Prostatitis
Prostatitis is inflammation of the prostate gland. Prostatitis is classified into acute, chronic, asymptomatic inflammatory prostatitis, and chronic pelvic pain syndrome.
| Prostatitis | |
|---|---|
| Other names | Prostatosis |
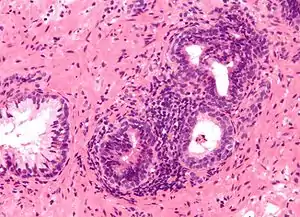 | |
| Micrograph showing an inflamed prostate gland, the histologic correlate of prostatitis. A normal non-inflamed prostatic gland is seen on the left of the image. H&E stain. | |
| Specialty | Urology |
In the United States, prostatitis is diagnosed in 8% of all male urologist visits and 1% of all primary care physician visits for male genitourinary symptoms.[1]
Classification
The term prostatitis refers to inflammation of the tissue of the prostate gland. It may occur as an appropriate physiological response to an infection, or it may occur in the absence of infection.[2]
In 1999, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) devised a new classification system.[3][4] For more specifics about each type of prostatitis, including information on symptoms, treatment, and prognosis, follow the links to the relevant full articles.
| Category | Current name | Old name | Pain | Bacteria | WBCs | Description |
|---|---|---|---|---|---|---|
| I | Acute prostatitis | Acute bacterial prostatitis | Yes | Yes | Yes | Bacterial infection of the prostate gland that requires urgent medical treatment. |
| II | Chronic bacterial prostatitis | Chronic bacterial prostatitis | ± | Yes | Yes | A relatively rare condition that usually presents as intermittent urinary tract infections. |
| IIIa | Inflammatory CP/CPPS | Nonbacterial prostatitis | Yes | No | Yes | Accounts for 90–95% of prostatitis diagnoses,[5] formerly known as chronic nonbacterial prostatitis'. |
| IIIb | Noninflammatory CP/CPPS | Prostatodynia | Yes | No | No | |
| IV | Asymptomatic inflammatory prostatitis | (none) | No | No | Yes | No history of genitourinary pain complaints, but leukocytosis is noted, usually during evaluation for other conditions. Between 6 and 19% of men have pus cells in their semen but no symptoms.[6] |
In 1968, Meares and Stamey determined a classification technique based upon the culturing of bacteria.[7] This classification is no longer used.
The conditions are distinguished by the different presentation of pain, white blood cells (WBCs) in the urine, duration of symptoms and bacteria cultured from the urine. To help express prostatic secretions that may contain WBCs and bacteria, prostate massage is sometimes used.[8]
See also
- Interstitial cystitis — a related disease
- Granulomatous prostatitis
- IgG4-related prostatitis
- Male accessory gland infection (MAGI)
References
- Collins MM, Stafford RS, O'Leary MP, Barry MJ (1998). "How common is prostatitis? A national survey of physician visits". J. Urol. 159 (4): 1224–8. doi:10.1016/S0022-5347(01)63564-X. PMID 9507840.
- Kirby, Roger; Carson, Culley C. (January–February 2015). "Editor's Comment on Diagnosis and treatment of chronic prostatitis/chronic pelvic pain syndrome". Trends in Urology and Men's Health. 6 (1): 17. doi:10.1002/tre.434.
- Krieger JN, Nyberg L, Nickel JC (July 1999). "NIH consensus definition and classification of prostatitis". JAMA. 282 (3): 236–7. doi:10.1001/jama.282.3.236. PMID 10422990.
- J. Curtis Nickel (1999). Textbook of prostatitis. Taylor & Francis. pp. 27–. ISBN 978-1-901865-04-2. Retrieved 18 April 2010.
- Habermacher GM, Chason JT, Schaeffer AJ (2006). "Prostatitis/chronic pelvic pain syndrome". Annu. Rev. Med. 57: 195–206. doi:10.1146/annurev.med.57.011205.135654. PMID 16409145.
- Korrovits P, Ausmees K, Mändar R, Punab M (June 2008). "Prevalence of asymptomatic inflammatory (National Institutes of Health Category IV) prostatitis in young men according to semen analysis". Urology. 71 (6): 1010–5. doi:10.1016/j.urology.2007.12.082. PMID 18455767.
- Meares EM, Stamey TA (March 1968). "Bacteriologic localization patterns in bacterial prostatitis and urethritis". Invest Urol. 5 (5): 492–518. PMID 4870505.
- "Prostatitis: Benign Prostate Disease: Merck Manual Professional". Retrieved 2011-07-11.