Lumbar spinal stenosis
Lumbar spinal stenosis (LSS) is a medical condition in which the spinal canal narrows and compresses the nerves and blood vessels at the level of the lumbar vertebrae. Spinal stenosis may also affect the cervical or thoracic region, in which case it is known as cervical spinal stenosis or thoracic spinal stenosis. Lumbar spinal stenosis can cause pain in the low back or buttocks, abnormal sensations, and the absence of sensation (numbness) in the legs, thighs, feet, or buttocks, or loss of bladder and bowel control.
| Lumbar spinal stenosis | |
|---|---|
| Other names | wear and tear in the spine |
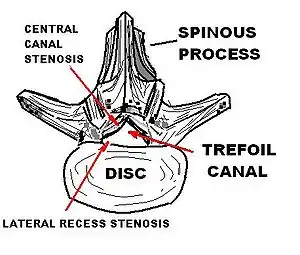 | |
| Lumbar vertebra showing central stenosis and lateral recess stenosis. | |
| Specialty | Orthopedics |
| Symptoms | Pain, numbness, or weakness in the low back, buttocks, or legs typically worsened with prolonged walking or standing and relieved with sitting or lying down |
| Usual onset | Gradual (months to years) |
| Types | Congenital, acquired |
| Causes | Narrowed spinal cord due to spinal degeneration or abnormal anatomy |
| Diagnostic method | Clinical (a combination of history, physical examination, and imaging) |
| Differential diagnosis | Claudication from peripheral artery disease |
| Treatment | Medication, physiotherapy, injections, surgery |
The precise cause of LSS is unclear. Narrowing of spinal structures in the spinal cord such as the central canal, the lateral recesses, or the intervertebral foramen (the opening where a spinal nerve root passes) must be present, but are not sufficient to cause LSS alone.[1] Many people who undergo MRI imaging are found to have such changes but have no symptoms.[1] These changes are commonly seen in people who have spinal degeneration that occurs with aging (e.g., spinal disc herniation). LSS may also be caused by osteophytes, osteoporosis, a tumor, trauma, or various skeletal dysplasias, such as with pseudoachondroplasia and achondroplasia.
Medical professionals may clinically diagnose lumbar spinal stenosis using a combination of a thorough medical history, physical examination, and imaging (CT or MRI).[1] EMG may be helpful if the diagnosis is unclear.[1] Useful clues that support a diagnosis of LSS are age; radiating leg pain that worsens with prolonged standing or walking (neurogenic claudication) and is relieved by sitting, lying down, or bending forward at the waist; and a wide stance when walking.[1] Other helpful clues may include objective weakness or decreased sensation in the legs, decreased reflexes in the legs, and balance difficulties, all of which are strongly associated with LSS.[1] Most people with LSS qualify for initial conservative non-operative treatment. Nonsurgical treatments include medications, physiotherapy, and injection procedures.[1] Decompressive spinal surgery may modestly improve outcomes but carries greater risk than conservative treatment.[1] Overall, there is limited supporting evidence to determine the most effective surgical or nonsurgical treatment for people with symptomatic LSS.[1] Evidence to support the use of acupuncture is also limited.[1]
Lumbar spinal stenosis is a common condition and causes substantial morbidity and disability. It is the most common reason people over the age of 65 pursue spinal surgery.[1] The condition affects over 200,000 people in the United States.[1]
Signs and symptoms
Understanding the meaning of signs and symptoms of lumbar stenosis requires an understanding of what the syndrome is, and the prevalence of the condition. A review of lumbar stenosis in the Journal of the American Medical Association's "Rational Clinical Examination Series"[2] emphasized that the syndrome can be considered when lower extremity pain occurs in combination with back pain. The syndrome occurs in 12% of older community-dwelling men[3] and up to 21% of those in retirement communities.[4]
Because the leg symptoms in lumbar spinal stenosis (LSS) are similar to those found with vascular claudication, the term pseudoclaudication is often used for symptoms of LSS.[5] These symptoms include pain, weakness, and tingling of the legs,[5] which may radiate down the legs to the feet.[6] Additional symptoms in the legs may be fatigue, heaviness, weakness, a sensation of tingling, pricking, or numbness, and leg cramps, as well as bladder symptoms.[6] Symptoms are most commonly bilateral and symmetrical, but they may be unilateral; leg pain is usually more troubling than back pain.[6]
Pseudoclaudication, now generally referred to as neurogenic claudication, typically worsens with standing or walking, and improves with sitting, and is often related to posture and lumbar extension. Lying on the side is often more comfortable than lying flat, since it permits greater lumbar flexion. Vascular claudication can resemble spinal stenosis, and some individuals experience unilateral or bilateral symptoms radiating down the legs rather than true claudication.[7]
The first symptoms of stenosis include bouts of low back pain. After a few months or years, this may progress to claudication. The pain may be radicular, following the classic neurologic pathways. This occurs as the spinal nerves or spinal cord become increasingly trapped in a smaller space within the canal. Determining whether pain in the elderly is caused by lack of blood supply or stenosis is difficult; testing can usually differentiate between them, but patients can have both vascular disease in the legs and spinal stenosis.
Among people with lower-extremity pain in combination with back pain, lumbar stenosis as the cause is two times more likely in those older than 70 years of age while in those younger than 60 years it is less than half as likely. The character of the pain is also useful for diagnosis. When the discomfort does not occur while seated, the likelihood of lumbar spinal stenosis increases considerably, around 7.4 times. Other features increasing the likelihood of lumbar stenosis are improvement in symptoms on bending forward (6.4 times), pain that occurs in both buttocks or legs (6.3 times), and the presence of neurogenic claudication (3.7 times).[2] On the other hand, the absence of neurogenic claudication makes lumbar stenosis much less likely as the explanation for the pain.[8]
Causes
Spinal stenosis may be congenital (rarely) or acquired (degenerative), overlapping changes normally seen in the aging spine.[6][7] Stenosis can occur as either central stenosis (the narrowing of the entire canal) or foraminal stenosis (the narrowing of the foramen through which the nerve root exits the spinal canal). Severe narrowing of the lateral portion of the canal is called lateral recess stenosis. The ligamentum flavum (yellow ligament), an important structural component intimately adjacent to the posterior portion of the dural sac (nerve sac) can become thickened and cause stenosis. The articular facets, also in the posterior portion of the bony spine can become thickened and enlarged, causing stenosis. These changes are often called "trophic changes" or "facet trophism" in radiology reports. As the canal becomes smaller, resembling a triangular shape, it is called a "trefoil" canal.
Degenerative spondylolisthesis
Forward displacement of a proximal vertebra in relation to its adjacent vertebra in association with an intact neural arch, and in the presence of degenerative changes, is known as degenerative spondylolisthesis,[9][10] which narrows the spinal canal, and symptoms of spinal stenosis are common. Of these, neural claudication is most common. Any forward slipping of one vertebra on another can cause spinal stenosis by narrowing the canal. If this forward slipping narrows the canal sufficiently, and impinges on the contents of the spinal column, it is spinal stenosis by definition. If associated symptoms of narrowing exist, the diagnosis of spinal stenosis is confirmed. With increasing age, the occurrence of degenerative spondylolisthesis becomes more common. The most common spondylolisthesis occurs with slipping of L4 on L5. Frymoyer showed that spondylolisthesis with canal stenosis is more common in diabetic women who have undergone oophorectomy (removal of ovaries). The cause of symptoms in the legs can be difficult to determine. A peripheral neuropathy secondary to diabetes can have the same symptoms as spinal stenosis.[11]
Ankylosing spondylitis
 L5 S1 Spondylolisthesis Grade II with forward slipping of L5 on S1 <50%
L5 S1 Spondylolisthesis Grade II with forward slipping of L5 on S1 <50% Lumbar spine showing advanced ankylosing spondylitis which can lead to spinal stenosis
Lumbar spine showing advanced ankylosing spondylitis which can lead to spinal stenosis
Diagnosis

The diagnosis is based on clinical findings.[7] Some patients can have a narrowed canal without symptoms, and do not require therapy.
The normal lumbar central canal has a midsagittal diameter (front to back) greater than 13 mm, with an area of 1.45 cm2. Relative stenosis is said to exist when the anterior-posterior canal diameter measures between 10 and 13 mm. Absolute stenosis of the lumbar canal exists anatomically when the anterior-posterior measurement is 10 mm or less.[12][13][14]
Plain X-rays of the lumbar or cervical spine may or may not show spinal stenosis. The definitive diagnosis is established by either computerized tomography or magnetic resonance imaging (MRI) scanning. Identifying the presence of a narrowed canal makes the diagnosis of spinal stenosis.[15][16][17]
Bicycle test of van Gelderen
In 1977, Dyck and Doyle reported on the bicycle test, a simple procedure in which the patient is asked to pedal on a stationary bicycle. If the symptoms are caused by peripheral artery disease, the patient will experience claudication, a sensation of not getting enough blood to the legs; if the symptoms are caused by lumbar stenosis, symptoms will be relieved when the patient is leaning forward while bicycling. Although diagnostic progress has been made with newer technical advances, the bicycle test remains an inexpensive and easy way to distinguish between claudication caused by vascular disease and spinal stenosis.[18]
MRI

MRI is the preferred method of diagnosing and evaluating spinal stenosis of all areas of the spine, including cervical, thoracic, and lumbar.[19][20] MRI is useful to diagnose cervical spondylotic myelopathy (degenerative arthritis of the cervical spine with associated damage to the spinal cord).[21] The finding of degeneration of the cervical spinal cord on MRI can be ominous; the condition is called myelomalacia or cord degeneration. It is seen as an increased signal on the MRI. In myelopathy (pathology of the spinal cord) from degenerative changes, the findings are usually permanent and decompressive laminectomy will not reverse the pathology. Surgery can stop the progression of the condition. In cases where the MRI changes are due to vitamin B12 deficiency, a brighter prospect for recovery can be expected.[22][23][24]
Establishing the diagnosis
The detection of spinal stenosis in the cervical, thoracic, or lumbar spine confirms only the anatomic presence of a stenotic condition. This may or may not correlate with the diagnosis of spinal stenosis which is based on clinical findings of radiculopathy, neurogenic claudication, weakness, bowel and bladder dysfunction, spasticity, motor weakness, hyperreflexia and muscular atrophy. These findings, taken from the history and physical examination of the patient (along with the anatomic demonstration of stenosis with an MRI or CT scan), establish the diagnosis.[25]
Management
Nonoperative therapies and laminectomy are the standard treatment for LSS.[26] A trial of conservative treatment is typically recommended.[7] Individuals are generally advised to avoid stressing the lower back, particularly with the spine extended. A physical-therapy program to provide core strengthening and aerobic conditioning may be recommended.[7] Overall scientific evidence is inconclusive on whether conservative approach or a surgical treatment is better for lumbar spinal stenosis.[27]
Medication
The evidence for the use of medical interventions for LSS is poor.[28] Injectable but not nasal calcitonin may be useful for short-term pain relief.[28] Epidural blocks may also transiently decrease pain, but no evidence of long-term effect has been found.[28] Adding corticosteroids to these injections does not improve the result;[28][29] the use of epidural steroid injections is controversial and evidence of their efficacy is contradictory.[7]
Nonsteroidal anti-inflammatory drugs, muscle relaxants, and opioid analgesics are often used to treat low back pain, but evidence of their efficacy is lacking.[7]
Surgery
Surgery appears to lead to better outcomes if symptoms continue after 3–6 months of conservative treatment.[30] Laminectomy is the most effective of the surgical treatments.[26] In those who worsen despite conservative treatments surgery leads to improvement in 60–70% of cases.[7] Another procedure using an interspinous distraction device known as X-STOP was less effective and more expensive when more than one spinal levels are repaired.[26] Both surgical procedures are more expensive than medical management.[26]
Prognosis
Most people with mild to moderate symptoms do not get worse.[7] While many improve in the short term after surgery, this improvement decreases somewhat with time.[7] A number of factors present before surgery are able to predict the outcome after surgery, with people with depression, cardiovascular disease, and scoliosis doing in general worse, while those with more severe stenosis beforehand and better overall health doing better.[6]
The natural evolution of disc disease and degeneration leads to stiffening of the intervertebral joint. This leads to osteophyte formation—a bony overgrowth about the joint. This process is called spondylosis, and is part of the normal aging of the spine. This has been seen in studies of normal and diseased spines. Degenerative changes begin to occur without symptoms as early as age 25–30 years. Not uncommonly, people experience at least one severe case of low back pain by the age of 35. This can be expected to improve and become less prevalent as the individual develops osteophyte formation around the discs.[31]
In the US workers' compensation system, once the threshold of two major spinal surgeries is reached, the vast majority of workers never return to any form of gainful employment. Beyond two spinal surgeries, any more are likely to make the patient worse, not better.[32]
Epidemiology
There are many causes for spinal stenosis but degenerative changes are a precursor to spinal stenosis becoming symptomatic.[33] While the exact prevalence of degenerative LSS is unknown, it is estimated that it ranges from 1.7% - 13.1%.[34] However, the results from these statistics have been put into question. This is mainly due to unclear diagnostic criteria. For example, magnetic resonance imaging (MRI) and computed tomography (CT) are the most common ways to diagnosis LSS, but clinically significant definitions of canal, foraminal, or subarticular narrowing do not exist.
In addition to this, the lumbar and cervical types are more common than the rarer thoracic stenosis.[35] Although stenosis can be found isolated in one region of the spine, developmental spinal stenosis will most likely involve both the cervical and lumbar sections.[36]
The age that people develop spinal stenosis is correlated with change in the joint's biomechanics.[33] Because of this, there has been a recent increasing trend seen by physicians, of lumbar spinal stenosis being more commonly diagnosed in older patients. Low back pain accounts for 17% of all physician visits of people aged 65 and older.[37] From this population, a large portion of radicular pain stems not from disk pathology, but from lumbar spinal stenosis.[37] According to Kalff et al., 21% of people over the age of 60 have lumbar spinal stenosis, as confirmed by radiological screening.[38] Degenerative lumbar spinal stenosis has been predominantly seen in the 50 to 60-year-old population. A recent study in Japan found that the incidence of LSS increases with age. The study supports that LSS incidence increases incrementally in the following age groups, 1.7–2.2% in 40–49 years old population, and 10.3%–11.2% in 70–79 years old population.[39] It is estimated that around 200,000 adults are affected by LSS in the United States and that by the year 2025, this number will rise to 64 million elderly.[34] The syndrome occurs in 12% of older community-dwelling men[40] and up to 21% of those in retirement communities.[37]
Spinal stenosis generally affects more men than women. A study in Geneva found that the ratio between men and women is 1.28.[41] It went on to state that while the disease is strongly related to aging, men are affected earlier in life than women. This is likely due to heavy workload and a higher body mass index (BMI).[41] Although spinal stenosis tends to affect men more than women, degenerative spondylolisthesis in association with spinal stenosis is more prevalent in women.[33] Occupation, race, and smaller canal diameter also do not appear to have a correlation with the development of spinal stenosis.[33]
Furthermore, there is now a disproportionate rise in spinal surgery being performed. The incidence in the 1980s in Sweden was 5 per 100,000 people and increased 300% between 1987 and 1999.[42] Again in 2013, Sweden reported an incidence of 40 per 100,000 people.[42] The large increase in surgical treatment for this disease is well known and studied. The United States has also followed similar trends.
History
A description of LSS was published by Sachs and Frankel in 1900,[43] but the first clinical description of LSS is usually attributed to the Dutch neurosurgeon Henk Verbiest, whose report appeared in 1954.[6][7][44]
Spinal stenosis began to be recognized as an impairing condition in the 1950s and 1970s. Individuals who experience back pain and other symptoms are likely to have bigger spinal canals than those who are asymptomatic.[45] A normal-sized lumbar canal is rarely encountered in persons with either disc disease or those requiring a laminectomy.[31]
During the 1970s and 1980s, many case reports showed successful surgical treatment rates, but these were based on subjective assessment by surgeons.[7] In 1992, Johnsson, Rosén and Udén described the natural history of LSS, with different conclusions about prognosis and treatment: "70% of patients reported no significant change in symptoms, 15% showed significant improvement, whereas 15% showed some deterioration.[46] The investigators concluded that observation is a reasonable treatment option for lumbar stenosis and that significant neurologic deterioration is rare."[7]
Society and culture
United States
Under rules promulgated by Titles II and XVI of the United States Social Security Act, spinal stenosis is recognized as a disabling condition under Listing 1.04 C. The listing states: "Lumbar spinal stenosis resulting in neurogenic claudication, established by findings on appropriate medically acceptable imaging, manifested by chronic nonradicular pain and weakness, and resulting in inability to ambulate effectively, as defined in 1.00B2b."[47] The regulation is written specifically for lumbar stenosis.[48]
References
- Lurie, J; Tomkins-Lane, C (January 2016). "Management of lumbar spinal stenosis". BMJ. 352: h6234. doi:10.1136/bmj.h6234. PMC 6887476. PMID 26727925.
- Suri P, Rainville J, Kalichman L, Katz JN (December 2010). "Does this older adult with lower extremity pain have the clinical syndrome of lumbar spinal stenosis?". JAMA. 304 (23): 2628–36. doi:10.1001/jama.2010.1833. PMC 3260477. PMID 21156951.
- Vogt MT, Cawthon PM, Kang JD, Donaldson WF, Cauley JA, Nevitt MC (June 2006). "Prevalence of symptoms of cervical and lumbar stenosis among participants in the Osteoporotic Fractures in Men Study". Spine. 31 (13): 1445–51. doi:10.1097/01.brs.0000219875.19688.a6. PMID 16741453. S2CID 12388628.
- Hicks GE, Gaines JM, Shardell M, Simonsick EM (September 2008). "Associations of back and leg pain with health status and functional capacity of older adults: findings from the retirement community back pain study". Arthritis and Rheumatism. 59 (9): 1306–13. doi:10.1002/art.24006. PMID 18759261.
- Englund J (January 2007). "Lumbar spinal stenosis". Current Sports Medicine Reports. 6 (1): 50–5. doi:10.1007/s11932-007-0012-0. PMID 17212913. S2CID 32916648.
- Genevay S, Atlas SJ (April 2010). "Lumbar spinal stenosis". Best Practice & Research. Clinical Rheumatology. 24 (2): 253–65. doi:10.1016/j.berh.2009.11.001. PMC 2841052. PMID 20227646.
- Djurasovic M, Glassman SD, Carreon LY, Dimar JR (April 2010). "Contemporary management of symptomatic lumbar spinal stenosis". The Orthopedic Clinics of North America. 41 (2): 183–91. doi:10.1016/j.ocl.2009.12.003. PMID 20399357.
- Konno S, Hayashino Y, Fukuhara S, Kikuchi S, Kaneda K, Seichi A, Chiba K, Satomi K, Nagata K, Kawai S (November 2007). "Development of a clinical diagnosis support tool to identify patients with lumbar spinal stenosis". European Spine Journal. 16 (11): 1951–7. doi:10.1007/s00586-007-0402-2. PMC 2223350. PMID 17549525.
- Takahashi K, Kitahara H, Yamagata M, Murakami M, Takata K, Miyamoto K, Mimura M, Akahashi Y, Moriya H (November 1990). "Long-term results of anterior interbody fusion for treatment of degenerative spondylolisthesis". Spine. 15 (11): 1211–5. doi:10.1097/00007632-199011010-00022. PMID 2267618. S2CID 33682603.
- Wiltse LL, Newman PH, Macnab I (June 1976). "Classification of spondylolisis and spondylolisthesis". Clinical Orthopaedics and Related Research (117): 23–9. doi:10.1097/00003086-197606000-00003. PMID 1277669.
- Frymoyer JW (January 1994). "Degenerative Spondylolisthesis: Diagnosis and Treatment". The Journal of the American Academy of Orthopaedic Surgeons. 2 (1): 9–15. doi:10.5435/00124635-199401000-00002. PMID 10708989. S2CID 19773985.
- Ullrich CG, Binet EF, Sanecki MG, Kieffer SA (January 1980). "Quantitative assessment of the lumbar spinal canal by computed tomography". Radiology. 134 (1): 137–43. doi:10.1148/radiology.134.1.7350593. PMID 7350593.
- Verbiest H (January 1975). "Pathomorphologic aspects of developmental lumbar stenosis". The Orthopedic Clinics of North America. 6 (1): 177–96. doi:10.1016/S0030-5898(20)31210-4. PMID 1113966.
- Eisenstein S (May 1977). "The morphometry and pathological anatomy of the lumbar spine in South African negroes and caucasoids with specific reference to spinal stenosis". The Journal of Bone and Joint Surgery. British Volume. 59 (2): 173–80. doi:10.1302/0301-620X.59B2.873978. PMID 873978.
- Lane JM, Gardner MJ, Lin JT, van der Meulen MC, Myers E (October 2003). "The aging spine: new technologies and therapeutics for the osteoporotic spine". European Spine Journal. 12 (Suppl 2): S147–54. doi:10.1007/s00586-003-0636-6. PMC 3591818. PMID 14534849.
- Benoist M (October 2003). "Natural history of the aging spine". European Spine Journal. 12 (Suppl 2): S86–9. doi:10.1007/s00586-003-0593-0. PMC 3591827. PMID 12961079.
- Szpalski M, Gunzburg R (October 2003). "Lumbar spinal stenosis in the elderly: an overview". European Spine Journal. 12 (Suppl 2): S170–5. doi:10.1007/s00586-003-0612-1. PMC 3591819. PMID 13680315.
- Dyck P, Doyle JB (May 1977). ""Bicycle test" of van Gelderen in diagnosis of intermittent cauda equina compression syndrome. Case report". Journal of Neurosurgery. 46 (5): 667–70. doi:10.3171/jns.1977.46.5.0667. PMID 845655. S2CID 20563075.
- Sheehan NJ (June 2010). "Magnetic resonance imaging for low back pain: indications and limitations". Postgraduate Medical Journal. 86 (1016): 374–8. doi:10.1136/ard.2009.110973. PMID 20547606. S2CID 22850914.
- Cousins JP, Haughton VM (January 2009). "Magnetic resonance imaging of the spine". The Journal of the American Academy of Orthopaedic Surgeons. 17 (1): 22–30. doi:10.5435/00124635-200901000-00004. PMID 19136424. S2CID 3052746.
- Tracy JA, Bartleson JD (May 2010). "Cervical spondylotic myelopathy". The Neurologist. 16 (3): 176–87. doi:10.1097/NRL.0b013e3181da3a29. PMID 20445427. S2CID 32781902.
- Kiers L, Desmond P (January 1999). "Magnetic resonance imaging in subacute combined degeneration of the spinal cord". Journal of Clinical Neuroscience. 6 (1): 49–50. doi:10.1016/S0967-5868(99)90604-5. PMID 18639123. S2CID 8357189.
- Rimbot A, Juglard R, Stéphant E, Bernard C, Aczel F, Talarmin B, Paoletti H, Artéaga C (March 2004). "[Subacute combined degeneration of the spinal cord: contribution of MRI]". Journal de Radiologie (in French). 85 (3): 326–8. doi:10.1016/S0221-0363(04)97586-5. PMID 15192526.
- Srikanth SG, Jayakumar PN, Vasudev MK, Taly AB, Chandrashekar HS (September 2002). "MRI in subacute combined degeneration of spinal cord: a case report and review of literature". Neurology India. 50 (3): 310–2. PMID 12391459.
- "Back Pain | Lower Back Pain | Sciatica |". Boulder Neurological Associates. Archived from the original on 4 March 2016. Retrieved 2014-08-27.
- Burnett MG, Stein SC, Bartels RH (July 2010). "Cost-effectiveness of current treatment strategies for lumbar spinal stenosis: nonsurgical care, laminectomy, and X-STOP". Journal of Neurosurgery. Spine. 13 (1): 39–46. doi:10.3171/2010.3.SPINE09552. PMID 20594016. S2CID 21155483.
- Zaina F, Tomkins-Lane C, Carragee E, Negrini S (January 2016). "Surgical versus non-surgical treatment for lumbar spinal stenosis". The Cochrane Database of Systematic Reviews. 1 (1): CD010264. doi:10.1002/14651858.CD010264.pub2. PMC 6669253. PMID 26824399.
- Tran DQ, Duong S, Finlayson RJ (July 2010). "Lumbar spinal stenosis: a brief review of the nonsurgical management". Canadian Journal of Anaesthesia. 57 (7): 694–703. doi:10.1007/s12630-010-9315-3. PMID 20428988.
- Parr AT, Diwan S, Abdi S (2009). "Lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain: a systematic review". Pain Physician. 12 (1): 163–88. doi:10.36076/ppj.2009/12/163. PMID 19165302.
- Kovacs FM, Urrútia G, Alarcón JD (September 2011). "Surgery versus conservative treatment for symptomatic lumbar spinal stenosis: a systematic review of randomized controlled trials". Spine. 36 (20): E1335–51. doi:10.1097/BRS.0b013e31820c97b1. PMID 21311394. S2CID 26245633.
- Rothman R, Semeone FA, eds. (1982). The Spine. Philadelphia: Saunders. p. 518. ISBN 978-0-7216-7718-7.
- Waddell G, Kummel EG, Lotto WN, Graham JD, Hall H, McCulloch JA (March 1979). "Failed lumbar disc surgery and repeat surgery following industrial injuries". The Journal of Bone and Joint Surgery. American Volume. 61 (2): 201–7. doi:10.2106/00004623-197961020-00007. PMID 422604.
- Martinelli, T. A.; Wiesel, S. W. (1992). "Epidemiology of spinal stenosis". Instructional Course Lectures. 41: 179–181. ISSN 0065-6895. PMID 1588062.
- Kalichman, Leonid; Cole, Robert; Kim, David H.; Li, Ling; Suri, Pradeep; Guermazi, Ali; Hunter, David J. (2009). "Spinal stenosis prevalence and association with symptoms: the Framingham Study". The Spine Journal. 9 (7): 545–550. doi:10.1016/j.spinee.2009.03.005. ISSN 1529-9430. PMC 3775665. PMID 19398386.
- "Differentiating Lumbar, Cervical, and Thoracic Spinal Stenosis". Tuckahoe Orthopaedics. 2017-03-20. Retrieved 2018-11-16.
- Miyazaki, Masashi; Kodera, Ryuzo; Yoshiiwa, Toyomi; Kawano, Masanori; Kaku, Nobuhiro; Tsumura, Hiroshi (2015). "Prevalence and Distribution of Thoracic and Lumbar Compressive Lesions in Cervical Spondylotic Myelopathy". Asian Spine Journal. 9 (2): 218–24. doi:10.4184/asj.2015.9.2.218. ISSN 1976-1902. PMC 4404536. PMID 25901233.
- Hicks, Gregory E.; Gaines, Jean M.; Shardell, Michelle; Simonsick, Eleanor M. (2008-09-15). "Associations of back and leg pain with health status and functional capacity of older adults: Findings from the retirement community back pain study". Arthritis & Rheumatism. 59 (9): 1306–1313. doi:10.1002/art.24006. ISSN 0004-3591. PMID 18759261.
- Kalff, Rolf; Ewald, Christian; Waschke, Albrecht; Gobisch, Lars; Hopf, Christof (2013-09-13). "Degenerative Lumbar Spinal Stenosis in Older People". Deutsches Ärzteblatt Online (in German). 110 (37): 613–23, quiz 624. doi:10.3238/arztebl.2013.0613. ISSN 1866-0452. PMC 3784039. PMID 24078855.
- Wu, Ai-Min; Zou, Fei; Cao, Yong; Xia, Dong-Dong; He, Wei; Zhu, Bin; Chen, Dong; Ni, Wen-Fei; Wang, Xiang-Yang (2017-05-26). "Lumbar spinal stenosis: an update on the epidemiology, diagnosis and treatment". AME Medical Journal. 2 (5): 63. doi:10.21037/amj.2017.04.13. hdl:10722/245163.
- Vogt, Molly T.; Cawthon, Peggy Mannen; Kang, James D.; Donaldson, William F.; Cauley, Jane A.; Nevitt, Michael C. (June 2006). "Prevalence of Symptoms of Cervical and Lumbar Stenosis Among Participants in the Osteoporotic Fractures in Men Study". Spine. 31 (13): 1445–1451. doi:10.1097/01.brs.0000219875.19688.a6. ISSN 0362-2436. PMID 16741453. S2CID 12388628.
- Berney, J. (1994). "[Epidemiology of narrow spinal canal]". Neuro-Chirurgie. 40 (3): 174–178. ISSN 0028-3770. PMID 7723924.
- Wessberg, Per; Frennered, Karin (2017-04-17). "Central lumbar spinal stenosis: natural history of non-surgical patients". European Spine Journal. 26 (10): 2536–2542. doi:10.1007/s00586-017-5075-x. ISSN 0940-6719. PMID 28417234.
- Sachs B, Frankel V (1900). "Progressive and kyphotic rigidity of the spine". J Nerv Ment Dis. 27: 1–15. doi:10.1097/00005053-190001000-00001. S2CID 144648117.
- Verbiest H (May 1954). "A radicular syndrome from developmental narrowing of the lumbar vertebral canal". The Journal of Bone and Joint Surgery. British Volume. 36-B (2): 230–7. doi:10.1302/0301-620X.36B2.230. PMID 13163105. Archived from the original (PDF) on 2011-07-24. Retrieved 2010-12-26.
- Porter RW, Hibbert CS, Wicks M (November 1978). "The spinal canal in symptomatic lumbar disc lesions". The Journal of Bone and Joint Surgery. British Volume. 60-B (4): 485–7. doi:10.1302/0301-620X.60B4.711794. PMID 711794. Archived from the original on 2011-07-24. Retrieved 2010-12-25.
- Johnsson KE, Rosén I, Udén A (June 1992). "The natural course of lumbar spinal stenosis". Clinical Orthopaedics and Related Research (279): 82–6. PMID 1534726.
- "Disability programs". US Social Security Administration. September 2008. Retrieved December 26, 2010.
- "Disability Evaluation Under Social Security" (PDF). US Social Security Administration. January 2003. Archived from the original (PDF) on January 1, 2011. Retrieved December 26, 2010.