Ivacaftor
Ivacaftor is a medication used to treat cystic fibrosis in people with certain mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene (primarily the G551D mutation), who account for 4–5% cases of cystic fibrosis.[5][6] It is also included in combination medications, lumacaftor/ivacaftor, tezacaftor/ivacaftor, and elexacaftor/tezacaftor/ivacaftor which are used to treat people with cystic fibrosis.[7][8][9]
 | |
| Clinical data | |
|---|---|
| Trade names | Kalydeco |
| Other names | VX-770 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a612012 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 99% |
| Metabolism | CYP3A |
| Elimination half-life | 12 hrs (single dose) |
| Excretion | 88% faeces |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.226.211 |
| Chemical and physical data | |
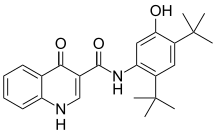
| Formula | C24H28N2O3 |
| Molar mass | 392.499 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| | |
Ivacaftor was developed by Vertex Pharmaceuticals in conjunction with the Cystic Fibrosis Foundation and is the first medication that treats the underlying cause rather than the symptoms of the disease.[10] It was approved by the U.S. Food and Drug Administration (FDA) in January 2012.[11][12][13] It is one of the most expensive drugs, costing over US$300,000 per year, which has led to criticism of the high cost. The combination drug lumacaftor/ivacaftor was approved by the FDA in July 2015.[14]
Cystic fibrosis is caused by any one of several defects in the CFTR protein, which regulates fluid flow within cells and affects the components of sweat, digestive fluids, and mucus. One such defect is the G551D mutation, in which the amino acid glycine (G) in position 551 is replaced with aspartic acid (D). G551D is characterized by a dysfunctional CFTR protein on the cell surface. In the case of G551D, the protein is trafficked to the correct area, the epithelial cell surface, but once there the protein cannot transport chloride through the channel. Ivacaftor, a CFTR potentiator, improves the transport of chloride through the ion channel by binding to the channels directly to induce a non-conventional mode of gating which in turn increases the probability that the channel is open.[15][16][17]
Medical uses
Ivacaftor is used for the treatment of cystic fibrosis in people having one of several specific mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) protein: E56K, G178R, S549R, K1060T, G1244E, P67L, E193K, G551D, A1067T, S1251N, R74W, L206W, G551S, G1069R, S1255P, D110E, R347H, D579G, R1070Q, D1270N, D110H, R352Q, S945L, R1070W, G1349D, R117C, A455E, S977F, F1074L, R117H, S549N, F1052V, D1152H.[18][3][19]
Ivacaftor is also included in a combination product, lumacaftor/ivacaftor, in a single pill, which is used to treat people with cystic fibrosis who have the F508del mutation in CFTR.[20][21][7][22]
Ivacaftor is also included in the combination product tezacaftor/ivacaftor with ivacaftor sold as Symdeko and as Symkevi.[8][23][24][25]
Symdeko is indicated to treat people aged six and older who have two copies of the F508del mutation in CFTR.[8][23][26]
Symkevi is indicated in a combination regimen with ivacaftor 150 mg tablets for the treatment of people with cystic fibrosis (CF) aged twelve years and older who are homozygous for the F508del mutation or who are heterozygous for the F508del mutation and have one of the following mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene: P67L, R117C, L206W, R352Q, A455E, D579G, 711+3A→G, S945L, S977F, R1070W, D1152H, 2789+5G→A, 3272 26A→G, and 3849+10kbC→T.[9]
Ivacaftor is available in a combination product with elexacaftor and tezacaftor called Trikafta for the treatment of people with cystic fibrosis who have the F508del mutation or other mutations.[27]
Adverse effects
The most common adverse reactions experienced by patients who received ivacaftor in the pooled placebo-controlled Phase III studies were abdominal pain (15.6% versus 12.5% on placebo), diarrhoea (12.8% versus 9.6% on placebo), dizziness (9.2% versus 1.0% on placebo), rash (12.8% versus 6.7% on placebo), upper respiratory tract reactions (including upper respiratory tract infection, nasal congestion, pharyngeal erythema, oropharyngeal pain, rhinitis, sinus congestion, and nasopharyngitis) (63.3% versus 50.0% on placebo), headache (23.9% versus 16.3% on placebo) and bacteria in sputum (7.3% versus 3.8% on placebo). One patient in the ivacaftor group reported a serious adverse reaction: abdominal pain.[28][4]
Pharmacology
Pharmacodynamics
Ivacaftor is a "potentiator" of CFTR, meaning it increases the probability that the defective channel will be open and allow chloride ions pass through the channel pore.[20]
Distribution
Ivacaftor is approximately 99% bound to plasma proteins, primarily to alpha 1-acid glycoprotein and albumin. Ivacaftor does not bind to human red blood cells.[28][4]
Biotransformation
Ivacaftor is extensively metabolised in humans. In vitro and in vivo data indicate that ivacaftor is primarily metabolised by CYP3A. M1 and M6 are the two major metabolites of ivacaftor in humans. M1 has approximately one-sixth the potency of ivacaftor and is considered pharmacologically active. M6 has less than one-fiftieth the potency of ivacaftor and is not considered pharmacologically active.[28][4]
Elimination
Following oral administration, the majority of ivacaftor (87.8%) is eliminated in the faeces after metabolic conversion. The major metabolites M1 and M6 accounted for approximately 65% of total dose eliminated with 22% as M1 and 43% as M6. There was negligible urinary excretion of ivacaftor as unchanged parent. The apparent terminal half-life was approximately 12 hours following a single dose in the fed state. The apparent clearance (CL/F) of ivacaftor was similar for healthy subjects and patients with CF. The mean (±SD) of CL/F for the 150 mg dose was 17.3 (8.4) L/h in healthy subjects at steady state.[28][4]
Society and culture
Legal status
The U.S. Food and Drug Administration (FDA) approved ivacaftor in January 2012,[29] and soon afterwards so too did the European Medicines Agency (EMA)[28][4] and Canada[30] and across some European countries.[31][32][33]
Lumacaftor/ivacaftor was approved by the FDA in July 2015, under breakthrough therapy status and under a priority review.[34]
Economics
The cost of ivacaftor is US$311,000 per year, roughly similar to the price of other medications for extremely rare diseases.[35] In the first nine months of its second year on the market (2014), ivacaftor sales were $339M, representing 54% of Vertex's product sales revenue. During the same period, total drug development expenses were $458M, most of which was spent on cystic fibrosis-related research.[36]
An editorial in JAMA called the price of ivacaftor "exorbitant", citing the support by the Cystic Fibrosis Foundation in its development and the contribution made by fundamental scientific research performed by the National Institutes of Health and relied upon by Vertex in its cystic fibrosis drug discovery programs.[37] The company responded in an email that "while publicly funded academic research provided important early understanding of the cause of cystic fibrosis, it took Vertex scientists 14 years of their own research, funded mostly by the company, before the drug won approval."[38]
The Cystic Fibrosis Foundation, a non-profit organization dedicated to improving healthcare for people with cystic fibrosis, provided $150 million of the funding for the development for ivacaftor in exchange for royalty rights in the event that the medication was successfully developed and commercialized. In 2014, the Foundation sold these royalty rights for $3.3 billion. The Foundation has stated that it intends to spend these funds in support of further research.[39][40]
Vertex said it would make the medication available free to patients in the United States with no insurance and a household income of under $150,000.[41] In 2012, 24 US doctors and researchers involved in the development of the medication wrote to Vertex to protest the price of the medication, which had been set at about $300,000 per year. In the UK, the company provided the medication free for a limited time for certain patients, then left the hospitals to decide whether to continue to pay for it for those patients. UK agencies estimated the cost per quality adjusted life year (QALY) at between £335,000 and £1,274,000 —well above the National Institute for Health and Care Excellence thresholds.[42]
The medication was not covered under the Ontario Drug Benefit plan until June 2014, when the Government of Ontario and the manufacturer negotiated for what "Ontario Health Minister Deb Matthews had called a "fair price" for taxpayers". The negotiations took 16 months and it was estimated that around 20 Ontarians required the medication at the time.[43]
The province of Alberta began covering the medication in July 2014, and in September the province of Saskatchewan became the third province to include it in its provincial medication plan.[44]
Delay in agreement on a price for Vertex to charge national health plans led to patient group protests in Wales,[45][46] England,[47] and Australia.[48]
As of March 2016, the combination medication cost $259,000 a year in the United States.[49]
Research
The clinical trials used in the regulatory approval of ivacaftor are described here.
G551D mutation
Of the approximately 70,000 cases of cystic fibrosis worldwide, 4% (~3,000) are due to a mutation called G551D.[50][51] The safety and efficacy of ivacaftor for the treatment of cystic fibrosis in patients with this mutation was examined in two clinical trials.
The first trial was performed in adults having baseline respiratory function (FEV1) between 32% and 98% of normal for persons of similar age, height, and weight. The baseline average was 64%. Improvement in FEV1 was rapid and sustained. At the end of 48 weeks, people treated with ivacaftor had on average an absolute increase in FEV1 of 10.4%, vs. a decline of 0.2% in the placebo group. Pulmonary exacerbations were reduced by about half in the ivacaftor group relative to the placebo group.[3]
In a second trial conducted in children age six to 11, the average improvement in FEV1 was an absolute increase of 12.5% in the ivacaftor group at 48 weeks, compared to a very slight decline in the placebo group.[3]
Other mutations
A third clinical trial examined the efficacy of ivacaftor in people with cystic fibrosis due to G1244E, G1349D, G178R, G551S, S1251N, S1255P, S549N, or S549R mutations. This trial, which included 39 people of age greater than six years, used a crossover design. The people in the trial had FEV1 averaging 78% of normal at baseline. The people in the trial were randomized to receive either ivacaftor or placebo for eight weeks. This was followed by a four to eight week washout period, then each group received the opposite treatment from what it received in the first part of the trial. At week 8, the people on treatment with ivacaftor experienced an average absolute improvement in FEV1 of 13.8%, but there was a strong dependence of the efficacy on the exact mutation that a patient had. The detailed data for different mutation types is shown in the U.S package insert.[3]
References
- "Ivacaftor (Kalydeco) Use During Pregnancy". Drugs.com. 9 November 2019. Retrieved 26 June 2020.
- "Kalydeco Product information". Health Canada. 25 April 2012. Retrieved 31 May 2022.
- "Kalydeco- ivacaftor tablet, film coated Kalydeco- ivacaftor granule prescribing information". DailyMed. 25 April 2019. Retrieved 20 November 2019.
- "Kalydeco EPAR". European Medicines Agency (EMA). Archived from the original on 21 November 2019. Retrieved 20 November 2019.
- Jones AM, Helm JM (October 2009). "Emerging treatments in cystic fibrosis". Drugs. 69 (14): 1903–10. doi:10.2165/11318500-000000000-00000. PMID 19747007. S2CID 23344660.
- McPhail GL, Clancy JP (April 2013). "Ivacaftor: the first therapy acting on the primary cause of cystic fibrosis". Drugs Today. 49 (4): 253–60. doi:10.1358/dot.2013.49.4.1940984. PMID 23616952.
- "Orkambi- lumacaftor and ivacaftor tablet, film coated Orkambi- lumacaftor and ivacaftor granule prescribing information". DailyMed. 15 July 2019. Retrieved 20 November 2019.
- "Symdeko- tezacaftor and ivacaftor kit prescribing information". DailyMed. 11 June 2019. Retrieved 20 November 2019.
- "Symkevi EPAR". European Medicines Agency (EMA). Retrieved 26 June 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Phase 3 Study of VX-770 Shows Marked Improvement in Lung Function Among People with Cystic Fibrosis with G551D Mutation" (Press release). Cystic Fibrosis Foundation. 23 February 2011 – via PR Newswire.
- "Drug Approval Package: Kalydeco (ivacaftor)". U.S. Food and Drug Administration (FDA). 13 March 2012. Archived from the original on 21 November 2019. Retrieved 20 November 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "The Most Important New Drug Of 2012". Forbes.
- Nocera J (18 July 2014). "The $300,000 Drug". The New York Times. Retrieved 20 November 2019.
- "Orkambi (lumacaftor/ivacaftor) Oral Tablet". U.S. Food and Drug Administration (FDA). 21 November 2019. Archived from the original on 21 November 2019. Retrieved 20 November 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Eckford PD, Li C, Ramjeesingh M, Bear CE (October 2012). "Cystic fibrosis transmembrane conductance regulator (CFTR) potentiator VX-770 (ivacaftor) opens the defective channel gate of mutant CFTR in a phosphorylation-dependent but ATP-independent manner". J. Biol. Chem. 287 (44): 36639–49. doi:10.1074/jbc.M112.393637. PMC 3481266. PMID 22942289.
- Van Goor F, Hadida S, Grootenhuis PD, Burton B, Cao D, Neuberger T, Turnbull A, Singh A, Joubran J, Hazlewood A, Zhou J, McCartney J, Arumugam V, Decker C, Yang J, Young C, Olson ER, Wine JJ, Frizzell RA, Ashlock M, Negulescu P (November 2009). "Rescue of CF airway epithelial cell function in vitro by a CFTR potentiator, VX-770". Proc. Natl. Acad. Sci. U.S.A. 106 (44): 18825–30. Bibcode:2009PNAS..10618825V. doi:10.1073/pnas.0904709106. PMC 2773991. PMID 19846789.
- Sloane PA, Rowe SM (November 2010). "Cystic fibrosis transmembrane conductance regulator protein repair as a therapeutic strategy in cystic fibrosis". Curr Opin Pulm Med. 16 (6): 591–7. doi:10.1097/MCP.0b013e32833f1d00. PMC 3733473. PMID 20829696.
- Cystic Fibrosis Foundation: FDA Approves Ivacaftor for 23 Additional CFTR Mutations
- "FDA expands approved use of Kalydeco to treat additional mutations of cystic fibrosis". U.S. Food and Drug Administration (FDA) (Press release). 17 May 2017. Archived from the original on 21 November 2019. Retrieved 20 November 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Kuk K, Taylor-Cousar JL (2015). "Lumacaftor and ivacaftor in the management of patients with cystic fibrosis: current evidence and future prospects". Ther Adv Respir Dis. 9 (6): 313–26. doi:10.1177/1753465815601934. PMID 26416827.
- "Orkambi (lumacaftor and ivacaftor)". CenterWatch. Retrieved 24 March 2016.
- "Drug Trials Snapshots: Orkambi". U.S. Food and Drug Administration (FDA). 30 July 2015. Archived from the original on 21 November 2019. Retrieved 20 November 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Drug Trials Snapshots: Symdeko". U.S. Food and Drug Administration (FDA). 7 March 2018. Archived from the original on 21 November 2019. Retrieved 20 November 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Symdeko (tezacaftor/ivacaftor) Tablets". U.S. Food and Drug Administration (FDA). 13 March 2018. Archived from the original on 11 December 2019. Retrieved 11 December 2019.
- "Summary Basis of Decision - Symdeko". Health Canada. 15 April 2019. Archived from the original on 21 November 2019. Retrieved 20 November 2019.
- "FDA expands approval of treatment for cystic fibrosis to include patients ages 6 and older". U.S. Food and Drug Administration (FDA) (Press release). 21 June 2019. Archived from the original on 11 December 2019. Retrieved 11 December 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Trikafta- elexacaftor, tezacaftor, and ivacaftor kit". DailyMed. 29 January 2020. Retrieved 22 August 2020.
- "Kalydeco: Annex I: Summary of product characteristics" (PDF). European Medicines Agency.
- "FDA approves Kalydeco to treat rare form of cystic fibrosis". U.S. Food and Drug Administration (FDA) (Press release). 31 January 2012. Archived from the original on 18 March 2016. Retrieved 20 November 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Summary Basis of Decision (SBD): Kalydeco - 2012 - Health Canada". Archived from the original on 6 August 2014. Retrieved 19 August 2014.
- "Kalydeco 50mg granules sachets - Summary of Product Characteristics (SmPC)". (emc). 30 August 2019. Archived from the original on 21 November 2019. Retrieved 20 November 2019.
- "Kalydeco 75mg granules sachets - Summary of Product Characteristics (SmPC)". (emc). 30 August 2019. Archived from the original on 21 November 2019. Retrieved 20 November 2019.
- "Kalydeco 150 mg film-coated tablets - Summary of Product Characteristics (SmPC)". (emc). 30 August 2019. Archived from the original on 21 November 2019. Retrieved 20 November 2019.
- "FDA approves new treatment for cystic fibrosis" (Press release). U.S. Food and Drug Administration (FDA). 2 July 2015. Archived from the original on 26 January 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "F.D.A. Approves New Cystic Fibrosis Drug". The New York Times. 31 January 2012. Retrieved 10 February 2015.
- "Vertex Pharmaceuticals 10-Q, Quarter ending September 30, 2014". Retrieved 10 February 2015.
- Brian P. O'Sullivan; David M. Orenstein; Carlos E. Milla (2 October 2013). "Viewpoint: Pricing for Orphan Drugs: Will the Market Bear What Society Cannot?". JAMA. 310 (13): 1343–1344. doi:10.1001/jama.2013.278129. PMID 24084916.
- "Cystic Fibrosis: Charity and Industry Partner for Profit". MedPage Today. 19 May 2013. Retrieved 10 February 2015.
- "CF Foundation Cashes Out on Kalydeco in $3.3B Sale to Royalty Pharma | Xconomy". 19 November 2014.
- "CF Foundation Royalty Sale Will Be Transformational for People with CF". Archived from the original on 27 December 2014.
- "FDA Approves Kalydeco (ivacaftor), the First Medicine to Treat the Underlying Cause of Cystic Fibrosis" (Press release). Cambridge, Massachusetts: Vertex Pharmaceuticals. 31 January 2012. Retrieved 1 February 2014.
- Deborah Cohen; James Raftery (12 February 2014). "Orphan Drugs: Paying twice: questions over high cost of cystic fibrosis drug developed with charitable funding". BMJ. 348: g1445. doi:10.1136/bmj.g1445. PMID 24523379. S2CID 8702814.
- Ferguson R (20 June 2014). "OHIP to cover cystic fibrosis drug Kalydeco". The Toronto Star. Retrieved 20 June 2014.
- "Saskatchewan to cover $300K cystic fibrosis drug Kalydeco". CBC News. 28 August 2014. Retrieved 28 August 2014.
- "Plea for Kalydeco drug to be introduced | Wales - ITV News".
- "Cystic fibrosis: New drug Kalydeco refused for Welsh NHS". BBC News Online. 8 May 2013.
- "Protests at Birmingham Hospital as cystic fibrosis sufferer is denied life-saving drug". Birmingham Mail. 29 October 2012.
- "Kalydeco breakthrough: Plea for life-saving medicine proves a winner". Manning River Times. 23 December 2013.
- Wasserman, Emily (23 March 2016). "NICE gives initial thumbs-down to Vertex's CF combo med Orkambi, citing costs". FiercePharma.
- "FAQs about the Cause, Diagnosis, Treatment of Cystic Fibrosis & More | CF Foundation". Archived from the original on 25 October 2006. Retrieved 27 December 2014.
- Bobadilla JL, Macek M, Fine JP, Farrell PM (June 2002). "Cystic fibrosis: a worldwide analysis of CFTR mutations--correlation with incidence data and application to screening". Hum. Mutat. 19 (6): 575–606. doi:10.1002/humu.10041. PMID 12007216. S2CID 35428054.
External links
- "Ivacaftor". Drug Information Portal. U.S. National Library of Medicine.
- "Ivacaftor mixture with lumacaftor". Drug Information Portal. U.S. National Library of Medicine.
- "Ivacaftor regimen with Tezacaftor". Drug Information Portal. U.S. National Library of Medicine.
- "Lumacaftor and Ivacaftor". MedlinePlus.
- "Tezacaftor and Ivacaftor". MedlinePlus.
- "Elexacaftor, Tezacaftor, and Ivacaftor". MedlinePlus.