Oral ecology
Oral ecology is the microbial ecology of the microorganisms found in mouths. Oral ecology, like all forms of ecology, involves the study of the living things found in oral cavities as well as their interactions with each other and with their environment. Oral ecology is frequently investigated from the perspective of oral disease prevention, often focusing on conditions such as dental caries (or "cavities"), candidiasis ("thrush"), gingivitis, periodontal disease, and others. Interactions between microbes and their environment can result in the stabilization or destabilization of the oral microbiome, with destabilization believed to result in disease states. Destabilization of the microbiome can be influenced by several factors, including diet changes, drugs or immune system disorders.
History
Bacteria were first detected under the microscope of Dutch scientist Anton van Leeuwenhoek in the late 17th century from his own healthy human oral sample.[1] After using this technology on a healthy sample, Leeuwenhoek applied his tool to the decayed tooth matter of his wife, where he noted that the organisms present were highly similar to those found in cheese.[1] These are believed to likely have been lactic acid bacteria, however the link between bacterial acid production and tooth decay was not further uncovered until much later. After this discovery and the further development of microscopy, bacteria was found within tooth cavities by multiple scientists throughout the 19th century.[2][3][4][5][6][7] Willoughby Miller was the first recorded oral microbiologist, and he performed much of his foundational microbiology research in the laboratory of famed microbiologist Robert Koch. In this time, Miller generated the chemo-parasitic (also referred to as "acidogenic") theory of caries, which proposed that tooth decay is initiated by bacterial acid production on the surface of teeth.[8] This theory is considered to be foundational to the field of dentistry as well as oral ecology, by drawing connections between the activities of microbial entities and its effects on their non-living microscopic environment.[2][9]
In ecological terms, early work in oral microbiology largely falls into a category of microbial research now described as "reductionist", generally meaning it focused heavily on the isolation of individual microbes before observation or testing.[10] It wasn't until the late 20th century that "holistic" approaches to oral microbiology were coming into the mainstream, and thus microbial ecology was intentionally studied. Holistic microbiology considers not only an organism of interest but also the biological and abiotic context in which the organism naturally is found. Scientist Philip Marsh is credited with developing the ecological plaque hypothesis in 1994, in which he ideated that dental plaque can be both normal and healthy as well as "cariogenic" (creates cavities), depending on the microbial community (or "consortia") present in the biofilm and the community's stability.[11] Furthermore, in his theory, Marsh links the exposure of nonliving environmental influences on the microbial community to the selection and change in microbial constituents that can cause cariogenic conditions.
Ecology and types
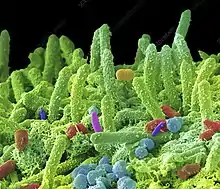
The human mouth contains around 500 to 1,000 different types of bacteria with various functions as part of the human flora and oral microbiology. About 100 to 200 species may live in them at any given time.[12] Individuals that practice oral hygiene have 1,000 to 100,000 bacteria living on each tooth surface, while less clean mouths can have between 100 million and 1 billion bacteria on each tooth.[13] While some of the bacteria in our mouths are harmful and can cause serious illness, much of our oral bacteria are actually beneficial in preventing disease. Streptococci make up a large part of oral bacteria.[14]
There are four main species within streptococci: the mutans, salivarius, anginosus, and mitis groups. Streptococcus mutans make up a large majority of what affects our mouths[15] and create acids which may cause decay.[16] The enzymes “leach down the tooth and begin to dissolve the ligaments and bone that help to hold the teeth in your mouth.”[17] By turning simple sugars and carbohydrates into acids and enzymes that dissolve tooth enamel, this bacteria can leave a person with lasting dental problems.[18] According to Dr. Robert Gandola, a dentist, “A number of bacteria can cause decay [and many] are suspected in periodontal (gum) disease.”[19]
Oral bacteria work with our immune system to keep our bodies disease free by fighting disease-producing germs that try to come in through the mouth. For example, some of these bacteria produce organic acids that kill the organisms that cause intestinal problems.[13] Without these good bacteria, our immune systems would be constantly bombarded by airborne and saliva-transferred germs. Bacteria are also needed to control the growth of fungus. “Balance between all the different bacteria and fungus are critical” or else the “fungus overgrows and takes over.”[19] So, ironically, though bacteria have the potential to harm us, our mouth and the good bacteria in it are the body's first line of defense. These bacteria are transmitted to a human early in their childhood through their contact with their caretakers by kisses or food premastication.[20]
Bacterial growth in the mouth/teeth
Numerous kinds of bacteria grow in the mouth. “They are competing for food and places to grow” and the many hard surfaces in the mouth provide an ideal place for bacteria and biofilms to grow and reproduce.[19] Unlike most other places in or on the body, the mouth does not desquamate (shed).[21] A tooth's distinct surface and stagnant nature makes it optimal for populations and growth of micro-organisms and bacteria, resulting in dental plaque. To grow and flourish in the mouth, biofilms go through four main stages of growth.[21] First, bacteria must be deposited from saliva onto a surface where it can attach. Then the bacteria, or micro-organisms, grow and replicate. Since bacteria can grow exponentially in short periods of time, it can quickly and easily create biofilms. Third, the biofilm matures and accumulates more mass on the surface. Bacteria can continue to divide and grow by binary fission until nutrients begin to run out or their growth is inhibited.[21] When this happens there is the final stage, the dispersal or detachment, causing the death of the bacteria.[22] Some oral bacteria, Streptococcus gordonii for example, cannot last for long periods without nutrients, while other types of bacteria can survive for weeks.[22] While in their prime, biofilms can cause major damage to a person's teeth and gums. Though damaging, biofilms can be partly removed by brushing and flossing and “some of it comes off with rinsing or eating.”[19]
Saliva
Saliva keeps the ecosystem of the mouth in balance. It contains its own bacterial enzymes that are beneficial to our health. An example of these are lysosomes. These antibacterial agents in saliva kill bacteria in our mouths and protect from potentially dangerous diseases.[23] In addition, saliva contains phosphate and calcium ions that help repair microscopic chinks made in the teeth by the bacteria's acid.[13] The major organic constituents of saliva are proteins and glycoproteins.[23] Proteins in saliva float around and influence the mouth's ecosystem in multiple ways. Some of the proteins provide nutrients for bacteria, while others cause bacteria to clump together so they are unable to stick to any surface and are washed away. The main function of saliva is to flush out all of the micro-organisms that could potentially threaten our health.[24] The flow of saliva constantly bathes the mouth and detaches all micro-organisms that are not already firmly attached to a surface.[13] This makes it difficult for bacteria to adhere to surfaces to even begin to form biofilms. Many harmful micro-organisms, therefore, are unable to attach quick enough to a surface before they are caught in saliva and swallowed.[25] Although saliva does a lot to keep our bodies healthy, it cannot completely keep all bacteria from adhering to tooth, tongue or gum surfaces.
Diseases
Diseases transmitted through saliva
Each day numerous bacteria grow in a person's mouth. Many diseases are related to oral bacteria. Proper oral care and habits often protect against and reduce the effects of some harmful bacteria.
Because of the amount of bacteria in each person's mouth, there is a transfer of bacteria through saliva when lip balm, drinks, toothbrushes, or anything else is shared. Said bacteria transfer can lead to human illnesses. Some of these diseases that result are relatively inconsequential while others could potentially have a serious impact on one's life. Some examples of the milder diseases passed through saliva include: herpes simple virus (cold sores or canker sores), flu virus, cold virus, various bacteria that cause periodontal disease (inflammation or infection of gum tissue), venereal diseases, and candida albicans (fungus).[26]
Mononucleosis (mono), known among teenagers as the “kissing disease”, is another prominent condition that can come from saliva exchange, although it is not caused by bacteria, it is a contagious viral disease in the herpes virus family. Mono can “be spread when a person coughs, sneezes, or shares objects such as drinking glass or water bottles.”[27] There are only certain stages when it is contagious, mostly during the fever stage,[27] but during those times it is transferable through saliva exchange.
Diseases related to oral hygiene
Some serious and possibly life-threatening diseases have been found to be connected to oral hygiene. These diseases are not passed through saliva, but are still influenced by the mouth's ecology and bacteria. Streptococcus mutans, a common oral bacteria discussed above, is a pathogen that causes pneumonia, sinusitis, otitis media, and meningitis.[18]
Prevention
Although disease is possible through oral interactions, there are many ways to prevent or reduce the risk of infection and disease. Brushing and flossing teeth regularly are the most basic ways to reduce these risks. These two hygiene tips help to get rid of bacteria that try to stick to surfaces in the mouth to form plaque (oral biofilms).[19] Brushing and flossing the teeth disrupts biofilms and their ability to permanently damage the teeth or gums. The less one brushes their teeth, the better chance that bacteria will form plaque, which may potentially cause serious oral health issues.[28]
Diet has an influence in our oral health as well.[29] Much of the bacteria in our mouths are nourished by simple sugars and carbohydrates.[19] An excess of candy, soda, or other simple sugars is an easy way to let bacteria thrive in our mouths. Fluoride is extremely effective in protecting enamel on the teeth. “Fluoride, a chemical that appears naturally in groundwater in many areas of the world, quickly bonds with the tooth's enamel to maintain its smooth crystalline surface and deter bacteria from gaining a toehold.”[13] The Oral-B website advises people to “drink tap water when possible” because “if bottled water is your main source of drinking water, you could be missing the decay-preventative benefits of fluoride.”[30] Also, a study in the Journal of the American Dental Association states that “antiseptic mouthwashes have been associated with a 28 to 34 percent reduction in dental plaque biofilms at six month follow-ups. Chlorhexidine gluconate [mouthwash] rinses, when combined with toothbrushing, have been reported to reduce oral biofilms . . . by 50 to 55 percent.”[31] Going to a dentist can help people who have difficulty with oral hygiene learn how to begin these preventive measure, as well as determining what symptoms one's oral ecology may be causing.
Notes
- van Leeuwenhoek, Antonie (1700). "A letter to the royal society". Philosophical Transactions of the Royal Society of London. 635 (265).
- He, Xue-song; Shi, Wen-yuan (June 2009). "Oral Microbiology: Past, Present and Future". International Journal of Oral Science. 1 (2): 47–58. doi:10.4248/ijos.09029. ISSN 2049-3169.
- Abbot, F (1879). "Caries of Human Teeth". Dental Cosmos. 21 (2).
- Black, G.V. (1884). "The Formation of Poisons by Microorganisms: A Biological Study of the Germ Theory of Disease".
{{cite journal}}: Cite journal requires|journal=(help) - Williams, J.L. (1897). "A contribution to the study of pathology of enamel". Dental Cosmos. 39 (3).
- Webb, M.H. (1883). "Notes on Operative Dentistry". The S. S. White Dental Manufacturing.
- Ruby, John D.; Cox, Charles F.; Akimoto, Naotake; Meada, Nobuko; Momoi, Yasuko (2010). "The Caries Phenomenon: A Timeline from Witchcraft and Superstition to Opinions of the 1500s to Today's Science". International Journal of Dentistry. 2010: 432767. doi:10.1155/2010/432767. ISSN 1687-8728. PMC 2913523. PMID 20706536.
- Miller, Willoughby D. (1890). "Micro-Organisms of the Human Mouth". The S. S. White Dental Manufacturing.
- Rossomando, EdwardF (2020). "The Influence of Miller's Chemo-Parasitic Theory on 20th Century Clinical Dentistry and Dental Research". Dental Hypotheses. 11 (2): 31. doi:10.4103/denthyp.denthyp_39_20. ISSN 2155-8213.
- Tecon, Robin; Mitri, Sara; Ciccarese, Davide; Or, Dani; van der Meer, Jan Roelof; Johnson, David R. (2019-02-26). "Bridging the Holistic-Reductionist Divide in Microbial Ecology". mSystems. 4 (1). doi:10.1128/msystems.00265-18. ISSN 2379-5077.
- Marsh, P.D. (July 1994). "Microbial Ecology of Dental Plaque and its Significance in Health and Disease". Advances in Dental Research. 8 (2): 263–271. doi:10.1177/08959374940080022001. ISSN 0895-9374.
- How Microbes Defend and Define Us
- Stevens, Jane E., and Jack Desrocher. "Oral ecology."
- "Streptococcus mutans." Encyclopædia Britannica.
- Marsh, Philip, and Michael V. Martin. Oral Microbiology. pg. 20
- Banas, Jeffrey A.; Drake, David R. (2018-07-31). "Are the mutans streptococci still considered relevant to understanding the microbial etiology of dental caries?". BMC Oral Health. 18 (1): 129. doi:10.1186/s12903-018-0595-2. ISSN 1472-6831. PMC 6069834. PMID 30064426.
- Dentist Robert Gandola, interview
- "Streptococcus mutans." Encyclopædia Britannica.
- Dentist Robert Gandola, email.
- Diane, Mapes (March 30, 2010), "Mom's kiss can spread cavities to baby", NBC News
- Kuramitsu, Howard K., and Richard P. Ellen. Oral Bacterial Ecology; the Molecular Basis.
- Thomas, John G. and Lindsay A. Nakaishi. “Managing the Complexity of a Dynamic Biofilm.”
- Kuramitsu, Howard K., and Richard P. Ellen. Oral Bacterial Ecology; the Molecular Basis
- Marsh, Philip, and Michael V. Martin. Oral Microbiology.
- DePaola, Dominick P., Frederick A. Curro, and Domenick T. Zero. "Saliva: The Precious Body Fluid."
- Robert Gandola, email.
- Dreher, Nancy. "What you need to know about mono."
- Favot, Christa. “What is Living in my Mouth? Biofilms, Carbohydrate, and Acid Blasts.”
- “Avoiding Tooth Decay.” Oral-B.
- “Avoiding Tooth Decay.” Oral-B.
- Slavkin, HC. "Biofilms, Microbial Ecology and Antoni Van Leeuwenhoek."
References
- "Antony van Leeuwenhoek." University of California Museum of Paleontology. 10 October 2008
- "Avoiding Tooth Decay." Oral-B. 10 October 2008 .
- DePaola, Dominick P., Frederick A. Curro, and Domenick T. Zero. "Saliva: The Precious Body Fluid." J Am Dent Assoc 139.suppl_2 (2008): 5S-10. 10 Oct 2008.
- Dreher, Nancy. "What you need to know about mono." Current Health 2 23.7 (March 1997): 28. Academic Search Premier. EBSCO. Brigham Young University, Provo, UT. 10 October 2008.
- Favot, Christa. "What is Living in my Mouth? Biofilms, Carbohydrate, and Acid Blasts." The Naked Scientists (March 2006). 10 October 2008.
- Gandola, Dr. Robert. Dentist. Email correspondence. 15 October 2008.
- Marsh, Philip, and Michael V. Martin. Oral Microbiology. Oxford: Wright/Butterworth-Heinem, 1999.
- Slavkin, HC. "Biofilms, Microbial Ecology and Antoni Van Leeuwenhoek." J Am Dent Assoc 128.4 (1997). 18 September 2008.
- Stevens, Jane E., and Jack Desrocher. "Oral ecology." Technology Review (00401692) 100.1 (January 1997): 48. Academic Search Premier. EBSCO. Brigham Young University, Provo, UT. 10 October 2008.
- "Streptococcus mutans." Encyclopædia Britannica. 2008. Encyclopædia Britannica Online. 18 September 2008.
- Thomas, John G., and Lindsay A. Nakaishi. "Managing the Complexity of a Dynamic Biofilm." J Am Dent Assoc 137.3 (2006). 10 October 2008.
- "Toothbrush Care, Cleaning and Replacement." J Am Dent Assoc 137.3 (2006): 415. 10 October 2008
- Zimmer, Carl. "How Microbes Defend and Define Us." Science, New York Times. 12 Jul 2010.