Pleural empyema
Pleural empyema is a collection of pus in the pleural cavity caused by microorganisms, usually bacteria.[1] Often it happens in the context of a pneumonia, injury, or chest surgery.[1] It is one of the various kinds of pleural effusion. There are three stages: exudative, when there is an increase in pleural fluid with or without the presence of pus; fibrinopurulent, when fibrous septa form localized pus pockets; and the final organizing stage, when there is scarring of the pleura membranes with possible inability of the lung to expand. Simple pleural effusions occur in up to 40% of bacterial pneumonias. They are usually small and resolve with appropriate antibiotic therapy. If however an empyema develops additional intervention is required.
| Pleural empyema | |
|---|---|
| Other names | Pyothorax, purulent pleuritis, lung empyema |
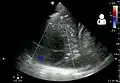
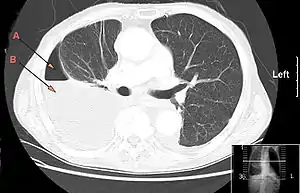 | |
| CT chest showing large right sided hydro-pneumothorax from pleural empyema. Arrows A: air, B: fluid | |
| Specialty | Pulmonology, cardiothoracic surgery |
| Symptoms | Fever, chest pain with breathing in, cough, shortness of breath |
| Causes | Bacteria (often Strep. pneumonia) |
| Diagnostic method | Chest X-ray, Ultrasound, CT scan, thoracentesis |
| Differential diagnosis | Pneumonia, pleural effusion, pulmonary embolism |
| Treatment | Supportive care, antibiotics, surgery, chest tube |
Signs and symptoms
The clinical presentation of both the adult and pediatric patient with pleural empyema depends upon several factors, including the causative micro-organism. Most cases present themselves in the setting of a pneumonia, although up to one third of patients do not have clinical signs of pneumonia and as many as 25% of cases are associated with trauma (including surgery).[2] Symptoms include fever, dry cough, sweating, difficulty breathing, and unintentional weight loss.[3] The elderly often do not have classic symptoms, but instead have anemia and exhaustion.[4]
Mechanism
When there is inflammation at the pleural space, fluid is produced at a greater level. As the disease progresses, bacteria can arrive at the fluid, which created an empyema.[5]
Diagnosis
The initial investigations for suspected empyema remains chest X-ray, although it cannot differentiate an empyema from uninfected parapneumonic effusion.[6] Ultrasound must be used to confirm the presence of a pleural fluid collection and can be used to estimate the size of the effusion, differentiate between free and loculated pleural fluid and guide thoracocentesis if necessary. Chest CT and MRI do not provide additional information in most cases and should therefore not be performed routinely.[7] On a CT scan, empyema fluid most often has a radiodensity of about 0-20 Hounsfield units (HU),[8] but gets over 30 HU when becoming more thickened with time.[9]
The most often used "golden" criteria for empyema are pleural effusion with macroscopic presence of pus, a positive Gram stain or culture of pleural fluid, or a pleural fluid pH under 7.2 with normal peripheral blood pH.[10][11] Clinical guidelines for adult patients therefore advocate diagnostic pleural fluid aspiration in patients with pleural effusion in association with sepsis or pneumonic illness.[12] Because pleural effusion in the pediatric population is almost always parapneumonic and the need for chest tube drainage can be made on clinical grounds, British guidelines for the management of pleural infection in children do not recommend diagnostic pleural fluid sampling.[7]
Blood and sputum culture has often already been performed in the setting of community acquired pneumonia needing hospitalization. It should however be noted that the micro-organism responsible for development of empyema is not necessarily the same as the organism causing the pneumonia, especially in adults. As already mentioned before, sensitivity of pleural fluid culture is generally low, often partly due to prior administration of antibiotics. It has been shown that culture yield can be increased from 44% to 69% if pleural fluid is injected into blood culture bottles (aerobic and anaerobic) immediately after aspiration.[11] Furthermore, diagnostic rates can be improved for specific pathogens using polymerase chain reaction or antigen detection, especially for Streptococcus pneumoniae, Streptococcus pyogenes and Staphylococcus aureus. In a study including 78 children with pleural empyema, the causative micro-organism could be identified using direct culture of fresh pleural fluid in 45% of patients, with an additional 28% using PCR on pleural fluid of negative cultures. Pneumococcal antigen detection in pleural fluid samples by latex agglutination can also be useful for rapid diagnosis of pneumococcal empyema. In the previously noted study, positive and negative predictive value of pneumococcal antigen detection was 95% and 90%, respectively.[13]
Treatment
Pleural fluid drainage
Proven empyema (as defined by the "golden" criteria mentioned earlier) is an indication for prompt chest tube drainage.[12] This has been shown to improve resolution of the infection and shorten hospital admission.[15] Data from a meta-analysis has shown that a pleural fluid pH of <7.2 is the most powerful indicator to predict the need for chest tube drainage in patients with non-purulent, culture negative fluid.[16]
Because of the viscous, lumpy nature of infected pleural fluid, in combination with possible septation and loculation, it has been proposed that intrapleural fibrinolytic or mucolytic therapy might improve drainage and therefore might have a positive effect on the clinical outcome.[17] Intrapleural fibrinolysis with urokinase decreased the need for surgery but there is a trend to increased serious side effects.[18]
Approximately 15 to 40 percent of people require surgical drainage of the infected pleural space because of inadequate drainage due to clogging of the chest tube or loculated empyema.[19] Patients should thus be considered for surgery if they have ongoing signs of sepsis in association with a persistent pleural collection despite drainage and antibiotics.[12]
Antibiotics
There is no readily available evidence on the route of administration and duration of antibiotics in patients with pleural empyema. Experts agree that all patients should be hospitalized and treated with antibiotics intravenously.[7][12] The specific antimicrobial agent should be chosen based on Gram stain and culture, or on local epidemiologic data when these are not available. Anaerobic coverage must be included in all adults, and in children if aspiration is likely. Good pleural fluid and empyema penetration has been reported in adults for penicillins, ceftriaxone, metronidazole, clindamycin, vancomycin, gentamicin and ciprofloxacin.[20][21] Aminoglycosides should typically be avoided as they have poor penetration into the pleural space. There is no clear consensus on duration of intravenous and oral therapy. Switching to oral antibiotics can be considered upon clinical and objective improvement (adequate drainage and removal of chest tube, declining CRP, temperature normalization). Oral antibiotic treatment should then be continued for another 1–4 weeks, again based on clinical, biochemical and radiological response.[7][12]
Prognosis
All patients with empyema require outpatient follow-up with a repeat chest X-ray and inflammatory biochemistry analysis within 4 weeks following discharge. Chest radiograph returns to normal in the majority of patients by 6 months. Patients should, of course, be advised to return sooner if symptoms redevelop. Long-term sequelae of pleural empyema are rare but include bronchopleural fistula formation, recurrent empyema and pleural thickening, which may lead to functional lung impairment needing surgical decortication.[12]
Mortality in children is generally reported to be less than 3%.[7] No reliable clinical, radiological or pleural fluid characteristics accurately determine patients’ prognosis at initial presentation.[22]
Epidemiology
The incidence of pleural empyema and the prevalence of specific causative microorganisms varies depending on the source of infection (community acquired vs. hospital acquired pneumonia), the age of the patient and host immune status. Risk factors include alcoholism, drug use, HIV infection, neoplasm and pre-existent pulmonary disease.[23] Pleural empyema was found in 0.7% of 3675 patients needing hospitalization for a community acquired pneumonia in a recent Canadian single-center prospective study.[10] A multi-center study from the UK including 430 adult patients with community acquired pleural empyema found negative pleural-fluid cultures in 54% of patients, Streptococcus milleri group in 16%, Staphylococcus aureus in 12%, Streptococcus pneumoniae in 8%, other Streptococci in 7% and anaerobic bacteria in 8%.[17]
The risk of empyema in children seems to be comparable to adults. Using the United States Kids’ Inpatient Database the incidence is calculated to be around 1.5% in children hospitalized for community acquired pneumonia,[24] although percentages up to 30% have been reported in individual hospitals,[25] a difference which may be explained by an transient endemic of highly invasive serotype or overdiagnosis of small parapneumonic effusions. The distribution of causative organisms does differ greatly from that in adults: in an analysis of 78 children with community acquired pleural empyema, no micro-organism was found in 27% of patients, Streptococcus pneumoniae in 51%, Streptococcus pyogenes in 9% and Staphylococcus aureus in 8%.[13]
Although pneumococcal vaccination dramatically decreased the incidence of pneumonia in children, it did not have this effect on the incidence of complicated pneumonia. It has been shown that the incidence of empyema in children was already on the rise at the end of the 20th century, and that the widespread use of pneumococcal vaccination did not slow down this trend.[26] This might in part be explained by a change in prevalence of (more invasive) pneumococcal serotypes, some of which are not covered by the vaccine, as well a rise in incidence of pneumonia caused by other streptococci and staphylococci.[27]
References
- Redden MD, Chin TY, van Driel ML (March 2017). "Surgical versus non-surgical management for pleural empyema". Cochrane Database Syst Rev. 3: CD010651. doi:10.1002/14651858.CD010651.pub2. ISSN 1469-493X. PMC 6464687. PMID 28304084.
- Fernández-Cotarelo MJ, López-Medrano F, San Juan R, Díaz-Pedroche C, Lizasoain M, Chaves F, Aguado JM (March 2007). "Protean manifestations of pleural empyema caused by Streptococcus pneumoniae in adults". Eur. J. Intern. Med. 18 (2): 141–5. doi:10.1016/j.ejim.2006.09.017. PMID 17338967.
- "Empyema: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2021-06-19.
- Feller-Kopman, David; Light, Richard (2018-02-21). "Pleural Disease". New England Journal of Medicine. doi:10.1056/NEJMra1403503.
- Garvia, Veronica; Paul, Manju (2021), "Empyema", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 29083780, retrieved 2021-06-19
- King S, Thomson A (2002). "Radiological perspectives in empyema". British Medical Bulletin. 61: 203–14. doi:10.1093/bmb/61.1.203. PMID 11997307.
- Balfour-Lynn IM, Abrahamson E, Cohen G, Hartley J, King S, Parikh D, Spencer D, Thomson AH, Urquhart D (2005). "BTS guidelines for the management of pleural infection in children". Thorax. 60 (Suppl 1): 1–21. doi:10.1136/thx.2004.030676. PMC 1766040. PMID 15681514.
- Yildiz S, Cece H, Turksoy O (October 2010). "Discriminative role of CT in exudative and transudative pleural effusions". AJR Am J Roentgenol. 195 (4): W305, author reply W306. doi:10.2214/AJR.10.4437. ISSN 0361-803X. PMID 20858794.
- Moshe Schein, John C. Marshall (2013). Source Control: A Guide to the Management of Surgical Infections. Springer Science & Business Media. ISBN 9783642559143.
- Ahmed R, Marri T, Huang J (2006). "Thoracic empyema in patients with community-acquired pneumonia". American Journal of Medicine. 119 (10): 877–83. doi:10.1016/j.amjmed.2006.03.042. PMID 17000220.
- Ferrer A, Osset J, Alegre J, Suriñach JM, Crespo E, Fernández de Sevilla T, Fernández F (April 1999). "Prospective clinical and microbiological study of pleural effusions". Eur. J. Clin. Microbiol. Infect. Dis. 18 (4): 237–41. doi:10.1007/s100960050270. PMID 10385010.
- Davies H, Davies R, Davies C (2010). "Management of pleural infection in adults: British Thoracic Society Pleural Disease Guideline 2010". Thorax. 65 (Suppl 2): 41–53. doi:10.1136/thx.2010.137000. PMID 20696693.
- Le Monnier A, Carbonnelle E, Zahar JR, Le Bourgeois M, Abachin E, Quesne G, Varon E, Descamps P, De Blic J, Scheinmann P, Berche P, Ferroni A (2006). "Microbiological diagnosis of empyema in children: comparative evaluations by culture, polymerase chain reaction, and pneumococcal antigen detection in pleural fluids". Clinical Infectious Diseases. 42 (8): 1135–40. doi:10.1086/502680. PMID 16575731.
- "UOTW #28 - Ultrasound of the Week". Ultrasound of the Week. 3 December 2014. Retrieved 27 May 2017.
- Sasse S, Nguyen TK, Mulligan M, Wang NS, Mahutte CK, Light RW (June 1997). "The effects of early chest tube placement on empyema resolution". Chest. 111 (6): 1679–83. doi:10.1378/chest.111.6.1679. PMID 9187193.
- Heffner JE, Brown LK, Barbieri C, DeLeo JM (June 1995). "Pleural fluid chemical analysis in parapneumonic effusions. A meta-analysis". Am. J. Respir. Crit. Care Med. 151 (6): 1700–8. doi:10.1164/ajrccm.151.6.7767510. PMID 7767510.
- Maskell NA, Davies CW, Nunn AJ, Hedley EL, Gleeson FV, Miller R, Gabe R, Rees GL, Peto TE, Woodhead MA, Lane DJ, Darbyshire JH, Davies RJ (2005). "U.K. controlled trial of intrapleural streptokinase for pleural infection". New England Journal of Medicine. 352 (9): 865–74. doi:10.1056/nejmoa042473. PMID 15745977.
- Nie W, Liu Y, Ye J, Shi L, Shao F, Ying K, Zhang R (July 2014). "Efficacy of intrapleural instillation of fibrinolytics for treating pleural empyema and parapneumonic effusion: a meta-analysis of randomized control trials". The Clinical Respiratory Journal. 8 (3): 281–91. doi:10.1111/crj.12068. PMID 24428897.
- Ferguson AD, Prescott RJ, Selkon JB, Watson D, Swinburn CR (April 1996). "The clinical course and management of thoracic empyema". QJM. 89 (4): 285–9. doi:10.1093/qjmed/89.4.285. PMID 8733515.
- Teixeira LR, Sasse SA, Villarino MA, Nguyen T, Mulligan ME, Light RW (June 2000). "Antibiotic levels in empyemic pleural fluid". Chest. 117 (6): 1734–9. doi:10.1378/chest.117.6.1734. PMID 10858410.
- Umut S, Demir T, Akkan G, Keskiner N, Yilmaz V, Yildirim N, Sipahioğlu B, Hasan A, Barlas A, Sözer K (April 1993). "Penetration of ciprofloxacin into pleural fluid". J Chemother. 5 (2): 110–2. doi:10.1080/1120009X.1993.11739217. PMID 8515292.
- Davies CW, Kearney SE, Gleeson FV, Davies RJ (November 1999). "Predictors of outcome and long-term survival in patients with pleural infection". Am. J. Respir. Crit. Care Med. 160 (5 Pt 1): 1682–7. doi:10.1164/ajrccm.160.5.9903002. PMID 10556140.
- Alfageme I, Muñoz F, Peña N, Umbría S (March 1993). "Empyema of the thorax in adults. Etiology, microbiologic findings, and management". Chest. 103 (3): 839–43. doi:10.1378/chest.103.3.839. PMID 8449078.
- Li S, Tancredi D (2010). "Empyema hospitalizations increased in US children despite pneumococcal conjugate vaccine". Pediatrics. 125 (1): 26–33. doi:10.1542/peds.2009-0184. PMID 19948570.
- Byington CL, Spencer LY, Johnson TA, Pavia AT, Allen D, Mason EO, Kaplan S, Carroll KC, Daly JA, Christenson JC, Samore MH (2002). "An epidemiological investigation of a sustained high rate of pediatric parapneumonic empyema: risk factors and microbiological associations". Clinical Infectious Diseases. 34 (4): 434–40. doi:10.1086/338460. PMID 11797168.
- Grijalva CG, Nuorti JP, Zhu Y, Griffin MR (2010). "Increasing incidence of empyema complicating childhood community-acquired pneumonia in the United States". Clinical Infectious Diseases. 50 (6): 805–13. doi:10.1086/650573. PMC 4696869. PMID 20166818.
- Obando I, Camacho-Lovillo MS, Porras A, Gandía-González MA, Molinos A, Vazquez-Barba I, Morillo-Gutierrez B, Neth OW, Tarrago D (August 2012). "Sustained high prevalence of pneumococcal serotype 1 in paediatric parapneumonic empyema in southern Spain from 2005 to 2009". Clin. Microbiol. Infect. 18 (8): 763–8. doi:10.1111/j.1469-0691.2011.03632.x. PMID 21910779.