wife of American President Abraham Lincoln, had pernicious anemia for decades and died from it in 1882.[73][74]
Research
Permeation enhancers
Treatment using oral drugs is an easier option in management but the bioavailabity of B12 is low. This is due to low absorption in the intestine, and breakdown by enzyme activity. Research continues to focus on the use of permeation enhancers or permeation absorbers in combination with the treatment. One of the better performing enhancers studied is salcoprozate sodium (SNAC).[75][76] SNAC is able to form a noncovalent complex with cobalamin while preserving its chemical integrity and protect B12 from gastric acidity.[77] This complex is much more lipophilic than the water-soluble vitamin B12, so is able to pass through cellular membranes with greater ease. Molecular dynamics are used in experiments to gain an understanding of the molecular interactions involved in the different molecules used and the degree of ease achieved in absorption across the gastric epithelium.[75]
References
- Andres E, Serraj K (2012). "Optimal management of pernicious anemia". Journal of Blood Medicine. 3: 97–103. doi:10.2147/JBM.S25620. PMC 3441227. PMID 23028239.
- Professional guide to diseases (9 ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. 2009. p. 502. ISBN 978-0-7817-7899-2.
- Forbis, Pat (2005). Stedman's medical eponyms (2nd ed.). Baltimore, Md.: Lippincott Williams & Wilkins. p. 6. ISBN 978-0-7817-5443-9.
- "Pernicious Anemia | NHLBI, NIH". www.nhlbi.nih.gov. Retrieved 25 February 2022.
- "How Is Pernicious Anemia Diagnosed?". NHLBI. April 1, 2011. Archived from the original on 14 March 2016. Retrieved 14 March 2016.
- Li X, Thomsen H, Sundquist K, Sundquist J, Försti A, Hemminki K (2021). "Familial Risks between Pernicious Anemia and Other Autoimmune Diseases in the Population of Sweden". Autoimmune Diseases. 2021: 8815297. doi:10.1155/2021/8815297. PMC 7815416. PMID 33505716.
- "ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Retrieved 19 February 2022.
- Qudsiya, Zainab; De Jesus, Orlando (2022). "Subacute Combined Degeneration of the Spinal Cord". StatPearls. StatPearls Publishing. PMID 32644742.
- "Anemia". www.nhlbi.nih.gov. Retrieved 25 February 2022.
- "Pernicious Anemia Clinical Presentation: History, Physical Examination". emedicine.medscape.com. Retrieved 27 April 2022.
- Zhang, Qin; Lv, Xue-ying; Yang, Yun-mei (2015). "Megaloblastic anemia with hypotension and transient delirium as the primary symptoms: report of a case". International Journal of Clinical and Experimental Medicine. 8 (10): 18879–18883. PMC 4694411. PMID 26770511. S2CID 5744323.
- Melton, ME; Kochman, ML (April 1994). "Reversal of severe osteoporosis with vitamin B12 and etidronate therapy in a patient with pernicious anemia". Metabolism: Clinical and Experimental. 43 (4): 468–9. doi:10.1016/0026-0495(94)90078-7. hdl:2027.42/31684. PMID 8159105.
- "What Is Pernicious Anemia?". NHLBI. April 1, 2011. Archived from the original on 14 March 2016. Retrieved 14 March 2016.
- "What Causes Pernicious Anemia?". NHLBI. April 1, 2011. Archived from the original on 14 March 2016. Retrieved 14 March 2016.
- Greer, John P. (2009). Wintrobe's clinical hematology (12th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 1157. ISBN 978-0-7817-6507-7. Archived from the original on 2016-03-14.
- Wailoo, Keith (1999). "The Corporate "Conquest" of Pernicious Anemia". Drawing blood technology and disease identity in twentieth-century America (Johns Hopkins Paperbacks ed.). Baltimore, Md.: Johns Hopkins University Press. p. Chapter 4. ISBN 978-0-8018-7029-3. Archived from the original on 2016-03-14.
- Dictionary of Medicine. Routledge. 2014. p. 404. ISBN 978-1-135-92841-4. Archived from the original on 2016-03-14.
- Tamparo, Carol (2016). Diseases of the Human Body. F.A. Davis. p. 295. ISBN 978-0-8036-5791-5. Archived from the original on 2016-03-17.
- "Pernicious Anemia Symptoms, Types, Causes & Treatment". MedicineNet. Retrieved 2021-12-11.
- "Pernicious Anemia". Healthline. 2020-05-13. Retrieved 2021-10-12.
- Htut, Thura Win; Thein, Kyaw Zin; Oo, Thein Hlaing (2021). "Pernicious anemia: Pathophysiology and diagnostic difficulties". Journal of Evidence-Based Medicine. 14 (2): 161–69. doi:10.1111/jebm.12435. ISSN 1756-5391. PMID 34015185. S2CID 235074954.
- Ramani, James Carton, Richard Daly, Pramila (2007). Clinical pathology. Oxford: Oxford University Press. ISBN 978-0-19-856946-6.
- "Vitamin B12 Deficiency: Causes, Symptoms, and Treatment". WebMD. Retrieved 2021-09-21.
- Means, Robert T. Jr. & Glader, Bertil (2009). "Anemia: General Considerations (Chapter 26)". In Greer, J.P.; Foerster, J.; Rodgers, G.M.; Paraskevas, F.; Glader, B.; Arber, D.A.; Means Jr., R.T. (eds.). Wintrobe's Clinical Hematology. Vol. 1 (12th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. pp. 779–809, esp. 782. ISBN 978-0-7817-6507-7. Retrieved 10 March 2016.
{{cite book}}: CS1 maint: uses authors parameter (link) - Schick, P.; Conrad, Marcel E.; Besa, Emmanuel C., eds. (2015-08-15). "Pernicious Anemia, Clinical Presentation". Medscape. Archived from the original on 17 November 2012. Retrieved 21 January 2013.
- "Harmful and Sneaky – Vitamin B12 deficiency | Unjury Protein". unjury.com. Retrieved 2021-09-21.
- Turgeon, Mary L. (2005). Clinical hematology : theory and procedures (4th ed.). Philadelphia: Lippincott Williams & Wilkins. ISBN 978-0-7817-5007-3.
- Li, Kenneth; McKay, Gerald (23 March 2000). "Ischemic Retinopathy Caused by Severe Megaloblastic Anemia". New England Journal of Medicine. 342 (12): 860. doi:10.1056/NEJM200003233421205. ISSN 0028-4793. PMID 10727590.
- Ata, Fateen; Bint I Bilal, Ammara; Javed, Saad; Shabir Chaudhry, Hammad; Sharma, Rohit; Fatima Malik, Rubab; Choudry, Hassan; Bhaskaran Kartha, Anand (December 2020). "Optic neuropathy as a presenting feature of vitamin B-12 deficiency: A systematic review of literature and a case report". Annals of Medicine and Surgery. 60: 316–322. doi:10.1016/j.amsu.2020.11.010. PMC 7653199. PMID 33204422.
- Hvas AM, Nexo E (November 2006). "Diagnosis and treatment of vitamin B12 deficiency – an update". Haematologica. 91 (11): 1506–12. PMID 17043022.
- "Vitamin B12 or folate deficiency anaemia – Complications". nhs.uk. 2017-10-20. Retrieved 2021-10-13.
- Gersten, Todd & VeriMed Healthcare Network (2016). "Pernicious anemia". In Zieve, David; Ogilvie, Isla; et al. (eds.). MedlinePlus Medical Encyclopedia. Washington, DC: nlm.nih.gov. Archived from the original on 11 March 2016. Retrieved 11 March 2016.
{{cite encyclopedia}}: CS1 maint: uses authors parameter (link) - Konda, Manojna; Godbole, Abhijit; Pandey, Soumya; Sasapu, Appalanaidu (2019-07-30). "Vitamin B12 deficiency mimicking acute leukemia". Proceedings (Baylor University. Medical Center). 32 (4): 589–92. doi:10.1080/08998280.2019.1641045. ISSN 0899-8280. PMC 6793970. PMID 31656431.
- Kalantari S, Brezzi B, Bracciamà V, Barreca A, Nozza P, Vaisitti T, Amoroso A, Deaglio S, Manganaro M, Porta F, Spada M (February 2022). "Adult-onset CblC deficiency: a challenging diagnosis involving different adult clinical specialists". Orphanet J Rare Dis. 17 (1): 33. doi:10.1186/s13023-022-02179-y. PMC 8812048. PMID 35109910.
- Christensen EI, Birn H (April 2002). "Megalin and cubilin: multifunctional endocytic receptors". Nat. Rev. Mol. Cell Biol. 3 (4): 256–66. doi:10.1038/nrm778. PMID 11994745. S2CID 21893726.
- Banka S, Ryan K, Thomson W, Newman WG (June 2011). "Pernicious anemia – genetic insights". Autoimmunity Reviews. 10 (8): 455–59. doi:10.1016/j.autrev.2011.01.009. PMID 21296191.
- "Pernicious Anemia | NHLBI, NIH". www.nhlbi.nih.gov. Retrieved 24 February 2022.
- Marzinotto I, Dottori L, Baldaro F, Dilaghi E, Brigatti C, Bazzigaluppi E, Esposito G, Davidson HW, Piemonti L, Lampasona V, Lahner E (2021). "Intrinsic factor autoantibodies by luminescent immuno-precipitation system in patients with corpus atrophic gastritis". J Transl Autoimmun. 4: 100131. doi:10.1016/j.jtauto.2021.100131. PMC 8716657. PMID 35005595.
- Shah SC, Piazuelo MB, Kuipers EJ, Li D (October 2021). "AGA Clinical Practice Update on the Diagnosis and Management of Atrophic Gastritis: Expert Review". Gastroenterology. 161 (4): 1325–1332.e7. doi:10.1053/j.gastro.2021.06.078. PMC 8740554. PMID 34454714.
- Lahner E, Annibale B (November 2009). "Pernicious anemia: New insights from a gastroenterological point of view". World J. Gastroenterol. 15 (41): 5121–8. doi:10.3748/wjg.15.5121. PMC 2773890. PMID 19891010.
- Desai HG, Gupte PA (December 2007). "Helicobacter pylori link to pernicious anaemia". The Journal of the Association of Physicians of India. 55: 857–59. PMID 18405134.
- Ulasoglu C, Temiz HE, Sağlam ZA. "The Relation of Cytotoxin-Associated Gene – A Seropositivity with Vitamin B12 Deficiency in Helicobacter pylori-Positive Patients". Biomed Res Int. 2019:1450536. Published 2019 Dec 9. doi:10.1155/2019/1450536
- Kaferle J, Strzoda CE (Feb 1, 2009). "Evaluation of macrocytosis". American Family Physician. 79 (3): 203–08. PMID 19202968.
- von Drygalski A, Andris DA (Apr–May 2009). "Anemia after bariatric surgery: more than just iron deficiency". Nutrition in Clinical Practice. 24 (2): 217–26. doi:10.1177/0884533609332174. PMID 19321896. S2CID 21448167.
- John S, Hoegerl C (November 2009). "Nutritional deficiencies after gastric bypass surgery". The Journal of the American Osteopathic Association. 109 (11): 601–04. doi:10.7556/jaoa. PMID 19948694. S2CID 245177279.
- Whittingham, S.; Ungar, B.; Mackay, I. R.; Mathews, J. D. (1969). "The Genetic Factor in Pernicious Anemia. A Family Study in Patients with Gastritis". The Lancet. 1 (7602): 951–54. doi:10.1016/S0140-6736(69)91856-X. PMID 4180811.
- McIntyre O. R., Sullivan L. W., Jeffries G. H., Silver R. H. (1965). "Pernicious Anemia in Childhood". The New England Journal of Medicine. 272 (19): 981–86. doi:10.1056/nejm196505132721901. PMID 14279251.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Wangel, A. G.; Callender, S. T.; Spray, G. H.; Wright, R. (1968). "A Family Study of Pernicious Anemia II. Intrinsic Factor Secretion, Vitamin B12 Absorption and Genetic Aspects of Gastric Autoimmunity". British Journal of Haematology. 14 (2): 183–204. doi:10.1111/j.1365-2141.1968.tb01486.x. PMID 5635601. S2CID 6994133.
- Wickramasinghe, SN (November 2006). "Diagnosis of megaloblastic anaemias". Blood Reviews. 20 (6): 299–318. doi:10.1016/j.blre.2006.02.002. PMID 16716475.
- Oh R, Brown DL (Mar 1, 2003). "Vitamin B12 deficiency". American Family Physician. 67 (5): 979–86. PMID 12643357.
- O'Leary F, Samman S (March 2010). "Vitamin B12 in health and disease". Nutrients. 2 (3): 299–316. doi:10.3390/nu2030299. PMC 3257642. PMID 22254022.
- Stover, PJ (June 2004). "Physiology of folate and vitamin B12 in health and disease". Nutrition Reviews. 62 (6 Pt 2): S3–12, discussion S13. doi:10.1111/j.1753-4887.2004.tb00070.x. PMID 15298442.
- Pagana, Timothy James; Pagana, Kathleen Deska (2006). Mosby's manual of diagnostic and laboratory tests. Mosby Elsevier. ISBN 978-0-323-03903-1.
- Devalia V (August 2006). "Diagnosing vitamin B-12 deficiency on the basis of serum B-12 assay". BMJ. 333 (7564): 385–86. doi:10.1136/bmj.333.7564.385. PMC 1550477. PMID 16916826.
- Snow, CF (Jun 28, 1999). "Laboratory diagnosis of vitamin B12 and folate deficiency: a guide for the primary care physician". Archives of Internal Medicine. 159 (12): 1289–98. doi:10.1001/archinte.159.12.1289. PMID 10386505.
- Moridani, Majid; Shana Ben-Poorat (March 2006). "Laboratory Investigation of Vitamin B12 Deficiency". Laboratory Medicine. 37 (3): 166–74. doi:10.1309/cvhkle2r4w68k2nq. S2CID 73781536.
- Miederer, S.E. (1977). The Histotopography of the Gastric Mucosa. Thieme, ISBN 3-13-508601-1
- Butler CC, Vidal-Alaball J, Cannings-John R, et al. (June 2006). "Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency: a systematic review of randomized controlled trials". Family Practice. 23 (3): 279–85. doi:10.1093/fampra/cml008. PMID 16585128.
- Ramakrishnan, Usha, ed. (2000). Nutritional anemias. Boca Raton: CRC Press. ISBN 978-0-8493-8569-8.
- Andres E., Serra K. (2012). "Optimal management of pernicious anemia". Journal of Blood Medicine. 3: 97–103. doi:10.2147/JBM.S25620. PMC 3441227. PMID 23028239.
- Cuskelly, Geraldine J.; Mooney, Kathleen M.; Young, Ian S. (November 2007). "Folate and vitamin B12: friendly or enemy nutrients for the elderly". The Proceedings of the Nutrition Society. 66 (4): 548–558. doi:10.1017/S0029665107005873. ISSN 0029-6651. PMID 17961276. S2CID 4639220.
- Bensky MJ, Ayalon-Dangur I, Ayalon-Dangur R, Naamany E, Gafter-Gvili A, Koren G, Shiber S (June 2019). "Comparison of sublingual vs. intramuscular administration of vitamin B12 for the treatment of patients with vitamin B12 deficiency". Drug Deliv Transl Res. 9 (3): 625–630. doi:10.1007/s13346-018-00613-y. PMID 30632091. S2CID 57765412.
- Lahner E, Capasso M, Carabotti M, Annibale B (August 2018). "Incidence of cancer (other than gastric cancer) in pernicious anaemia: A systematic review with meta-analysis". Dig Liver Dis. 50 (8): 780–786. doi:10.1016/j.dld.2018.05.012. PMID 29887343. S2CID 47006345.
- Venerito M, Link A, Rokkas T, Malfertheiner P (September 2016). "Gastric cancer - clinical and epidemiological aspects". Helicobacter. 21 Suppl 1: 39–44. doi:10.1111/hel.12339. PMID 27531538. S2CID 25093505.
- Stabler S. P., Allen R. H. (2004). "Vitamin B12 deficiency as a worldwide problem". Annual Review of Nutrition. 24 (1): 299–326. doi:10.1146/annurev.nutr.24.012003.132440. PMID 15189123.
- Enersen, Ole Daniel (2016). "Whonamedit Dictionary of Medical Eponyms". whonamedit.com. Archived from the original on 3 March 2016. Retrieved 11 March 2016.
- Sinclair, L. (2008-05-01). "Recognizing, treating and understanding pernicious anaemia". Journal of the Royal Society of Medicine. 101 (5): 262–264. doi:10.1258/jrsm.2008.081006. PMC 2376267. PMID 18463283.
- "Vitamin B-12 Associated Neurological Diseases: Background, Pathophysiology, Epidemiology". 22 February 2022. Retrieved 4 March 2022.
- Bunn, H. Franklin (2014-02-20). Longo, Dan L. (ed.). "Vitamin B12 and Pernicious Anemia — The Dawn of Molecular Medicine". New England Journal of Medicine. 370 (8): 773–776. doi:10.1056/NEJMcibr1315544. ISSN 0028-4793. PMID 24552327.
- "History of Vitamin B-12 and Pernicious Anemia". 2021-11-16. Archived from the original on 2021-11-16. Retrieved 2021-11-16.
- "The Nobel Prize in Physiology or Medicine 1934". NobelPrize.org. Retrieved 3 March 2022.
- "The Nobel Prize in Chemistry 1964". NobelPrize.org. Retrieved 2021-11-18.
- John G. Sotos, The Mary Lincoln Mind-Body Sourcebook: Including a Unifying Diagnosis to Explain Her Public Decay, Manifest Insanity, and Slow Death (Mt. Vernon, VA: Mt. Vernon Book Systems, 2016) ISBN 978-0-9818193-8-9
- Sotos, JG (2015). ""What an Affliction": Mary Todd Lincoln's Fatal Pernicious Anemia". Perspectives in Biology and Medicine. 58 (4): 419–43. doi:10.1353/pbm.2015.0034. PMID 27397049. S2CID 28038786.
- Kneiszl, R; Hossain, S; Larsson, P (3 January 2022). "In Silico-Based Experiments on Mechanistic Interactions between Several Intestinal Permeation Enhancers with a Lipid Bilayer Model". Molecular Pharmaceutics. 19 (1): 124–137. doi:10.1021/acs.molpharmaceut.1c00689. PMC 8728740. PMID 34913341.
- Castelli, M. C.; Wong, D. F.; Friedman, K.; Riley, M. G. I. (2011). "Pharmacokinetics of Oral Cyanocobalamin Formulated with Sodium N-\8-(2-hydroxybenzoyl)amino]caprylate (SNAC): An Open-Label, Randomized, Single-Dose, Parallel-Group Study in Healthy Male Subjects". Clinical Therapeutics. 33 (7): 934–945. doi:10.1016/j.clinthera.2011.05.088. PMID 21722960.
- Jonathan Courtney, PharmDc (2016-06-13). "Cyanocobalamin/Salcaprozate Sodium: A Novel Way to Treat Vitamin B12 Deficiency and Anemia".
{{cite journal}}: Cite journal requires|journal=(help)