Low back pain
Low back pain (LBP) or lumbago is a common disorder involving the muscles, nerves, and bones of the back,[4] in between the lower edge of the ribs and the lower fold of the buttocks. Pain can vary from a dull constant ache to a sudden sharp feeling.[4] Low back pain may be classified by duration as acute (pain lasting less than 6 weeks), sub-chronic (6 to 12 weeks), or chronic (more than 12 weeks).[3] The condition may be further classified by the underlying cause as either mechanical, non-mechanical, or referred pain.[5] The symptoms of low back pain usually improve within a few weeks from the time they start, with 40–90% of people recovered by six weeks.[2]
| Low back pain | |
|---|---|
| Other names | Lower back pain, lumbago |
 | |
| Low back pain is a common and costly complaint. | |
| Pronunciation |
|
| Specialty | Orthopedics, rheumatology, rehabilitation medicine |
| Usual onset | 20 to 40 years of age[1] |
| Duration | ~65% get better in 6 weeks[2] |
| Types | Acute (less than 6 weeks), sub-chronic (6 to 12 weeks), chronic (more than 12 weeks)[3] |
| Causes | Usually non-specific, occasionally significant underlying cause[1][4] |
| Diagnostic method | Medical imaging (if red flags )[5] |
| Treatment | Continued normal activity, non-medication based treatments, NSAIDs[2][6] |
| Frequency | ~25% in any given month[7][8] |
In most episodes of low back pain, a specific underlying cause is not identified or even looked for, with the pain believed to be due to mechanical problems such as muscle or joint strain.[1][4] If the pain does not go away with conservative treatment or if it is accompanied by "red flags" such as unexplained weight loss, fever, or significant problems with feeling or movement, further testing may be needed to look for a serious underlying problem.[5] In most cases, imaging tools such as X-ray computed tomography are not useful and carry their own risks.[9][10] Despite this, the use of imaging in low back pain has increased.[11] Some low back pain is caused by damaged intervertebral discs, and the straight leg raise test is useful to identify this cause.[5] In those with chronic pain, the pain processing system may malfunction, causing large amounts of pain in response to non-serious events.[12]
Initial management with non-medication based treatments is recommended.[6] NSAIDs are recommended if these are not sufficiently effective.[6] Normal activity should be continued as much as the pain allows.[2] A number of other options are available for those who do not improve with usual treatment. Opioids may be useful if simple pain medications are not enough, but they are not generally recommended due to side effects.[4][13] Surgery may be beneficial for those with disc-related chronic pain and disability or spinal stenosis.[14][15] No clear benefit of surgery has been found for other cases of non-specific low back pain.[14] Low back pain often affects mood, which may be improved by counseling or antidepressants.[13][16] Additionally, there are many alternative medicine therapies, including the Alexander technique and herbal remedies, but there is not enough evidence to recommend them confidently.[17] The evidence for chiropractic care[18] and spinal manipulation is mixed.[17][19][20][21]
Approximately 9–12% of people (632 million) have LBP at any given point in time, and nearly 25% report having it at some point over any one-month period.[7][8] About 40% of people have LBP at some point in their lives,[7] with estimates as high as 80% among people in the developed world.[22] Difficulty most often begins between 20 and 40 years of age.[1] Men and women are equally affected.[4] Low back pain is more common among people aged between 40 and 80 years, with the overall number of individuals affected expected to increase as the population ages.[7]
Signs and symptoms
In the common presentation of acute low back pain, pain develops after movements that involve lifting, twisting, or forward-bending. The symptoms may start soon after the movements or upon waking up the following morning. The description of the symptoms may range from tenderness at a particular point to diffuse pain. It may or may not worsen with certain movements, such as raising a leg, or positions, such as sitting or standing. Pain radiating down the legs (known as sciatica) may be present. The first experience of acute low back pain is typically between the ages of 20 and 40. This is often a person's first reason to see a medical professional as an adult.[1] Recurrent episodes occur in more than half of people[23] with the repeated episodes being generally more painful than the first.[1]
Other problems may occur along with low back pain. Chronic low back pain is associated with sleep problems, including a greater amount of time needed to fall asleep, disturbances during sleep, a shorter duration of sleep, and less satisfaction with sleep.[24] In addition, a majority of those with chronic low back pain show symptoms of depression[13] or anxiety.[17]
Causes

Low back pain is not a specific disease but rather a complaint that may be caused by a large number of underlying problems of varying levels of seriousness.[25] The majority of LBP does not have a clear cause[1] but is believed to be the result of non-serious muscle or skeletal issues such as sprains or strains.[26] Obesity, smoking, weight gain during pregnancy, stress, poor physical condition, and poor sleeping position may also contribute to low back pain.[26] There is no consensus as to whether spinal posture or certain physical activities are causal factors.[27] A full list of possible causes includes many less common conditions.[5] Physical causes may include osteoarthritis, degeneration of the discs between the vertebrae or a spinal disc herniation, broken vertebra(e) (such as from osteoporosis) or, rarely, an infection or tumor of the spine.[28]
Women may have acute low back pain from medical conditions affecting the female reproductive system, including endometriosis, ovarian cysts, ovarian cancer, or uterine fibroids.[29] Nearly half of all pregnant women report pain in the lower back or sacral area during pregnancy, due to changes in their posture and center of gravity causing muscle and ligament strain.[30]
Low back pain can be broadly classified into four main categories:
- Musculoskeletal – mechanical (including muscle strain, muscle spasm, or osteoarthritis); herniated nucleus pulposus, herniated disc; spinal stenosis; or compression fracture
- Inflammatory – HLA-B27 associated arthritis including ankylosing spondylitis, reactive arthritis, psoriatic arthritis, inflammation within the reproductive system, and inflammatory bowel disease
- Malignancy – bone metastasis from lung, breast, prostate, thyroid, among others
- Infectious – osteomyelitis; abscess
Low back pain can also be caused by an urinary tract infection.[31]
Pathophysiology
Back structures
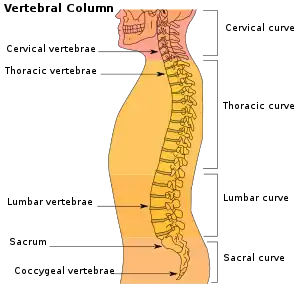

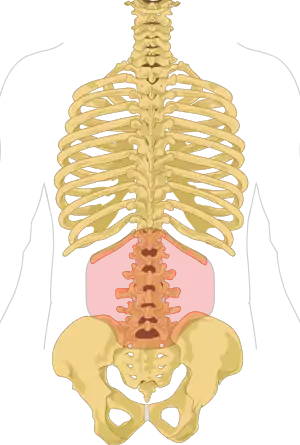
The lumbar (or lower back) region is the area between the lower ribs and gluteal fold which includes five lumbar vertebrae (L1–L5) and the sacrum. In between these vertebrae are fibrocartilaginous discs, which act as cushions, preventing the vertebrae from rubbing together while at the same time protecting the spinal cord. Nerves come from and go to the spinal cord through specific openings between the vertebrae, providing the skin with sensations and sending messages to muscles. Stability of the spine is provided by the ligaments and muscles of the back and abdomen. Small joints called facet joints limit and direct the motion of the spine.[32]
The multifidus muscles run up and down along the back of the spine, and are important for keeping the spine straight and stable during many common movements such as sitting, walking and lifting.[12] A problem with these muscles is often found in someone with chronic low back pain, because the back pain causes the person to use the back muscles improperly in trying to avoid the pain.[33] The problem with the multifidus muscles continues even after the pain goes away, and is probably an important reason why the pain comes back.[33] Teaching people with chronic low back pain how to use these muscles is recommended as part of a recovery program.[33]
An intervertebral disc has a gelatinous core surrounded by a fibrous ring.[34] When in its normal, uninjured state, most of the disc is not served by either the circulatory or nervous systems – blood and nerves only run to the outside of the disc.[34] Specialized cells that can survive without direct blood supply are in the inside of the disc.[34] Over time, the discs lose flexibility and the ability to absorb physical forces.[25] This decreased ability to handle physical forces increases stresses on other parts of the spine, causing the ligaments of the spine to thicken and bony growths to develop on the vertebrae.[25] As a result, there is less space through which the spinal cord and nerve roots may pass.[25] When a disc degenerates as a result of injury or disease, the makeup of a disc changes: blood vessels and nerves may grow into its interior and/or herniated disc material can push directly on a nerve root.[34] Any of these changes may result in back pain.[34]
Pain sensation
Pain is generally an unpleasant feeling in response to an event that either damages or can potentially damage the body's tissues. There are four main steps in the process of feeling pain: transduction, transmission, perception, and modulation.[12] The nerve cells that detect pain have cell bodies located in the dorsal root ganglia and fibers that transmit these signals to the spinal cord.[35] The process of pain sensation starts when the pain-causing event triggers the endings of appropriate sensory nerve cells. This type of cell converts the event into an electrical signal by transduction. Several different types of nerve fibers carry out the transmission of the electrical signal from the transducing cell to the posterior horn of spinal cord, from there to the brain stem, and then from the brain stem to the various parts of the brain such as the thalamus and the limbic system. In the brain, the pain signals are processed and given context in the process of pain perception. Through modulation, the brain can modify the sending of further nerve impulses by decreasing or increasing the release of neurotransmitters.[12]
Parts of the pain sensation and processing system may not function properly; creating the feeling of pain when no outside cause exists, signaling too much pain from a particular cause, or signaling pain from a normally non-painful event. Additionally, the pain modulation mechanisms may not function properly. These phenomena are involved in chronic pain.[12]
Diagnosis
As the structure of the lumbago back is complex and the reporting of pain is subjective and affected by social factors, the diagnosis of low back pain is not straightforward.[5] While most low back pain is caused by muscle and joint problems, this cause must be separated from neurological problems, spinal tumors, fracture of the spine, and infections, among others.[3][1]
Classification
There are a number of ways to classify low back pain with no consensus that any one method is best.[5] There are three general types of low back pain by cause: mechanical back pain (including nonspecific musculoskeletal strains, herniated discs, compressed nerve roots, degenerative discs or joint disease, and broken vertebra), non-mechanical back pain (tumors, inflammatory conditions such as spondyloarthritis, and infections), and referred pain from internal organs (gallbladder disease, kidney stones, kidney infections, and aortic aneurysm, among others).[5] Mechanical or musculoskeletal problems underlie most cases (around 90% or more),[5][36] and of those, most (around 75%) do not have a specific cause identified, but are thought to be due to muscle strain or injury to ligaments.[5][36] Rarely, complaints of low back pain result from systemic or psychological problems, such as fibromyalgia and somatoform disorders.[36]
Low back pain may be classified based on the signs and symptoms. Diffuse pain that does not change in response to particular movements, and is localized to the lower back without radiating beyond the buttocks, is classified as nonspecific, the most common classification.[5] Pain that radiates down the leg below the knee, is located on one side (in the case of disc herniation), or is on both sides (in spinal stenosis), and changes in severity in response to certain positions or maneuvers is radicular, making up 7% of cases.[5] Pain that is accompanied by red flags such as trauma, fever, a history of cancer or significant muscle weakness may indicate a more serious underlying problem and is classified as needing urgent or specialized attention.[5]
The symptoms can also be classified by duration as acute, sub-chronic (also known as sub-acute), or chronic. The specific duration required to meet each of these is not universally agreed upon, but generally pain lasting less than six weeks is classified as acute, pain lasting six to twelve weeks is sub-chronic, and more than twelve weeks is chronic.[3] Management and prognosis may change based on the duration of symptoms.
Red flags
| Red flag[37] | Possible cause[1] |
|---|---|
| Previous history of cancer | Cancer |
| Unintentional weight loss | |
| Loss of bladder or bowel control | Cauda equina syndrome |
| Significant motor weakness or sensory problems | |
| Loss of sensation in the buttocks (saddle anesthesia) | |
| Significant trauma related to age | Fracture |
| Chronic corticosteroid use | |
| Osteoporosis | |
| Severe pain after lumbar surgery in past year | Infection |
| Fever | |
| Urinary tract infection | |
| Immunosuppression | |
| Intravenous drug use |
The presence of certain signs, termed red flags, indicate the need for further testing to look for more serious underlying problems, which may require immediate or specific treatment.[5][38] The presence of a red flag does not mean that there is a significant problem. It is only suggestive,[39][40] and most people with red flags have no serious underlying problem.[3][1] If no red flags are present, performing diagnostic imaging or laboratory testing in the first four weeks after the start of the symptoms has not been shown to be useful.[5]
The usefulness of many red flags is poorly supported by evidence.[41][42] The most useful for detecting a fracture are: older age, corticosteroid use, and significant trauma especially if it results in skin markings.[41] The best determinant of the presence of cancer is a history of the same.[41]
With other causes ruled out, people with non-specific low back pain are typically treated symptomatically, without exact determination of the cause.[3][1] Efforts to uncover factors that might complicate the diagnosis, such as depression, substance abuse, or an agenda concerning insurance payments may be helpful.[5]
Tests

Imaging is indicated when there are red flags, ongoing neurological symptoms that do not resolve, or ongoing or worsening pain.[5] In particular, early use of imaging (either MRI or CT) is recommended for suspected cancer, infection, or cauda equina syndrome.[5] MRI is slightly better than CT for identifying disc disease; the two technologies are equally useful for diagnosing spinal stenosis.[5] Only a few physical diagnostic tests are helpful.[5] The straight leg raise test is almost always positive in those with disc herniation,[5] and lumbar provocative discography may be useful to identify a specific disc causing pain in those with chronic high levels of low back pain.[43] Therapeutic procedures such as nerve blocks can also be used to determine a specific source of pain.[5] Some evidence supports the use of facet joint injections, transforminal epidural injections and sacroiliac injections as diagnostic tests.[5] Most other physical tests, such as evaluating for scoliosis, muscle weakness or wasting, and impaired reflexes, are of little use.[5]
Complaints of low back pain are one of the most common reasons people visit doctors.[9][44] For pain that has lasted only a few weeks, the pain is likely to subside on its own.[45] Thus, if a person's medical history and physical examination do not suggest a specific disease as the cause, medical societies advise against imaging tests such as X-rays, CT scans, and MRIs.[44] Individuals may want such tests but, unless red flags are present,[10][46] they are unnecessary health care.[9][45] Routine imaging increases costs, is associated with higher rates of surgery with no overall benefit,[47][48] and the radiation used may be harmful to one's health.[47] Fewer than 1% of imaging tests identify the cause of the problem.[9] Imaging may also detect harmless abnormalities, encouraging people to request further unnecessary testing or to worry.[9] Even so, MRI scans of the lumbar region increased by more than 300% among United States Medicare beneficiaries from 1994 to 2006.[11]
Prevention
Exercise appears to be useful for preventing low back pain.[49] Exercise is also probably effective in preventing recurrences in those with pain that has lasted more than six weeks.[1][50] Medium-firm mattresses are more beneficial for chronic pain than firm mattresses.[51] There is little to no evidence that back belts are any more helpful in preventing low back pain than education about proper lifting techniques.[49][52] There is no quality data that supports medium firm mattresses over firm mattresses. A few studies that have contradicted this notion have also failed to include sleep posture and mattress firmness. The most comfortable sleep surface may be preferred.[53] Shoe insoles do not help prevent low back pain.[49][54]
Management
Most people with acute or subacute low back pain improve over time no matter the treatment.[6] There is often improvement within the first month.[6] Recommendations include remaining active, avoiding activity that worsen the pain, and understanding self-care of the symptoms.[6] Management of low back pain depends on which of the three general categories is the cause: mechanical problems, non-mechanical problems, or referred pain.[55] For acute pain that is causing only mild to moderate problems, the goals are to restore normal function, return the individual to work, and minimize pain. The condition is normally not serious, resolves without much being done, and recovery is helped by attempting to return to normal activities as soon as possible within the limits of pain.[3] Providing individuals with coping skills through reassurance of these facts is useful in speeding recovery.[1] For those with sub-chronic or chronic low back pain, multidisciplinary treatment programs may help.[56] Initial management with non–medication based treatments is recommended[6] Non–medication based treatments include superficial heat, massage, acupuncture, or spinal manipulation.[6] If these are not sufficiently effective, NSAIDs are recommended.[6] Acetaminophen and systemic steroids are not recommended as both medications are not effective at improving pain outcomes in acute or subacute low back pain.[6]
Physical therapy stabilization exercises for lumbar spine and manual therapy have shown decrease in pain symptoms in patients. Manual therapy and stabilization effects have similar effects on low back pain which overweighs the effects of general exercises.[57]
Management of acute low back pain
Increasing general physical activity has been recommended, but no clear relationship to pain or disability has been found when used for the treatment of an acute episode of pain.[50][58] For acute pain, low- to moderate-quality evidence supports walking.[59] Aerobic exercises like progressive walking appears useful for subacute and acute low back pain, is strongly recommended for chronic low back pain, and is recommended after surgery.[53] Directional exercises, which try to limit low back pain, are recommended in sub-acute, chronic and radicular low back pain. These exercises only work if they are limiting low back pain.[53] Treatment according to McKenzie method is somewhat effective for recurrent acute low back pain, but its benefit in the short term does not appear significant.[1] There is tentative evidence to support the use of heat therapy for acute and sub-chronic low back pain[60] but little evidence for the use of either heat or cold therapy in chronic pain.[61] Weak evidence suggests that back belts might decrease the number of missed workdays, but there is nothing to suggest that they help with the pain.[52] Ultrasound and shock wave therapies do not appear effective and therefore are not recommended.[62][63] Lumbar traction lacks effectiveness as an intervention for radicular low back pain.[64] It is also unclear whether lumbar supports are an effective treatment intervention.[65] Exercise programs that incorporate stretching only are not recommended for low back pain. Generic or non specific stretching has also been found to not help with acute low back pain. Yoga and Tai chi are not recommended in case of acute or subacute low back pain, but are recommended in case of chronic back pain.[53] Stretching, especially with limited range of motion, can impede future progression of treatment like limiting strength and limiting exercises.[53]
Management of chronic low back pain
Exercise therapy is effective in decreasing pain and improving physical function, trunk muscle strength and the mental health for those with chronic low back pain.[66][67] It also improves long-term function[61] and appears to reduce recurrence rates for as long as six months after the completion of the program.[68] The observed treatment effect for the exercise when compared to no treatment, usual care or placebo, improved pain (low‐certainty evidence), but improvements were small for functional limitations outcomes (moderate‐certainty evidence).[67] There is no evidence that one particular type of exercise therapy is more effective than another,[69][70] so the form of exercise used can be based on patient or practitioner preference, availability and cost. The Alexander technique appears useful for chronic back pain,[71] and there is tentative evidence to support the use of yoga.[72][73] If a person with chronic low back pain is motivated, it is recommended to use yoga and tai chi as a form of treatment, but this is not recommended to treat acute or subacute low back pain.[53] Motor control exercise, which involves guided movement and use of normal muscles during simple tasks which then builds to more complex tasks, improves pain and function up to 20 weeks, but there was little difference compared to manual therapy and other forms of exercise.[74] Motor control exercise accompanied by manual therapy also produces similar reductions in pain intensity when compared to general strength and condition exercise training, yet only the latter also improved muscle endurance and strength, whilst concurrently decreased self-reported disability.[75] Aquatic therapy is recommended as an option in those with other preexisting conditions like extreme obesity, degenerative joint disease, or other conditions that limit progressive walking. Aquatic therapy is recommended for chronic and subacute low back pain in those with a preexisting condition. Aquatic therapy is not recommended for people that have no preexisting condition that limits their progressive walking.[53] There is low-to-moderate quality evidence that supports pilates in low back pain for the reduction of pain and disability,[53][76] however there is no conclusive evidence that pilates is better than any other form of exercise for low back pain.[76]
Patients with chronic low back pain receiving multidisciplinary biopsychosocial rehabilitation (MBR) programs are likely to experience less pain and disability than those receiving usual care or a physical treatment. MBR also has a positive influence on work status of the patient compared to physical treatment. Effects are of a modest magnitude and should be balanced against the time and resource requirements of MBR programs.[77]
Peripheral nerve stimulation, a minimally-invasive procedure, may be useful in cases of chronic low back pain that do not respond to other measures, although the evidence supporting it is not conclusive, and it is not effective for pain that radiates into the leg.[78] Evidence for the use of shoe insoles as a treatment is inconclusive.[54] Transcutaneous electrical nerve stimulation (TENS) has not been found to be effective in chronic low back pain.[79] There has been little research that supports the use of lumbar extension machines and thus they are not recommended.[53]
Medications
The management of low back pain often includes medications for the duration that they are beneficial. With the first episode of low back pain the hope is a complete cure; however, if the problem becomes chronic, the goals may change to pain management and the recovery of as much function as possible. As pain medications are only somewhat effective, expectations regarding their benefit may differ from reality, and this can lead to decreased satisfaction.[13]
The medication typically recommended first are acetaminophen (paracetamol), NSAIDs (though not aspirin), or skeletal muscle relaxants and these are enough for most people.[13][6][80] Benefits with NSAIDs; however, is often small.[81] High-quality reviews have found acetaminophen (paracetamol) to be no more effective than placebo at improving pain, quality of life, or function.[82][83] NSAIDs are more effective for acute episodes than acetaminophen; however, they carry a greater risk of side effects, including kidney failure, stomach ulcers and possibly heart problems. Thus, NSAIDs are a second choice to acetaminophen, recommended only when the pain is not handled by the latter. NSAIDs are available in several different classes; there is no evidence to support the use of COX-2 inhibitors over any other class of NSAIDs with respect to benefits.[81][13][84] With respect to safety naproxen may be best.[85] Muscle relaxants may be beneficial.[13]
If the pain is still not managed adequately, short-term use of opioids such as morphine may be useful.[86][13] These medications carry a risk of addiction, may have negative interactions with other drugs, and have a greater risk of side effects, including dizziness, nausea, and constipation.[13] The effect of long-term use of opioids for lower back pain is unknown.[87] Opioid treatment for chronic low back pain increases the risk for lifetime illicit drug use.[88] Specialist groups advise against general long-term use of opioids for chronic low back pain.[13][89] As of 2016, the CDC has released a guideline for prescribed opioid use in the management of chronic pain.[90] It states that opioid use is not the preferred treatment when managing chronic pain due to the excessive risks involved. If prescribed, a person and their clinician should have a realistic plan to discontinue its use in the event that the risks outweigh the benefit.[90]
For older people with chronic pain, opioids may be used in those for whom NSAIDs present too great a risk, including those with diabetes, stomach or heart problems. They may also be useful for a select group of people with neuropathic pain.[91]
Antidepressants may be effective for treating chronic pain associated with symptoms of depression, but they have a risk of side effects.[13] Although the antiseizure drugs gabapentin, pregabalin, and topiramate are sometimes used for chronic low back pain evidence does not support a benefit.[92] Systemic oral steroids have not been shown to be useful in low back pain.[1][13] Facet joint injections and steroid injections into the discs have not been found to be effective in those with persistent, non-radiating pain; however, they may be considered for those with persistent sciatic pain.[93] Epidural corticosteroid injections provide a slight and questionable short-term improvement in those with sciatica but are of no long-term benefit.[94] There are also concerns of potential side effects.[95]
A study with 80 patients found magnesium to be useful in those with chronic back pain.[96]
Surgery
Surgery may be useful in those with a herniated disc that is causing significant pain radiating into the leg, significant leg weakness, bladder problems, or loss of bowel control.[14] It may also be useful in those with spinal stenosis.[15] In the absence of these issues, there is no clear evidence of a benefit from surgery.[14]
Discectomy (the partial removal of a disc that is causing leg pain) can provide pain relief sooner than nonsurgical treatments.[14] Discectomy has better outcomes at one year but not at four to ten years.[14] The less invasive microdiscectomy has not been shown to result in a different outcome than regular discectomy.[14] For most other conditions, there is not enough evidence to provide recommendations for surgical options.[14] The long-term effect surgery has on degenerative disc disease is not clear.[14] Less invasive surgical options have improved recovery times, but evidence regarding effectiveness is insufficient.[14]
For those with pain localized to the lower back due to disc degeneration, fair evidence supports spinal fusion as equal to intensive physical therapy and slightly better than low-intensity nonsurgical measures.[15] Fusion may be considered for those with low back pain from acquired displaced vertebra that does not improve with conservative treatment,[14] although only a few of those who have spinal fusion experience good results.[15] There are a number of different surgical procedures to achieve fusion, with no clear evidence of one being better than the others.[97] Adding spinal implant devices during fusion increases the risk but provides no added improvement in pain or function.[11]
Alternative medicine
It is unclear if alternative treatments are useful for non-chronic back pain.[98] Chiropractic care or spinal manipulation therapy (SMT) appear similarly effective to other recommended treatments.[99][100][20] National guidelines differ, with some not recommending SMT, some describing manipulation as optional, and others recommending a short course for those who do not improve with other treatments.[3] A 2017 review recommended SMT based on low-quality evidence.[6] There is insufficient evidence to recommend manipulation under anaesthesia, or medically assisted manipulation.[101] SMT does not provide significant benefits compared to motor control exercises.[102]
Acupuncture is no better than placebo, usual care, or sham acupuncture for nonspecific acute pain or sub-chronic pain.[103] For those with chronic pain, it improves pain a little more than no treatment and about the same as medications, but it does not help with disability.[103] This pain benefit is only present right after treatment and not at follow-up.[103] Acupuncture may be a reasonable option for those with chronic pain that does not respond to other treatments like conservative care and medications.[1][104]
Massage therapy does not appear to provide much benefit for acute low back pain.[1] According to a 2015 Cochrane review, massage therapy was more effective for acute low back pain than no treatment; the benefits were limited to the short term[105] and there was no effect for improving function.[105] For chronic low back pain, massage therapy was no better than no treatment for both pain and function, though only in the short-term.[105] The overall quality of the evidence was low and the authors conclude that massage therapy is generally not an effective treatment for low back pain.[105] Massage therapy is recommended for selected people with subacute and chronic low back pain, but it should be paired with another form of treatment like aerobic or strength exercises. For acute or chronic radicular pain syndromes massage therapy is recommended only if low back pain is considered a symptom. Mechanical massage tools are not recommended for the treatment of any form of low back pain.[53]
Prolotherapy – the practice of injecting solutions into joints (or other areas) to cause inflammation and thereby stimulate the body's healing response – has not been found to be effective by itself, although it may be helpful when added to another therapy.[17]
Herbal medicines, as a whole, are poorly supported by evidence.[106] The herbal treatments Devil's claw and white willow may reduce the number of individuals reporting high levels of pain; however, for those taking pain relievers, this difference is not significant.[17] Capsicum, in the form of either a gel or a plaster cast, has been found to reduce pain and increase function.[17]
Behavioral therapy may be useful for chronic pain.[16] There are several types available, including operant conditioning, which uses reinforcement to reduce undesirable behaviors and increase desirable behaviors; cognitive behavioral therapy, which helps people identify and correct negative thinking and behavior; and respondent conditioning, which can modify an individual's physiological response to pain.[17] The benefit however is small.[107] Medical providers may develop an integrated program of behavioral therapies.[17] The evidence is inconclusive as to whether mindfulness-based stress reduction reduces chronic back pain intensity or associated disability, although it suggests that it may be useful in improving the acceptance of existing pain.[108][109]
Tentative evidence supports neuroreflexotherapy (NRT), in which small pieces of metal are placed just under the skin of the ear and back, for non-specific low back pain.[110][111][17] Multidisciplinary biopsychosocial rehabilitation (MBR), targeting physical and psychological aspects, may improve back pain but evidence is limited.[112] There is a lack of good quality evidence to support the use of radiofrequency denervation for pain relief.[113]
KT Tape has been found to be no different for management of chronic non-specific low back pain than other established pain management strategies.[114]
Education
There is strong evidence that education may improve low back pain, with a 2.5 hour educational session more effective than usual care for helping people return to work in the short- and long-term. This was more effective for people with acute rather than chronic back pain.[115]
Prognosis
Overall, the outcome for acute low back pain is positive. Pain and disability usually improve a great deal in the first six weeks, with complete recovery reported by 40 to 90%.[2] In those who still have symptoms after six weeks, improvement is generally slower with only small gains up to one year. At one year, pain and disability levels are low to minimal in most people. Distress, previous low back pain, and job satisfaction are predictors of long-term outcome after an episode of acute pain.[2] Certain psychological problems such as depression, or unhappiness due to loss of employment may prolong the episode of low back pain.[13] Following a first episode of back pain, recurrences occur in more than half of people.[23]
For persistent low back pain, the short-term outcome is also positive, with improvement in the first six weeks but very little improvement after that. At one year, those with chronic low back pain usually continue to have moderate pain and disability.[2] People at higher risk of long-term disability include those with poor coping skills or with fear of activity (2.5 times more likely to have poor outcomes at one year),[116] those with a poor ability to cope with pain, functional impairments, poor general health, or a significant psychiatric or psychological component to the pain (Waddell's signs).[116]
Prognosis may be influenced by expectations, with those having positive expectations of recovery related to higher likelihood of returning to work and overall outcomes.[117]
Epidemiology
Low back pain that lasts at least one day and limits activity is a common complaint.[7] Globally, about 40% of people have LBP at some point in their lives,[7] with estimates as high as 80% of people in the developed world.[22] Approximately 9 to 12% of people (632 million) have LBP at any given point in time, and nearly one quarter (23.2%) report having it at some point over any one-month period.[7][8] Difficulty most often begins between 20 and 40 years of age.[1] Low back pain is more common among people aged 40–80 years, with the overall number of individuals affected expected to increase as the population ages.[7]
It is not clear whether men or women have higher rates of low back pain.[7][8] A 2012 review reported a rate of 9.6% among males and 8.7% among females.[8] Another 2012 review found a higher rate in females than males, which the reviewers felt was possibly due to greater rates of pains due to osteoporosis, menstruation, and pregnancy among women, or possibly because women were more willing to report pain than men.[7] An estimated 70% of women experience back pain during pregnancy with the rate being higher the further along in pregnancy.[118] Current smokers – and especially those who are adolescents – are more likely to have low back pain than former smokers, and former smokers are more likely to have low back pain than those who have never smoked.[119]
History

Low back pain has been with humans since at least the Bronze Age. The oldest known surgical treatise – the Edwin Smith Papyrus, dating to about 1500 BCE – describes a diagnostic test and treatment for a vertebral sprain. Hippocrates (c. 460 BCE – c. 370 BCE) was the first to use a term for sciatic pain and low back pain; Galen (active mid to late second century CE) described the concept in some detail. Physicians through the end of the first millennium recommended watchful waiting. Through the Medieval period, folk medicine practitioners provided treatments for back pain based on the belief that it was caused by spirits.[120]
At the start of the 20th century, physicians thought low back pain was caused by inflammation of or damage to the nerves,[120] with neuralgia and neuritis frequently mentioned by them in the medical literature of the time.[121] The popularity of such proposed causes decreased during the 20th century.[121] In the early 20th century, American neurosurgeon Harvey Williams Cushing increased the acceptance of surgical treatments for low back pain.[14] In the 1920s and 1930s, new theories of the cause arose, with physicians proposing a combination of nervous system and psychological disorders such as nerve weakness (neurasthenia) and female hysteria.[120] Muscular rheumatism (now called fibromyalgia) was also cited with increasing frequency.[121]
Emerging technologies such as X-rays gave physicians new diagnostic tools, revealing the intervertebral disc as a source for back pain in some cases. In 1938, orthopedic surgeon Joseph S. Barr reported on cases of disc-related sciatica improved or cured with back surgery.[121] As a result of this work, in the 1940s, the vertebral disc model of low back pain took over,[120] dominating the literature through the 1980s, aiding further by the rise of new imaging technologies such as CT and MRI.[121] The discussion subsided as research showed disc problems to be a relatively uncommon cause of the pain. Since then, physicians have come to realize that it is unlikely that a specific cause for low back pain can be identified in many cases and question the need to find one at all as most of the time symptoms resolve within 6 to 12 weeks regardless of treatment.[120]
Society and culture
Low back pain results in large economic costs. In the United States, it is the most common type of pain in adults, responsible for a large number of missed work days, and is the most common musculoskeletal complaint seen in the emergency department.[25] In 1998, it was estimated to be responsible for $90 billion in annual health care costs, with 5% of individuals incurring most (75%) of the costs.[25] Between 1990 and 2001 there was a more than twofold increase in spinal fusion surgeries in the US, despite the fact that there were no changes to the indications for surgery or new evidence of greater usefulness.[11] Further costs occur in the form of lost income and productivity, with low back pain responsible for 40% of all missed work days in the United States.[122] Low back pain causes disability in a larger percentage of the workforce in Canada, Great Britain, the Netherlands and Sweden than in the US or Germany.[122] In the United States, Low Back pain is highest of Years Lived With Disability (YLDs) Rank, Rate, and Percentage Change for the 25 Leading Causes of Disability and Injury, between 1990 and 2016.[123]
Workers who experience acute low back pain as a result of a work injury may be asked by their employers to have x-rays.[124] As in other cases, testing is not indicated unless red flags are present.[124] An employer's concern about legal liability is not a medical indication and should not be used to justify medical testing when it is not indicated.[124] There should be no legal reason for encouraging people to have tests which a health care provider determines are not indicated.[124]
Research
Total disc replacement is an experimental option,[34] but no significant evidence supports its use over lumbar fusion.[14] Researchers are investigating the possibility of growing new intervertebral structures through the use of injected human growth factors, implanted substances, cell therapy, and tissue engineering.[34]
References
- Casazza BA (February 2012). "Diagnosis and treatment of acute low back pain". American Family Physician. 85 (4): 343–350. PMID 22335313.
- da C Menezes Costa L, Maher CG, Hancock MJ, McAuley JH, Herbert RD, Costa LO (August 2012). "The prognosis of acute and persistent low-back pain: a meta-analysis". CMAJ. 184 (11): E613–E624. doi:10.1503/cmaj.111271. PMC 3414626. PMID 22586331.
- Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C (December 2010). "An updated overview of clinical guidelines for the management of non-specific low back pain in primary care". European Spine Journal. 19 (12): 2075–2094. doi:10.1007/s00586-010-1502-y. PMC 2997201. PMID 20602122.
- "Low Back Pain Fact Sheet". National Institute of Neurological Disorders and Stroke. 3 November 2015. Archived from the original on 4 March 2016. Retrieved 5 March 2016.
- Manusov EG (September 2012). "Evaluation and diagnosis of low back pain". Primary Care. 39 (3): 471–479. doi:10.1016/j.pop.2012.06.003. PMID 22958556.
- Qaseem A, Wilt TJ, McLean RM, Forciea MA, Denberg TD, Barry MJ, et al. (April 2017). "Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians". Annals of Internal Medicine. 166 (7): 514–530. doi:10.7326/M16-2367. PMID 28192789.
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. (June 2012). "A systematic review of the global prevalence of low back pain". Arthritis and Rheumatism. 64 (6): 2028–2037. doi:10.1002/art.34347. PMID 22231424.
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. (December 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2163–2196. doi:10.1016/S0140-6736(12)61729-2. PMC 6350784. PMID 23245607.
- "Use of imaging studies for low back pain: percentage of members with a primary diagnosis of low back pain who did not have an imaging study (plain x-ray, MRI, CT scan) within 28 days of the diagnosis". 2013. Archived from the original on 4 October 2013. Retrieved 11 June 2013.
- Chou R, Fu R, Carrino JA, Deyo RA (February 2009). "Imaging strategies for low-back pain: systematic review and meta-analysis". Lancet. 373 (9662): 463–472. doi:10.1016/S0140-6736(09)60172-0. PMID 19200918. S2CID 31602395.
- Deyo RA, Mirza SK, Turner JA, Martin BI (2009). "Overtreating chronic back pain: time to back off?". Journal of the American Board of Family Medicine. 22 (1): 62–68. doi:10.3122/jabfm.2009.01.080102. PMC 2729142. PMID 19124635.
- Salzberg L (September 2012). "The physiology of low back pain". Primary Care. 39 (3): 487–498. doi:10.1016/j.pop.2012.06.014. PMID 22958558.
- Miller SM (September 2012). "Low back pain: pharmacologic management". Primary Care. 39 (3): 499–510. doi:10.1016/j.pop.2012.06.005. PMID 22958559.
- Manusov EG (September 2012). "Surgical treatment of low back pain". Primary Care. 39 (3): 525–531. doi:10.1016/j.pop.2012.06.010. PMID 22958562.
- Chou R, Baisden J, Carragee EJ, Resnick DK, Shaffer WO, Loeser JD (May 2009). "Surgery for low back pain: a review of the evidence for an American Pain Society Clinical Practice Guideline". Spine. 34 (10): 1094–1109. doi:10.1097/BRS.0b013e3181a105fc. PMID 19363455. S2CID 1504909.
- Henschke N, Ostelo RW, van Tulder MW, Vlaeyen JW, Morley S, Assendelft WJ, Main CJ (July 2010). "Behavioural treatment for chronic low-back pain". The Cochrane Database of Systematic Reviews (7): CD002014. doi:10.1002/14651858.CD002014.pub3. PMC 7065591. PMID 20614428.
- Marlowe D (September 2012). "Complementary and alternative medicine treatments for low back pain". Primary Care. 39 (3): 533–546. doi:10.1016/j.pop.2012.06.008. PMID 22958563.
- Walker BF, French SD, Grant W, Green S (February 2011). "A Cochrane review of combined chiropractic interventions for low-back pain". Spine. 36 (3): 230–242. doi:10.1097/BRS.0b013e318202ac73. PMID 21248591. S2CID 26310171.
- Dagenais S, Gay RE, Tricco AC, Freeman MD, Mayer JM (October 2010). "NASS Contemporary Concepts in Spine Care: spinal manipulation therapy for acute low back pain". The Spine Journal. 10 (10): 918–940. doi:10.1016/j.spinee.2010.07.389. PMID 20869008.
- Rubinstein SM, van Middelkoop M, Assendelft WJ, de Boer MR, van Tulder MW (February 2011). Rubinstein SM (ed.). "Spinal manipulative therapy for chronic low-back pain". The Cochrane Database of Systematic Reviews (2): CD008112. doi:10.1002/14651858.CD008112.pub2. hdl:1887/117578. PMID 21328304.
- Rubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW (September 2012). "Spinal manipulative therapy for acute low-back pain". The Cochrane Database of Systematic Reviews. 9 (9): CD008880. doi:10.1002/14651858.CD008880.pub2. hdl:1871/48563. PMC 6885055. PMID 22972127.
- Vinod Malhotra; Yao, Fun-Sun F.; Fontes, Manuel da Costa (2011). Yao and Artusio's Anesthesiology: Problem-Oriented Patient Management. Hagerstwon, MD: Lippincott Williams & Wilkins. pp. Chapter 49. ISBN 978-1-4511-0265-9. Archived from the original on 8 September 2017.
- Stanton TR, Latimer J, Maher CG, Hancock MJ (April 2010). "How do we define the condition 'recurrent low back pain'? A systematic review". European Spine Journal. 19 (4): 533–539. doi:10.1007/s00586-009-1214-3. PMC 2899839. PMID 19921522.
- Kelly GA, Blake C, Power CK, O'keeffe D, Fullen BM (February 2011). "The association between chronic low back pain and sleep: a systematic review". The Clinical Journal of Pain. 27 (2): 169–181. doi:10.1097/AJP.0b013e3181f3bdd5. PMID 20842008. S2CID 19569862.
- Borczuk P (July 2013). "An evidence-based approach to the evaluation and treatment of low back pain in the emergency department". Emergency Medicine Practice. 15 (7): 1–23, Quiz 23–24. PMID 24044786. Archived from the original on 14 August 2013.
- "Low Back Pain Fact Sheet". National Institute of Neurological Disorders and Stroke. National Institute of Health. Archived from the original on 19 July 2013. Retrieved 12 July 2013.
- Swain, Christopher T.V.; Pan, Fumin; Owen, Patrick J.; Schmidt, Hendrik; Belavy, Daniel L. (2020). "No consensus on causality of spine postures or physical exposure and low back pain: A systematic review of systematic reviews". Journal of Biomechanics. 102: 109312. doi:10.1016/j.jbiomech.2019.08.006.
- "Fast Facts About Back Pain". National Institute of Arthritis and Musculoskeletal and Skin Diseases. National Institute of Health. September 2009. Archived from the original on 5 June 2013. Retrieved 10 June 2013.
- "Low back pain – acute". U.S. Department of Health and Human Services – National Institutes of Health. Archived from the original on 1 April 2013. Retrieved 1 April 2013.
- Majchrzycki M, Mrozikiewicz PM, Kocur P, Bartkowiak-Wieczorek J, Hoffmann M, Stryła W, et al. (November 2010). "[Low back pain in pregnant women]". Ginekologia Polska (in Polish). 81 (11): 851–855. PMID 21365902.
- Lane DR, Takhar SS (August 2011). "Diagnosis and management of urinary tract infection and pyelonephritis". Emergency Medicine Clinics of North America. 29 (3): 539–552. doi:10.1016/j.emc.2011.04.001. PMID 21782073.
- Floyd, R., & Thompson, Clem. (2008). Manual of structural kinesiology. New York: McGraw-Hill Humanities/Social Sciences/Languages.
- Freeman MD, Woodham MA, Woodham AW (February 2010). "The role of the lumbar multifidus in chronic low back pain: a review". PM & R. 2 (2): 142–6, quiz 1 p following 167. doi:10.1016/j.pmrj.2009.11.006. PMID 20193941. S2CID 22246810.
- Hughes SP, Freemont AJ, Hukins DW, McGregor AH, Roberts S (October 2012). "The pathogenesis of degeneration of the intervertebral disc and emerging therapies in the management of back pain" (PDF). The Journal of Bone and Joint Surgery. British Volume. 94 (10): 1298–1304. doi:10.1302/0301-620X.94B10.28986. PMID 23015552. Archived from the original (PDF) on 4 October 2013. Retrieved 25 June 2013.
- Patel NB (2010). "Chapter 3: Physiology of Pain". In Kopf A, Patel NB (eds.). Guide to Pain Management in Low-Resource Settings. Archived from the original on 5 October 2013. Retrieved 26 May 2017.
- Cohen SP, Argoff CE, Carragee EJ (December 2008). "Management of low back pain". BMJ. 337: a2718. doi:10.1136/bmj.a2718. PMID 19103627. S2CID 78716905.
- Davis PC, Wippold II FJ, Cornelius RS, et al. (2011). American College of Radiology ACR Appropriateness Criteria – Low Back Pain (PDF) (Report). Archived from the original (PDF) on 22 December 2012.
- North American Spine Society (February 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, North American Spine Society, retrieved 25 March 2013, which cites
- Chou R, Qaseem A, Snow V, Casey D, Cross JT, Shekelle P, Owens DK, et al. (Clinical Efficacy Assessment Subcommittee of the American College of Physicians, American College of Physicians, American Pain Society Low Back Pain Guidelines Panel) (October 2007). "Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society". Annals of Internal Medicine. 147 (7): 478–491. doi:10.7326/0003-4819-147-7-200710020-00006. PMID 17909209.
- Forseen SE, Corey AS (October 2012). "Clinical decision support and acute low back pain: evidence-based order sets". Journal of the American College of Radiology. 9 (10): 704–712.e4. doi:10.1016/j.jacr.2012.02.014. PMID 23025864.
- Williams CM, Henschke N, Maher CG, van Tulder MW, Koes BW, Macaskill P, Irwig L (January 2013). "Red flags to screen for vertebral fracture in patients presenting with low-back pain". The Cochrane Database of Systematic Reviews. 1 (1): CD008643. doi:10.1002/14651858.CD008643.pub2. PMID 23440831. S2CID 42469808.
- Henschke N, Maher CG, Ostelo RW, de Vet HC, Macaskill P, Irwig L (February 2013). "Red flags to screen for malignancy in patients with low-back pain". The Cochrane Database of Systematic Reviews. 2 (2): CD008686. doi:10.1002/14651858.CD008686.pub2. PMID 23450586.
- Downie A, Williams CM, Henschke N, Hancock MJ, Ostelo RW, de Vet HC, et al. (December 2013). "Red flags to screen for malignancy and fracture in patients with low back pain: systematic review". BMJ. 347 (dec11 1): f7095. doi:10.1136/bmj.f7095. PMC 3898572. PMID 24335669.
- Williams CM, Henschke N, Maher CG, van Tulder MW, Koes BW, Macaskill P, Irwig L (January 2013). "Red flags to screen for vertebral fracture in patients presenting with low-back pain". The Cochrane Database of Systematic Reviews (1): CD008643. doi:10.1002/14651858.CD008643.pub2. PMID 23440831. S2CID 42469808.
- Manchikanti L, Glaser SE, Wolfer L, Derby R, Cohen SP (2009). "Systematic review of lumbar discography as a diagnostic test for chronic low back pain". Pain Physician. 12 (3): 541–559. doi:10.36076/ppj.2009/12/541. PMID 19461822.
- American Academy of Family Physicians, "Ten Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American Academy of Family Physicians, archived from the original on 10 February 2013, retrieved 5 September 2012
- American College of Physicians, "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American College of Physicians, archived from the original on 1 September 2013, retrieved 5 September 2013
- Crownover BK, Bepko JL (April 2013). "Appropriate and safe use of diagnostic imaging". American Family Physician. 87 (7): 494–501. PMID 23547591.
- Chou R, Qaseem A, Owens DK, Shekelle P, et al. (Clinical Guidelines Committee of the American College of Physicians) (February 2011). "Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians". Annals of Internal Medicine. 154 (3): 181–189. doi:10.7326/0003-4819-154-3-201102010-00008. PMID 21282698. S2CID 1326352.
- Flynn TW, Smith B, Chou R (November 2011). "Appropriate use of diagnostic imaging in low back pain: a reminder that unnecessary imaging may do as much harm as good". The Journal of Orthopaedic and Sports Physical Therapy. 41 (11): 838–846. doi:10.2519/jospt.2011.3618. PMID 21642763. S2CID 207399397.
- Steffens D, Maher CG, Pereira LS, Stevens ML, Oliveira VC, Chapple M, et al. (February 2016). "Prevention of Low Back Pain: A Systematic Review and Meta-analysis". JAMA Internal Medicine. 176 (2): 199–208. doi:10.1001/jamainternmed.2015.7431. PMID 26752509.
- Choi BK, Verbeek JH, Tam WW, Jiang JY (January 2010). Choi BK (ed.). "Exercises for prevention of recurrences of low-back pain". The Cochrane Database of Systematic Reviews (1): CD006555. doi:10.1002/14651858.CD006555.pub2. PMC 8078403. PMID 20091596.
- Chou R, Qaseem A, Snow V, Casey D, Cross JT, Shekelle P, Owens DK, et al. (Clinical Efficacy Assessment Subcommittee of the American College of Physicians, American College of Physicians, American Pain Society Low Back Pain Guidelines Panel) (October 2007). "Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society". Annals of Internal Medicine. 147 (7): 478–491. doi:10.7326/0003-4819-147-7-200710020-00006. PMID 17909209.
- Guild DG (September 2012). "Mechanical therapy for low back pain". Primary Care. 39 (3): 511–516. doi:10.1016/j.pop.2012.06.006. PMID 22958560.
- Hegmann KT, Travis R, Andersson GB, Belcourt RM, Carragee EJ, Donelson R, et al. (March 2020). "Non-Invasive and Minimally Invasive Management of Low Back Disorders". Journal of Occupational and Environmental Medicine. 62 (3): e111–e138. doi:10.1097/JOM.0000000000001812. PMID 31977923.
- Sahar T, Cohen MJ, Uval-Ne'eman V, Kandel L, Odebiyi DO, Lev I, et al. (April 2009). "Insoles for prevention and treatment of back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group". Spine. 34 (9): 924–933. doi:10.1097/BRS.0b013e31819f29be. PMID 19359999. S2CID 22162952.
- Sprouse R (September 2012). "Treatment: current treatment recommendations for acute and chronic undifferentiated low back pain". Primary Care. 39 (3): 481–486. doi:10.1016/j.pop.2012.06.004. PMID 22958557.
- Momsen AM, Rasmussen JO, Nielsen CV, Iversen MD, Lund H (November 2012). "Multidisciplinary team care in rehabilitation: an overview of reviews". Journal of Rehabilitation Medicine. 44 (11): 901–912. doi:10.2340/16501977-1040. PMID 23026978.
- Gomes-Neto M, Lopes JM, Conceição CS, Araujo A, Brasileiro A, Sousa C, et al. (January 2017). "Stabilization exercise compared to general exercises or manual therapy for the management of low back pain: A systematic review and meta-analysis". Physical Therapy in Sport. 23: 136–142. doi:10.1016/j.ptsp.2016.08.004. PMID 27707631.
- Hendrick P, Milosavljevic S, Hale L, Hurley DA, McDonough S, Ryan B, Baxter GD (March 2011). "The relationship between physical activity and low back pain outcomes: a systematic review of observational studies". European Spine Journal. 20 (3): 464–474. doi:10.1007/s00586-010-1616-2. PMC 3048226. PMID 21053026.
- Hendrick P, Te Wake AM, Tikkisetty AS, Wulff L, Yap C, Milosavljevic S (October 2010). "The effectiveness of walking as an intervention for low back pain: a systematic review". European Spine Journal. 19 (10): 1613–1620. doi:10.1007/s00586-010-1412-z. PMC 2989236. PMID 20414688.
- French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ (January 2006). "Superficial heat or cold for low back pain". The Cochrane Database of Systematic Reviews. 2011 (1): CD004750. doi:10.1002/14651858.CD004750.pub2. PMC 8846312. PMID 16437495.
- van Middelkoop M, Rubinstein SM, Kuijpers T, Verhagen AP, Ostelo R, Koes BW, van Tulder MW (January 2011). "A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain". European Spine Journal. 20 (1): 19–39. doi:10.1007/s00586-010-1518-3. PMC 3036018. PMID 20640863.
- Ebadi S, Henschke N, Forogh B, Nakhostin Ansari N, van Tulder MW, Babaei-Ghazani A, Fallah E (July 2020). "Therapeutic ultrasound for chronic low back pain". The Cochrane Database of Systematic Reviews. 2020 (7): CD009169. doi:10.1002/14651858.CD009169.pub3. PMC 7390505. PMID 32623724.
- National Institute for Health and Care Excellence (2016). Low back pain and sciatica in over 16s: assessment and management. Manchester: National Institute for Health and Care Excellence (NICE). ISBN 978-1-4731-2186-7. OCLC 1198756858.
- Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al. (2016). Noninvasive Treatments for Low Back Pain. AHRQ Comparative Effectiveness Reviews. Rockville (MD): Agency for Healthcare Research and Quality (US). PMID 26985522.
- van Duijvenbode IC, Jellema P, van Poppel MN, van Tulder MW (April 2008). "Lumbar supports for prevention and treatment of low back pain". The Cochrane Database of Systematic Reviews (2): CD001823. doi:10.1002/14651858.cd001823.pub3. PMC 7046130. PMID 18425875.
- Owen PJ, Miller CT, Mundell NL, Verswijveren SJ, Tagliaferri SD, Brisby H, et al. (November 2020). "Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis". British Journal of Sports Medicine. 54 (21): 1279–1287. doi:10.1136/bjsports-2019-100886. PMC 7588406. PMID 31666220.
- Hayden JA, Ellis J, Ogilvie R, Malmivaara A, van Tulder MW (September 2021). "Exercise therapy for chronic low back pain". The Cochrane Database of Systematic Reviews. 9 (10): CD009790. doi:10.1002/14651858.cd009790.pub2. PMC 8477273. PMID 34580864.
- Smith C, Grimmer-Somers K (June 2010). "The treatment effect of exercise programmes for chronic low back pain". Journal of Evaluation in Clinical Practice. 16 (3): 484–491. doi:10.1111/j.1365-2753.2009.01174.x. PMID 20438611.
- van Middelkoop M, Rubinstein SM, Verhagen AP, Ostelo RW, Koes BW, van Tulder MW (April 2010). "Exercise therapy for chronic nonspecific low-back pain". Best Practice & Research. Clinical Rheumatology. 24 (2): 193–204. doi:10.1016/j.berh.2010.01.002. PMID 20227641.
- Wewege MA, Booth J, Parmenter BJ (25 October 2018). "Aerobic vs. resistance exercise for chronic non-specific low back pain: A systematic review and meta-analysis". Journal of Back and Musculoskeletal Rehabilitation. 31 (5): 889–899. doi:10.3233/BMR-170920. PMID 29889056. S2CID 47013227.
- Woodman JP, Moore NR (January 2012). "Evidence for the effectiveness of Alexander Technique lessons in medical and health-related conditions: a systematic review". International Journal of Clinical Practice. 66 (1): 98–112. doi:10.1111/j.1742-1241.2011.02817.x. PMID 22171910. S2CID 7579458.
- Posadzki P, Ernst E (September 2011). "Yoga for low back pain: a systematic review of randomized clinical trials". Clinical Rheumatology. 30 (9): 1257–1262. doi:10.1007/s10067-011-1764-8. PMID 21590293. S2CID 17095187.
- Wieland LS, Skoetz N, Pilkington K, Vempati R, D'Adamo CR, Berman BM, et al. (Cochrane Back and Neck Group) (January 2017). "Yoga treatment for chronic non-specific low back pain". The Cochrane Database of Systematic Reviews. 1 (1): CD010671. doi:10.1002/14651858.CD010671.pub2. PMC 5294833. PMID 28076926.
- Saragiotto BT, Maher CG, Yamato TP, Costa LO, Menezes Costa LC, Ostelo RW, Macedo LG (January 2016). "Motor control exercise for chronic non-specific low-back pain". The Cochrane Database of Systematic Reviews. 2016 (1): CD012004. doi:10.1002/14651858.cd012004. PMC 8761501. PMID 26742533.
- Tagliaferri SD, Miller CT, Ford JJ, Hahne AJ, Main LC, Rantalainen T, et al. (June 2020). "Randomized Trial of General Strength and Conditioning Versus Motor Control and Manual Therapy for Chronic Low Back Pain on Physical and Self-Report Outcomes". Journal of Clinical Medicine. 9 (6): 1726. doi:10.3390/jcm9061726. PMC 7355598. PMID 32503243.
- Yamato TP, Maher CG, Saragiotto BT, Hancock MJ, Ostelo RW, Cabral CM, et al. (Cochrane Back and Neck Group) (July 2015). "Pilates for low back pain". The Cochrane Database of Systematic Reviews. 2015 (7): CD010265. doi:10.1002/14651858.CD010265.pub2. PMC 8078578. PMID 26133923.
- Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, van Tulder MW (September 2014). "Multidisciplinary biopsychosocial rehabilitation for chronic low back pain". The Cochrane Database of Systematic Reviews (9): CD000963. doi:10.1002/14651858.cd000963.pub3. PMID 25180773.
- Nizard J, Raoul S, Nguyen JP, Lefaucheur JP (October 2012). "Invasive stimulation therapies for the treatment of refractory pain". Discovery Medicine. 14 (77): 237–246. PMID 23114579.
- Dubinsky RM, Miyasaki J (January 2010). "Assessment: efficacy of transcutaneous electric nerve stimulation in the treatment of pain in neurologic disorders (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology". Neurology. 74 (2): 173–176. doi:10.1212/WNL.0b013e3181c918fc. PMID 20042705.
- "Acute low back pain without radiculopathy". English.prescrire.org. October 2019. Retrieved 15 November 2019.
- Machado GC, Maher CG, Ferreira PH, Day RO, Pinheiro MB, Ferreira ML (July 2017). "Non-steroidal anti-inflammatory drugs for spinal pain: a systematic review and meta-analysis". Annals of the Rheumatic Diseases. 76 (7): 1269–1278. doi:10.1136/annrheumdis-2016-210597. PMID 28153830. S2CID 22850331.
- Saragiotto BT, Machado GC, Ferreira ML, Pinheiro MB, Abdel Shaheed C, Maher CG (June 2016). "Paracetamol for low back pain". The Cochrane Database of Systematic Reviews. 2019 (6): CD012230. doi:10.1002/14651858.CD012230. PMC 6353046. PMID 27271789.
- Machado GC, Maher CG, Ferreira PH, Pinheiro MB, Lin CW, Day RO, et al. (March 2015). "Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials". BMJ. 350: h1225. doi:10.1136/bmj.h1225. PMC 4381278. PMID 25828856.
- Enthoven WT, Roelofs PD, Deyo RA, van Tulder MW, Koes BW (February 2016). "Non-steroidal anti-inflammatory drugs for chronic low back pain". The Cochrane Database of Systematic Reviews. 2 (8): CD012087. doi:10.1002/14651858.CD012087. PMC 7104791. PMID 26863524.
- Bhala N, Emberson J, Merhi A, Abramson S, Arber N, Baron JA, et al. (Coxib and traditional NSAID Trialists' (CNT) Collaboration)) (August 2013). "Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials". Lancet. 382 (9894): 769–779. doi:10.1016/S0140-6736(13)60900-9. PMC 3778977. PMID 23726390.
- Chaparro LE, Furlan AD, Deshpande A, Mailis-Gagnon A, Atlas S, Turk DC (April 2014). "Opioids compared with placebo or other treatments for chronic low back pain: an update of the Cochrane Review". Spine. 39 (7): 556–563. doi:10.1097/BRS.0000000000000249. PMID 24480962. S2CID 25356400.
- Abdel Shaheed C, Maher CG, Williams KA, Day R, McLachlan AJ (July 2016). "Efficacy, Tolerability, and Dose-Dependent Effects of Opioid Analgesics for Low Back Pain: A Systematic Review and Meta-analysis". JAMA Internal Medicine. 176 (7): 958–968. doi:10.1001/jamainternmed.2016.1251. PMID 27213267. S2CID 29903177.
- Shmagel A, Krebs E, Ensrud K, Foley R (September 2016). "Illicit Substance Use in US Adults With Chronic Low Back Pain". Spine. 41 (17): 1372–1377. doi:10.1097/brs.0000000000001702. PMC 5002230. PMID 27438382.
- Franklin GM (September 2014). "Opioids for chronic noncancer pain: a position paper of the American Academy of Neurology". Neurology. 83 (14): 1277–1284. doi:10.1212/WNL.0000000000000839. PMID 25267983.
- Dowell D, Haegerich TM, Chou R (March 2016). "CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016". MMWR. Recommendations and Reports. 65 (1): 1–49. doi:10.15585/mmwr.rr6501e1. PMID 26987082.
- de Leon-Casasola OA (March 2013). "Opioids for chronic pain: new evidence, new strategies, safe prescribing". The American Journal of Medicine. 126 (3 Suppl 1): S3-11. doi:10.1016/j.amjmed.2012.11.011. PMID 23414718.
- Enke O, New HA, New CH, Mathieson S, McLachlan AJ, Latimer J, et al. (July 2018). "Anticonvulsants in the treatment of low back pain and lumbar radicular pain: a systematic review and meta-analysis". CMAJ. 190 (26): E786–E793. doi:10.1503/cmaj.171333. PMC 6028270. PMID 29970367.
- Chou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, Baisden J, et al. (American Pain Society Low Back Pain Guideline Pane) (May 2009). "Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society". Spine. 34 (10): 1066–1077. doi:10.1097/BRS.0b013e3181a1390d. PMID 19363457. S2CID 10658374.
- Pinto RZ, Maher CG, Ferreira ML, Hancock M, Oliveira VC, McLachlan AJ, et al. (December 2012). "Epidural corticosteroid injections in the management of sciatica: a systematic review and meta-analysis". Annals of Internal Medicine. 157 (12): 865–877. doi:10.7326/0003-4819-157-12-201212180-00564. PMID 23362516. S2CID 21203011.
- "Epidural Corticosteroid Injection: Drug Safety Communication – Risk of Rare But Serious Neurologic Problems". FDA. 23 April 2014. Archived from the original on 24 April 2014. Retrieved 24 April 2014.
- Yousef AA, Al-deeb AE (March 2013). "A double-blinded randomised controlled study of the value of sequential intravenous and oral magnesium therapy in patients with chronic low back pain with a neuropathic component". Anaesthesia. 68 (3): 260–266. doi:10.1111/anae.12107. PMID 23384256. S2CID 5486834.
- Lee CS, Hwang CJ, Lee DH, Kim YT, Lee HS (March 2011). "Fusion rates of instrumented lumbar spinal arthrodesis according to surgical approach: a systematic review of randomized trials". Clinics in Orthopedic Surgery. 3 (1): 39–47. doi:10.4055/cios.2011.3.1.39. PMC 3042168. PMID 21369477.
- Rothberg S, Friedman BW (January 2017). "Complementary therapies in addition to medication for patients with nonchronic, nonradicular low back pain: a systematic review". The American Journal of Emergency Medicine. 35 (1): 55–61. doi:10.1016/j.ajem.2016.10.001. PMID 27751598. S2CID 34520820.
- Rubinstein SM, de Zoete A, van Middelkoop M, Assendelft WJ, de Boer MR, van Tulder MW (March 2019). "Benefits and harms of spinal manipulative therapy for the treatment of chronic low back pain: systematic review and meta-analysis of randomised controlled trials". BMJ. 364: l689. doi:10.1136/bmj.l689. PMC 6396088. PMID 30867144.
- Rubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW, et al. (Cochrane Back and Neck Group) (September 2012). "Spinal manipulative therapy for acute low-back pain". The Cochrane Database of Systematic Reviews (9): CD008880. doi:10.1002/14651858.CD008880.pub2. PMC 6885055. PMID 22972127.
- Dagenais S, Mayer J, Wooley JR, Haldeman S (2008). "Evidence-informed management of chronic low back pain with medicine-assisted manipulation". The Spine Journal. 8 (1): 142–149. doi:10.1016/j.spinee.2007.09.010. PMID 18164462.
- Macedo LG, Saragiotto BT, Yamato TP, Costa LO, Menezes Costa LC, Ostelo RW, Maher CG (February 2016). "Motor control exercise for acute non-specific low back pain". The Cochrane Database of Systematic Reviews. 2016 (2): CD012085. doi:10.1002/14651858.cd012085. PMC 8734597. PMID 26863390.
- Furlan AD, Yazdi F, Tsertsvadze A, Gross A, Van Tulder M, Santaguida L, et al. (2012). "A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain". Evidence-Based Complementary and Alternative Medicine. 2012: 953139. doi:10.1155/2012/953139. PMC 3236015. PMID 22203884.
- Lin CW, Haas M, Maher CG, Machado LA, van Tulder MW (July 2011). "Cost-effectiveness of guideline-endorsed treatments for low back pain: a systematic review". European Spine Journal. 20 (7): 1024–1038. doi:10.1007/s00586-010-1676-3. PMC 3176706. PMID 21229367.
- Furlan AD, Giraldo M, Baskwill A, Irvin E, Imamura M (September 2015). "Massage for low-back pain". The Cochrane Database of Systematic Reviews. 2015 (9): CD001929. doi:10.1002/14651858.CD001929.pub3. PMC 8734598. PMID 26329399.
- Gagnier JJ, Oltean H, van Tulder MW, Berman BM, Bombardier C, Robbins CB (January 2016). "Herbal Medicine for Low Back Pain: A Cochrane Review". Spine. 41 (2): 116–133. doi:10.1097/brs.0000000000001310. PMID 26630428.
- Cherkin DC, Herman PM (April 2018). "Cognitive and Mind-Body Therapies for Chronic Low Back Pain and Neck Pain: Effectiveness and Value". JAMA Internal Medicine. 178 (4): 556–557. doi:10.1001/jamainternmed.2018.0113. PMID 29507946. S2CID 3680364.
- Cramer H, Haller H, Lauche R, Dobos G (September 2012). "Mindfulness-based stress reduction for low back pain. A systematic review". BMC Complementary and Alternative Medicine. 12: 162. doi:10.1186/1472-6882-12-162. PMC 3520871. PMID 23009599.
- Anheyer D, Haller H, Barth J, Lauche R, Dobos G, Cramer H (June 2017). "Mindfulness-Based Stress Reduction for Treating Low Back Pain: A Systematic Review and Meta-analysis". Annals of Internal Medicine. 166 (11): 799–807. doi:10.7326/M16-1997. PMID 28437793. S2CID 1157568.
- Urrútia G, Burton AK, Morral A, Bonfill X, Zanoli G (19 April 2004). "Neuroreflexotherapy for non-specific low-back pain". The Cochrane Database of Systematic Reviews. 2011 (2): CD003009. doi:10.1002/14651858.cd003009.pub2. PMC 8992702. PMID 15106186.
- Urrútia G, Burton K, Morral A, Bonfill X, Zanoli G (March 2005). "Neuroreflexotherapy for nonspecific low back pain: a systematic review". Spine. 30 (6): E148–E153. doi:10.1097/01.brs.0000155575.85223.14. PMID 15770167. S2CID 31140257.
- Marin TJ, Van Eerd D, Irvin E, Couban R, Koes BW, Malmivaara A, et al. (June 2017). "Multidisciplinary biopsychosocial rehabilitation for subacute low back pain". The Cochrane Database of Systematic Reviews. 2017 (6): CD002193. doi:10.1002/14651858.cd002193.pub2. PMC 6481490. PMID 28656659.
- Maas ET, Ostelo RW, Niemisto L, Jousimaa J, Hurri H, Malmivaara A, van Tulder MW (October 2015). "Radiofrequency denervation for chronic low back pain". The Cochrane Database of Systematic Reviews. 2015 (10): CD008572. doi:10.1002/14651858.cd008572.pub2. PMC 8782593. PMID 26495910.
- Luz Júnior MA, Almeida MO, Santos RS, Civile VT, Costa LO (January 2019). "Effectiveness of Kinesio Taping in Patients With Chronic Nonspecific Low Back Pain: A Systematic Review With Meta-analysis". Spine. 44 (1): 68–78. doi:10.1097/BRS.0000000000002756. PMID 29952880. S2CID 49486200.
- Engers A, Jellema P, Wensing M, van der Windt DA, Grol R, van Tulder MW (January 2008). "Individual patient education for low back pain". The Cochrane Database of Systematic Reviews (1): CD004057. doi:10.1002/14651858.cd004057.pub3. hdl:2066/69744. PMC 6999124. PMID 18254037.
- Chou R, Shekelle P (April 2010). "Will this patient develop persistent disabling low back pain?". JAMA. 303 (13): 1295–1302. doi:10.1001/jama.2010.344. PMID 20371789.
- Hayden JA, Wilson MN, Riley RD, Iles R, Pincus T, Ogilvie R (November 2019). "Individual recovery expectations and prognosis of outcomes in non-specific low back pain: prognostic factor review". The Cochrane Database of Systematic Reviews. 2019 (11). doi:10.1002/14651858.cd011284.pub2. PMC 6877336. PMID 31765487.
- Cunningham F (2009). Williams Obstetrics (23 ed.). McGraw Hill Professional. p. 210. ISBN 9780071702850. Archived from the original on 8 September 2017.
- Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E (January 2010). "The association between smoking and low back pain: a meta-analysis". The American Journal of Medicine. 123 (1): 87.e7–87.35. doi:10.1016/j.amjmed.2009.05.028. PMID 20102998.
- Maharty DC (September 2012). "The history of lower back pain: a look "back" through the centuries". Primary Care. 39 (3): 463–470. doi:10.1016/j.pop.2012.06.002. PMID 22958555.
- Lutz GK, Butzlaff M, Schultz-Venrath U (August 2003). "Looking back on back pain: trial and error of diagnoses in the 20th century". Spine. 28 (16): 1899–1905. doi:10.1097/01.BRS.0000083365.41261.CF. PMID 12923482. S2CID 25083375.
- Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA (2009). "Comprehensive review of epidemiology, scope, and impact of spinal pain". Pain Physician. 12 (4): E35–E70. doi:10.36076/ppj.2009/12/E35. PMID 19668291.
- Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, et al. (April 2018). "The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors Among US States". JAMA. 319 (14): 1444–1472. doi:10.1001/jama.2018.0158. PMC 5933332. PMID 29634829.
- American College of Occupational and Environmental Medicine (February 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American College of Occupational and Environmental Medicine, archived from the original on 11 September 2014, retrieved 24 February 2014, which cites
- Talmage J, Belcourt R, Galper J, et al. (2011). "Low back disorders". In Hegmann KT (ed.). Occupational medicine practice guidelines : evaluation and management of common health problems and functional recovery in workers (3rd ed.). Elk Grove Village, IL: American College of Occupational and Environmental Medicine. pp. 336, 373, 376–77. ISBN 978-0615452272.
External links
- Back and spine at Curlie
- Back Pain at MedlinePlus.gov