Microcirculation
The microcirculation is the circulation of the blood in the smallest blood vessels, the microvessels of the microvasculature present within organ tissues.[1] The microvessels include terminal arterioles, metarterioles, capillaries, and venules. Arterioles carry oxygenated blood to the capillaries, and blood flows out of the capillaries through venules into veins.
| Microcirculation | |
|---|---|
 Microcirculation in the capillary | |
| Details | |
| System | Circulatory system |
| Artery | Arteriole |
| Vein | Venule |
| Identifiers | |
| MeSH | D008833 |
| Anatomical terminology | |
In addition to these blood vessels, the microcirculation also includes lymphatic capillaries and collecting ducts. The main functions of the microcirculation are the delivery of oxygen and nutrients and the removal of carbon dioxide (CO2). It also serves to regulate blood flow and tissue perfusion thereby affecting blood pressure and responses to inflammation which can include edema (swelling).
Most vessels of the microcirculation are lined by flattened cells of the endothelium and many of them are surrounded by contractile cells called pericytes. The endothelium provides a smooth surface for the flow of blood and regulates the movement of water and dissolved materials in the interstitial plasma between the blood and the tissues.
The microcirculation contrasts with macrocirculation, which is the circulation of blood to and from the organs.
Structure
Microvessels
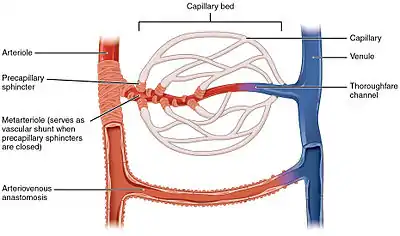

The vessels on the arterial side of the microcirculation are called the arterioles, which are well innervated, are surrounded by smooth muscle cells, and are 10-100 μm in diameter. Arterioles carry the blood to the capillaries, which are not innervated, have no smooth muscle, and are about 5-8 μm in diameter. Blood flows out of the capillaries into the venules, which have little smooth muscle and are 10-200 μm. The blood flows from the venules into the veins. Metarterioles connect arterioles and capillaries. A tributary to the venules is known as a thoroughfare channel.
The microcirculation has three major components: pre-capillary, capillary, and post-capillary. In the pre-capillary sector, arterioles, and precapillary sphincters participate. Their function is to regulate blood flow before it enters the capillaries and venules by the contraction and relaxation of the smooth muscle found on their walls. The second sector is the capillary sector, which is represented by the capillaries, where substance and gas exchange between blood and interstitial fluid takes place. Finally, the post-capillary sector is represented by the post-capillary venules, which are formed by a layer of endothelial cells that allow free movement of some substances.[2]
Microanatomy
Most vessels of the microcirculation are lined by flattened cells of the endothelium and many of them are surrounded by contractile cells called pericytes. The endothelium provides a smooth surface for the flow of blood and regulates the movement of water and dissolved materials in the interstitial plasma between the blood and the tissues. The endothelium also produces molecules that discourage the blood from clotting unless there is a leak. Pericyte cells can contract and decrease the size of the arterioles and thereby regulate blood flow and blood pressure.
Function
In addition to these blood vessels, the microcirculation also includes lymphatic capillaries and collecting ducts. The main functions of the microcirculation are the delivery of oxygen and nutrients and the removal of carbon dioxide (CO2). It also serves to regulate blood flow and tissue perfusion thereby affecting blood pressure and responses to inflammation which can include edema (swelling).
Regulation
The regulation of tissue perfusion occurs in microcirculation.[2] There, arterioles control the flow of blood to the capillaries. Arterioles contract and relax, varying their diameter and vascular tone, as the vascular smooth muscle responds to diverse stimuli. Distension of the vessels due to increased blood pressure is a fundamental stimulus for muscle contraction in arteriolar walls. As a consequence, microcirculation blood flow remains constant despite changes in systemic blood pressure. This mechanism is present in all tissues and organs of the human body. In addition, the nervous system participates in the regulation of microcirculation. The sympathetic nervous system activates the smaller arterioles, including terminals. Noradrenaline and adrenaline have effects on alpha and beta adrenergic receptors. Other hormones (catecholamine, renin-angiotensin, vasopressin, and atrial natriuretic peptide) circulate in the bloodstream and can have an effect on the microcirculation causing vasodilation or vasoconstriction. Many hormones and neuropeptides are released together with classical neurotransmitters.[1]
Arterioles respond to metabolic stimuli that are generated in the tissues. When tissue metabolism increases, catabolic products accumulate leading to vasodilation. The endothelium begins to control muscle tone and arteriolar blood flow tissue. Endothelial function in the circulation includes the activation and inactivation of circulating hormones and other plasma constituents. There are also synthesis and secretion of vasodilator and vasoconstrictor substances for modifying the width as necessary. Variations in the flow of blood that circulates by arterioles are capable of responses in endothelium.[1]
Capillary exchange
The term capillary exchange refers to all exchanges at microcirculatory level, most of which occurs in the capillaries. Sites where material exchange occurs between the blood and tissues are the capillaries, which branch out to increase the swap area, minimize the diffusion distance as well as maximize the surface area and the exchange time.[3]
Approximately, seven percent of the body's blood is in the capillaries which continuously exchange substances with the liquid outside these blood vessels, called interstitial fluid. This dynamic displacement of materials between the interstitial fluid and the blood is named capillary exchange.[4] These substances pass through capillaries through three different systems or mechanisms: diffusion, bulk flow, and transcytosis or vesicular transport.[2] The liquid and solid exchanges that take place in the microvasculature particularly involve capillaries and post-capillary venules and collecting venules.
Capillary walls allow the free flow of almost every substance in plasma.[5] The plasma proteins are the only exception, as they are too big to pass through.[4] The minimum number of un-absorbable plasma proteins that exit capillaries enter lymphatic circulation for returning later on to those blood vessels. Those proteins which leave capillaries use the first capillary exchange mechanism and the process of diffusion, which is caused by kinetic motion of molecules.[5]
Regulation
These exchanges of substances are regulated by different mechanisms.[6] These mechanisms work together and promote capillary exchange in the following way. First, molecules that diffuse are going to travel a short distance thanks to the capillary wall, the small diameter and the close proximity to each cell having a capillary. The short distance is important because the capillary diffusion rate decreases when the diffusion distance increases. Then, because of its large number (10-14 million capillaries), there is an incredible amount of surface area for exchange. However, this only has 5% of the total blood volume (250 ml 5000 ml). Finally, blood flows more slowly in the capillaries, given the extensive branching.[3]
Diffusion
Diffusion is the first and most important mechanism that allows the flow of small molecules across capillaries. The process depends on the difference of gradients between the interstitium and blood, with molecules moving to low concentrated spaces from high concentrated ones.[7] Glucose, amino acids, oxygen (O2) and other molecules exit capillaries by diffusion to reach the organism's tissues. Contrarily, carbon dioxide (CO2) and other wastes leave tissues and enter capillaries by the same process but in reverse.[4] Diffusion through the capillary walls depends on the permeability of the endothelial cells forming the capillary walls, which may be continuous, discontinuous, and fenestrated.[3] The Starling equation describes the roles of hydrostatic and osmotic pressures (the so-called Starling forces) in the movement of fluid across capillary endothelium. Lipids, which are transported by proteins, are too large to cross the capillary walls by diffusion, and have to rely on the other two methods.[8][9]
Bulk flow
The second mechanism of capillary exchange is bulk flow. It is used by small, lipid-insoluble substances in order to cross. This movement depends on the physical characteristics of the capillaries. For example, continuous capillaries (tight structure) reduce bulk flow, fenestrated capillaries (perforated structure) increases bulk flow, and discontinuous capillaries (great intercellular gaps) enable bulk flow. In this case, the exchange of materials is determined by changes in pressure.[6] When the flow of substances goes from the bloodstream or the capillary to the interstitial space or interstitium, the process is called filtration. This kind of movement is favored by blood hydrostatic pressure (BHP) and interstitial fluid osmotic pressure (IFOP).[4] When substances move from the interstitial fluid to the blood in capillaries, the process is called reabsorption. The pressures that favor this movement are blood colloid osmotic pressure (BCOP) and interstitial fluid hydrostatic pressure (IFHP).[10] Whether a substance is filtrated or reabsorbed depends on the net filtration pressure (NFP), which is the difference between hydrostatic (BHP and IFHP) and osmotic pressures (IFOP and BCOP).[4] These pressures are known as the Starling forces. If the NFP is positive then there will be filtration, but if it is negative then reabsorption will occur.[11]
Transcytosis
The third capillary exchange mechanism is transcytosis, also called vesicular transport.[12] By this process, blood substances move across the endothelial cells that compose the capillary structure. Finally, these materials exit by exocytosis, the process by which vesicles go out from a cell to the interstitial space. Few substances cross by transcytosis: it is mainly used by large, lipid-insoluble molecules such as the insulin hormone.[13] Once vesicles exit the capillaries, they go to the interstitium.[13] Vesicles can go directly to a specific tissue or they can merge with other vesicles, so their contents are mixed. This intermixed material increases the functional capability of the vesicle.[4]
See also
- Fahraeus–Lindquist effect
- Glycocalyx
- Microcirculatory Society
References
- Conti, Fiorenzo (13 April 2010). Fisiología Médica (1st ed.). Mc-Graw Hill. ISBN 978-970-10-7341-4.
- Drucker, René. Medical physiology (1st ed.). Modern Manual. p. 137.
- Sherwood, Lauralee (2005). Human Physiology. From cells to systems (7th ed.). Cengage learning. p. 361. ISBN 970-729-069-2.
- Tortora, Gerard (4 January 2011). Principles of anatomy and physiology (13th ed.). Wiley & Sons, Inc. p. 811. ISBN 978-0470565100.
- Hall, John (2011). Textbook of Medical Physiology (12th ed.). Elsevier Science Publishers. p. 184. ISBN 978-84-8086-819-8.
- Klaubunde, Richard (3 November 2011). Cardiovascular physiology concepts (2nd ed.). Lippincott Williams & Wilkins. p. 181. ISBN 9781451113846.
- Johnson, Leonard (2 October 2003). Essential medical physiology (3rd ed.). Academic Press. p. 59. ISBN 978-0123875846.
- Scow, R. O; Blanchette-Mackie, E. J; Smith, L. C (1980). "Transport of lipid across capillary endothelium". Federation Proceedings. 39 (9): 2610–7. PMID 6995154.
- "Fluid Physiology: 4.1 Microcirculation".
- Scallan, Joshua (2010). Capillary Fluid Exchange: Regulation, Functions and Pathology (3rd ed.). Morgan & Claypool Life Sciences. p. 4. ISBN 9781615040667.
- Sicar, Sabyasachi (2008). Principles of medical physiology (1st ed.). Lippincott Williams & Wilkins. p. 259. ISBN 978-3-13-144061-7.
- Barret, Kim (5 April 2012). Ganong Medical Physiology (24th ed.). Mc-Graw Hill. ISBN 978-0071780032.
- Shahid, Mohammad (January 2008). Physiology (1st ed.). Elsevier Health Sciences. p. 82. ISBN 978-0-7234-3388-0.