Pneumoconiosis
Pneumoconiosis is the general term for a class of interstitial lung disease where inhalation of dust ( for example Ash dust, lead particles, pollen grains etc) has caused interstitial fibrosis.[1][2] The three most common types are asbestosis, silicosis, and coal miner's lung.[3] Pneumoconiosis often causes restrictive impairment,[4] although diagnosable pneumoconiosis can occur without measurable impairment of lung function.[1][2] Depending on extent and severity, it may cause death within months or years, or it may never produce symptoms. It is usually an occupational lung disease, typically from years of dust exposure during work in mining;[5] textile milling; shipbuilding, ship repairing, and/or shipbreaking; sandblasting; industrial tasks; rock drilling (subways or building pilings);[6] or agriculture.[7][8] It is one of the most common occupational diseases in the world.[9]
| Pneumoconiosis | |
|---|---|
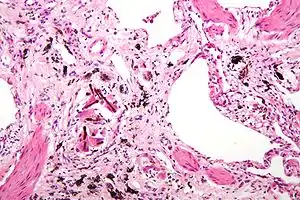 | |
| Micrograph of asbestosis (with ferruginous bodies), a type of pneumoconiosis. H&E stain. | |
| Specialty | Pulmonology |
Types
Depending upon the type of dust, the disease is given different names:
- Coalworker's pneumoconiosis (also known as coal miner's lung, black lung or anthracosis) – coal, carbon
- Aluminosis – Aluminium
- Asbestosis – asbestos
- Silicosis (also known as "grinder's disease" or Potter's rot) – crystalline silica dust
- Bauxite fibrosis – bauxite
- Berylliosis – beryllium
- Siderosis – iron
- Byssinosis – Byssinosis is caused by cotton dust inhalation and typically demonstrates a different pattern of lung abnormalities than most other pneumoconiosis.[1]
- Chalicosis – fine dust from stonecutting
- Silicosiderosis (also sometimes called iron miner's lung[10]) – mixed dust containing silica and iron[11]
- Labrador lung (found in miners in Labrador, Canada) – mixed dust containing iron, silica and anthophyllite, a type of asbestos
- Stannosis – tin oxide
- Talcosis – talc
- Baritosis - a benign type of pneumoconiosis caused by barium inhalation; it typically causes little or no overgrowth, hardening, and/or fibrosis.[12]
- Mixed-dust pneumoconiosis[1]
Pathogenesis
The reaction of the lung to mineral dusts depends on many variables, including size, shape, solubility, and reactivity of the particles.[13] For example, particles greater than 5 to 10 μm are unlikely to reach distal airways, whereas particles smaller than 0.5 μm move into and out of alveoli, often without substantial deposition and injury.[14] Particles that are 1 to 5 μm in diameter are the most dangerous, because they get lodged at the bifurcation of the distal airways. Coal dust is relatively inert, and large amounts must be deposited in the lungs before lung disease is clinically detectable. Silica, asbestos, and beryllium are more reactive than coal dust, resulting in fibrotic reactions at lower concentrations. Most inhaled dust is entrapped in the mucus blanket and rapidly removed from the lung by ciliary movement. However, some of the particles become impacted at alveolar duct bifurcations, where macrophages accumulate and engulf the trapped particulates. The pulmonary alveolar macrophage is a key cellular element in the initiation and perpetuation of lung injury and fibrosis. Many particles activate the inflammasome and induce IL-1 production. The more reactive particles trigger the macrophages to release a number of products that mediate an inflammatory response and initiate fibroblast proliferation and collagen deposition. Some of the inhaled particles may reach the lymphatics either by direct drainage or within migrating macrophages and thereby initiate an immune response to components of the particulates and/or to self-proteins that are modified by the particles. This then leads to an amplification and extension of the local reaction. Tobacco smoking worsens the effects of all inhaled mineral dusts, more so with asbestos than with any other particle.[7]
Diagnosis
Typical indications on patient assessment include:[15]
- Cough
- Shortness of breath
- Chest tightness
- Chest X-ray may show a characteristic patchy, subpleural, bibasilar interstitial infiltrates or small cystic radiolucencies called honeycombing, particularly in advanced disease.[16][17][18][19]
Pneumoconiosis in combination with multiple pulmonary rheumatoid nodules in rheumatoid arthritis patients is known as Caplan's syndrome.[20][21]
Epidemiology
The prevalence as of 2021 of pneumoconiosis is around 527,500 cases, with over 60,000 new patients reported globally in 2017. Prevalence has trended somewhat downward since 2015.[2] The mortality of pneumoconiosis patients remained at a high level in recent years, with over 21,000 deaths each year since 2015.[2] It is likely that pneumoconiosis is under-diagnosed and under-reported, especially in countries without highly developed healthcare systems.[2]
Treatment and Prognosis
Lung damage due to pneumoconiosis cannot be reversed.[22] However, some steps can slow down disease progression and relieve symptoms. These include the prescription of medications and breathing treatments to open airways and reduce inflammation.[22] Pulmonary rehabilitation and supplemental oxygen may also be recommended.[22] A lung transplant may be needed in cases of serious diseases. If the patient smokes, smoking cessation is also important.[22] Regular testing, such as X-rays or lung function tests, may be indicated to monitor disease progression.
Prevention
To reduce the likelihood of developing pneumoconiosis, individuals working in affected industries should wear a mask, wash skin that comes in contact with dust, remove dust from clothing and wash the face and hands before eating or drinking.[22] In addition, governments often regulate industry, especially mines, to limit how much dust is in the air.[23] In the United States, coal miners injured by pneumoconiosis and their families may receive monthly payments and medical benefits under the Black Lung Benefits Act.[24]
See also
- Aluminosis
- Black Lung Benefits Act of 1972
- Chalicosis
- Philip D'Arcy Hart
- Pneumonoultramicroscopicsilicovolcanoconiosis
- Popcorn workers' lung disease — diacetyl emissions and airborne dust from butter flavorings used in microwave popcorn production
References
- "Pneumoconioses | NIOSH | CDC". www.cdc.gov. 2022-03-21. Retrieved 2022-04-01.
- Qi, Xian-Mei; Luo, Ya; Song, Mei-Yue; Liu, Ying; Shu, Ting; Liu, Ying; Pang, Jun-Ling; Wang, Jing; Wang, Chen (2021-04-13). "Pneumoconiosis: current status and future prospects". Chinese Medical Journal. 134 (8): 898–907. doi:10.1097/CM9.0000000000001461. ISSN 2542-5641. PMC 8078400. PMID 33879753.
- DeLight, Navina; Sachs, Howard (2022), "Pneumoconiosis", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 32310362, retrieved 2022-04-01
- American Thoracic Society (2004). "Diagnosis and Initial Management of Nonmalignant Diseases Related to Asbestos". American Journal of Respiratory and Critical Care Medicine. 170 (6): 691–715. doi:10.1164/rccm.200310-1436ST. PMID 15355871.
- Hall, Noemi B.; Blackley, David J.; Halldin, Cara N.; Laney, A. Scott (September 2019). "Current Review of Pneumoconiosis Among US Coal Miners". Current Environmental Health Reports. 6 (3): 137–147. doi:10.1007/s40572-019-00237-5. ISSN 2196-5412. PMC 7055360. PMID 31302880.
- Shih, Gerry (15 December 2019). "They built a Chinese boomtown. It left them dying of lung disease with nowhere to turn". New York Times. Retrieved 16 December 2019.
- Kumar, MBBS, MD, FRCPath, Vinay (2013). Robbins Basic Pathology 9th Edition. Philadelphia, Pennsylvania: Elsevier Saunders. pp. 474–475. ISBN 978-1-4377-1781-5.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Schenker, Marc B.; Pinkerton, Kent E.; Mitchell, Diane; Vallyathan, Val; Elvine-Kreis, Brenda; Green, Francis H.Y. (2009). "Pneumoconiosis from Agricultural Dust Exposure among Young California Farmworkers". Environmental Health Perspectives. 117 (6): 988–994. doi:10.1289/ehp.0800144. PMC 2702418. PMID 19590695.
- DeLight, Navina (2020). Pneumoconiosis. StatPearls.
- "Silicosiderosis". NORD (National Organization for Rare Disorders). Retrieved 2022-04-01.
- "Silicosiderosis | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2022-04-01.
- "Baritosis | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2022-04-01.
- Fujimura, Naoki (March 2000). "Pathology and pathophysiology of pneumoconiosis". Current Opinion in Pulmonary Medicine. 6 (2): 140–144. doi:10.1097/00063198-200003000-00010. ISSN 1070-5287. PMID 10741774.
- Heppleston, A. G. (June 1988). "Prevalence and pathogenesis of pneumoconiosis in coal workers". Environmental Health Perspectives. 78: 159–170. doi:10.1289/ehp.8878159. ISSN 0091-6765. PMC 1474620. PMID 3060352.
- "Diagnosing and Treating Pneumoconiosis". www.lung.org. Retrieved 2022-04-01.
- Chong, Semin; Lee, Kyung Soo; Chung, Myung Jin; Han, Joungho; Kwon, O Jung; Kim, Tae Sung (2006-01-01). "Pneumoconiosis: Comparison of Imaging and Pathologic Findings". RadioGraphics. 26 (1): 59–77. doi:10.1148/rg.261055070. ISSN 0271-5333. PMID 16418244.
- Brichet, Anne; Tonnel, André Bernard; Brambilla, Elizabeth; Devouassoux, Gilles; Rémy-Jardin, Martine; Copin, Marie-Christine; Wallaert, Benoit; Groupe d'Etude en Pathologie Interstitielle (GEPI) de la Société de Pathologie Thoracique du Nord (October 2002). "Chronic interstitial pneumonia with honeycombing in coal workers". Sarcoidosis, Vasculitis, and Diffuse Lung Diseases. 19 (3): 211–219. ISSN 1124-0490. PMID 12405491.
- Arakawa, Hiroaki; Honma, Koichi (April 2011). "Honeycomb Lung: History and Current Concepts". American Journal of Roentgenology. 196 (4): 773–782. doi:10.2214/AJR.10.4873. ISSN 0361-803X. PMID 21427324.
- Masanori, Akira (2021-03-10). "Imaging diagnosis of classical and new pneumoconiosis: predominant reticular HRCT pattern". Insights into Imaging. 12 (1): 33. doi:10.1186/s13244-021-00966-y. ISSN 1869-4101. PMC 7947097. PMID 33689008.
- Andreoli, Thomas, ed. CECIL Essentials of Medicine. Saunders: Pennsylvania, 2004. p. 737.
- "Rheumatoid pneumoconiosis: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2022-04-01.
- "Pneumoconiosis Symptoms, Causes and Risk Factors". www.lung.org. Retrieved 2022-04-01.
- Office, U. S. Government Accountability. "Mine Safety: Reports and Key Studies Support the Scientific Conclusions Underlying the Proposed Exposure Limit for Respirable Coal Mine Dust". www.gao.gov. Retrieved 2022-04-01.
- "General | U.S. Department of Labor". www.dol.gov. Retrieved 2022-04-01.
Further reading
- Cochrane, A.L.; Blythe, M. (1989). One Man's Medicine, an autobiography of Professor Archie Cochrane. London: BMJ Books. ISBN 0727902776. (Paperback ed. (2009) Cardiff University ISBN 0954088433.
External links
- "Pneumoconioses". NIOSH Safety and Health Topic. Center for Disease Control. 30 March 2022.
- "Black Lung Benefits Act". U.S. Department of Labor. Archived from the original on 2010-05-27. Retrieved 2007-03-02.
- Coal Workers' Pneumoconiosis at Merck Manual of Diagnosis and Therapy Professional Edition
- Black Lung — United Mine Workers of America
- "Black Lung" (PDF). U.S. Department of Labor Mine Safety and Health Administration. Archived from the original (PDF) on 2010-05-30.
- A Conversation about Mining and Black Lung Disease
- Flavorings-Related Lung Disease
- The Institute of Occupational Medicine and its research into pneumocomiosis
- Miller, B.G.; Kinnear, A.G. Pneumoconiosis in coalminers and exposure to dust of variable quartz content (PDF) (Technical report). Institute of Occupational Medicine. TM/88/17.