Staphylococcus capitis
Staphylococcus capitis is a coagulase-negative species (CoNS) of Staphylococcus. It is part of the normal flora of the skin of the human scalp, face, neck, scrotum, and ears and has been associated with prosthetic valve endocarditis, but is rarely associated with native valve infection.[1]
| Staphylococcus capitis | |
|---|---|
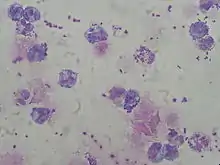 | |
| Staphylococcus capitis in cerebrospinal fluid. | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Bacillota |
| Class: | Bacilli |
| Order: | Bacillales |
| Family: | Staphylococcaceae |
| Genus: | Staphylococcus |
| Species: | S. capitis |
| Binomial name | |
| Staphylococcus capitis Kloos and Schleifer 1975 (Approved Lists 1980) | |
Clinical importance
CoNS produce a slimy biofilm enabling them to adhere to medical devices such as prosthetic valves and catheters and makes them difficult to remove by patient immune response to antibiotic therapy. As native flora of the skin and mucous membranes, they may be introduced anytime these are punctured, i.e. at the time of device placement, venipuncture, or through breaks in the mucous membrane or skin. CoNS species, such as S. epidermidis and S. capitis, are recorded as the most common cause of prosthetic valve endocarditis.[2][3][4]
Staphylococcus capitis, fortunately, has a lower propensity to antibiotic resistance and also produces less biofilm than many other CoNS. This improves chances of successful eradication of S. capitis in periprosthetic infections (as total knee and total hip arthroplasty infections) relative to other CoNS such as S. epidermidis .[5]
New studies show that the organism can be taken from prosthetic joint infections, most likely contracted from surgery. This organism is shown in creating human disease and can easily be spread in the hospital so knowing where the bacteria comes from is vital in improving treatment algorithms in the future.[6]
Background
Staphylococcus capitis is a bacteria that colonizes the skin, scalp, face and neck. Contacting Staphylococcus capitis is not a disaster for healthy people. Immunocompromised individuals, on the other hand, might develop poisoning symptoms and even endocarditis as a result of microorganisms entering the body. Although bacteria of the species Staphylococcus capitis are a natural element of human flora, they can be dangerous to immunocompromised patients. This is especially true when bacteria enter the body.[7]
Morphology
Staphylococcus capitis was originally detected in human skin in 1975 and categorized as a coagulase negative staphylococci (CoNS) species. Staphylococcus capitis bacteria preferentially dwell on the skin and mucous membranes of humans and other warm-blooded animals. Warm-blooded creatures provide a very conducive environment for bacteria to grow, since the ideal temperature for bacteria to thrive is between 30 and 37 degrees Celsius. They are tolerated by the human immune system when applied to the skin. Because of their inept behavior, they must be translated. Bacteria are spherical cells 0.5 to 1.5 µm in diameter, not rod-shaped. Staphylococci are incapable of active movement and are organized singly, in pairs, or in grape-like clusters. All staphylococci develop anaerobically on one side. That is, they can metabolize even when there is no oxygen present. However, when oxygen is available in their surroundings, their metabolism becomes active.[8] Staphylococcus capitis TE8 was isolated from the skin surface of a healthy adult foot and found to have potent antibacterial action against Gram-positive bacteria such as Staphylococcus aureus.[9] Staphylococcus is a gram-positive bacterial spherule. Some staphylococci are capable of producing free coagulase. Thus, that is used to differentiate Staphylococcus species. In this context, a distinction is made in species between coagulase-positive and coagulase-negative staphylococci. Staphylococcus capitis is a species in the genus that is positive for staph coagulase.[10]
Methods
Shotgun and paired-end pyrosequencing were one of the technique using to study the genome of Staph. Capitis. Researchers get a 109-fold coverage of the whole genome of S. Capitis. The clinical and subclinical isolates are found in a broad variety of clades and do not exhibit any evident link, according to analysis of the 16S RNA genes from the genome sequences of Staphylococcus spp. from bovine and buffalo mastitis cases.[9]
Genomes
The whole genome of S. capitis will help researchers better understand the evolution and pathophysiology of coagulase-negative staphylococci in the future. Staphylococcus capitis is a coagulase-negative staphylococci opportunistic pathogen (CoNS). S. Capitis was described as the absence of accessible full genome sequences in S. capitis functional genomic investigations was restricted to this day. S. capitis' connections with S. epidermidis are more evolutionarily than other clinically important negative coagulase staphylococcus. The smallest genome among the closed genomes sequenced to date is S. capitis with the least expected CDS. The paucity of full genome sequences for S. capitis has hampered functional genomic investigations thus far. In a nutshell, bacteria were cultured as previously described, planktonic cells were removed, and biofilms were rinsed three times in PBS. Other therapeutically relevant coagulase negative staphylococci have closer evolutionary ties to S. epidermidis than S. capitis. There are 2304 protein-coding DNA sequences predicted on the chromosome, six rRNA operons, 63 tRNA genes, and a single tmRNA gene. With the fewest projected CDS of all closed staphylococcal genomes sequenced to date, S. capitis has the smallest genome of all closed staphylococcal genomes sequenced to date. Proteases like ClpP in S. Capitis, which helps create biofilms, and SepA, which has been demonstrated to degrade host antimicrobial peptides in CoNS, as well as hemolysins, lipases, and esterases, are among them. In contrast to the acute illness enabled by conventional exoproteins of the more virulent staphylococcal species, S. aureus, these proteins are expected to facilitate immune evasion, host colonization, and persistence.[11]
Staphylococci are organized individually, in pairs or clusters similar to grapes, and cannot be actively migrated. All staphylococci are anaerobic unilaterally growing. They have catalase instead of oxidase: an enzyme that turns hydrogen peroxide in oxygen and water into energy. As the information written above is based on the phylogeny of S. Capitis, this can be listed into an Evolution relationship section that briefly describes their morphology and how they were found to be related to other Staph families.[11]
Evolutions
This Bacterium’s evolution through genome expression in very detail and in comparison with other relatives of the Staphylococci as well with experiments and data that have been collected in the past. S. Capitis’ genomes with a deeper understanding of this species and how evolutionary related it is to other Bacterium (S. capitis has a closer evolutionary link to S. epidermidis than other clinically relevant coagulase negative staphylococci), we could discover with more information whether this species' cause of the disease is connected to other species.[11] Although they cause different pathogenic virulence, they have many similar features in their genetics and morphology. The main causes of nosocomial infections, in particular nosocomial bacteremias, have emerged as coagulase-negative staphylococci (CoNS). The capacity to produce biofilm from implanted equipment surfaces is CoNS's most significant mechanism for pathogenicity. Starting very early, research into biofilm formation in Staphylococcus epidermidis has served as a model for other staphylococci such as Staphylococcus aureus and other CoNS species. Moreover, data also showed that S. capitis have a strain (AYP1020) that researchers use to general genomic characteristics compared to S. epidermidis’ strain (RP62a). Thus, in comparison study, S. epidermidis (RP62a) was identified as a near related with S. capitis and as the therapeutically highly significant coagulase-negative staphylococci (CoNS). This source showed very detailed studies of S. Capitis’ relationship among its Staph families highlighting clearly the significance between itself and S. epidermidis.[12]
Pathogenesis
Most scientists and the general public are interested in the Bacterium because of its connection to several human ailments, and they may learn more on Wikipedia about how the Bacterium causes these diseases. Although bacteria of the species Staphylococcus capitis are a natural element of human flora, they can be dangerous to immunocompromised patients.[11]
This is especially true when bacteria enter the body. Staphylococcus capitis is a kind of CoNS that typically affects the head (especially the ears and forehead), arms, and infrequently the legs. A recent research found that 20% of people had persistent populations on their heads and arms after a year. There are two subspecies of Staphylococcus capitis: subsp. urealyticus and subsp. capitis. During antibiotic therapy, the former, but not the latter, has been demonstrated to expand its range of habitats outside the brain. Human diseases are found in both subspecies. S. capitis has been linked to peritoneal dialysis peritonitis, prosthetic-valve endocarditis, pacemaker endocarditis, meningitis, acetabulum osteomyelitis, and spondylodiscitis, according to case reports. It's also a well-known pathogen in neonatal sepsis, where genetic fingerprinting has shown its ability for clonal nosocomial dissemination. All nine S. capitis isolates from blood cultures in neonatal intensive care units (NICUs) had vancomycin-heteroresistant subpopulations, according to the study.[13]
Staphylococcus capitis is a coagulase-negative staphylococcus that can infect native heart valves and cause endocarditis. The authors describe two instances of S capitis-induced native valve endocarditis in individuals with aortic valve dysfunction. S capitis, a different species, is found in the typical microflora of the human scalp, face, neck, and ears. It is known to cause infection surrounding prosthetic devices, as is the case with other CoNS, but it is infrequently recognized as a cause of endocarditis; our instances bring the total number of cases documented to eight. Seven of the eight instances had an underlying heart problem that might have predisposed the patient to infection.[14]
Treatments
Treatment with vancomycin is a significant risk factor. Gut colonization of S. capitis was not linked to S. capitis. An additional Cox model using S. capitis gut colonization as the end point was used to investigate the link between colonization and colonization. Surprisingly, the link was significant, with an HR of 3.45 (95% confidence range 2.07–5.76, p0.001). Thus, our analyses discovered links between vancomycin therapy and S. capitis gut colonization, but not between S. capitis colonization [15]
References
- Kloos, W. E.; Schleifer, K. H. (1975). "Isolation and Characterization of Staphylococci from Human Skin II. Descriptions of Four New Species: Staphylococcus warneri, Staphylococcus capitis, Staphylococcus hominis, and Staphylococcus simulans". International Journal of Systematic Bacteriology. 25 (1): 62–79. doi:10.1099/00207713-25-1-62. ISSN 0020-7713.
- Van Der Zwet WC, Debets-Ossenkopp YJ, Reinders E, et al. (July 2002). "Nosocomial spread of a Staphylococcus capitis strain with heteroresistance to vancomycin in a neonatal intensive care unit". J. Clin. Microbiol. 40 (7): 2520–5. doi:10.1128/JCM.40.7.2520-2525.2002. PMC 120592. PMID 12089273.
- D'mello D, Daley AJ, Rahman MS, et al. (September 2008). "Vancomycin heteroresistance in bloodstream isolates of Staphylococcus capitis". J. Clin. Microbiol. 46 (9): 3124–6. doi:10.1128/JCM.00592-08. PMC 2546727. PMID 18596138.
- Iwase T, Seki K, Shinji H, Mizunoe Y, Masuda S (October 2007). "Development of a real-time PCR assay for the detection and identification of Staphylococcus capitis, Staphylococcus haemolyticus and Staphylococcus warneri". J. Med. Microbiol. 56 (Pt 10): 1346–9. doi:10.1099/jmm.0.47235-0. PMID 17893172.
- Kloos WE PMC 358308, Update on clinical significance of coagulase-negative staphylococci. Clin Microbiol Rev. 1994 Jan; 7(1): 117–140
- Tevell, S.; Hellmark, B.; Nilsdotter-Augustinsson, Å.; Söderquist, B. (2017). "Staphylococcus capitis isolated from prosthetic joint infections". European Journal of Clinical Microbiology & Infectious Diseases. 36 (1): 115–122. doi:10.1007/s10096-016-2777-7. PMC 5203848. PMID 27680718.
- Kloos, Wesley E. (1981), Maibach, Howard I.; Aly, Raza (eds.), "The Identification of Staphylococcus and Micrococcus Species Isolated from Human Skin", Skin Microbiology, New York, NY: Springer US, pp. 3–12, doi:10.1007/978-1-4612-5868-1_1, ISBN 978-1-4612-5870-4, retrieved 2021-12-13
- Otto, Michael (April 2010). "Staphylococcus colonization of the skin and antimicrobial peptides". Expert Review of Dermatology. 5 (2): 183–195. doi:10.1586/edm.10.6. ISSN 1746-9872. PMC 2867359. PMID 20473345.
- Pizauro, Lucas José Luduverio; de Almeida, Camila Chioda; Silva, Saura Rodrigues; MacInnes, Janet I.; Kropinski, Andrew M.; Zafalon, Luiz Francisco; de Avila, Fernando Antônio; de Mello Varani, Alessandro (December 2021). "Genomic comparisons and phylogenetic analysis of mastitis-related staphylococci with a focus on adhesion, biofilm, and related regulatory genes". Scientific Reports. 11 (1): 17392. Bibcode:2021NatSR..1117392P. doi:10.1038/s41598-021-96842-2. ISSN 2045-2322. PMC 8405628. PMID 34462461.
- DEVRIESE, L.A.; SCHLEIFER, K.H.; ADEGOKE, G.O. (January 1985). "Identification of coagulase-negative staphylococci from farm animals". Journal of Applied Bacteriology. 58 (1): 45–55. doi:10.1111/j.1365-2672.1985.tb01428.x. ISSN 0021-8847. PMID 3980296.
- Cameron, David R.; Jiang, Jhih-Hang; Hassan, Karl A.; Elbourne, Liam D. H.; Tuck, Kellie L.; Paulsen, Ian T.; Peleg, Anton Y. (2015-09-23). "Insights on virulence from the complete genome of Staphylococcus capitis". Frontiers in Microbiology. 6: 980. doi:10.3389/fmicb.2015.00980. ISSN 1664-302X. PMC 4585213. PMID 26441910.
- Cui, Bintao; Smooker, Peter M.; Rouch, Duncan A.; Daley, Andrew J.; Deighton, Margaret A. (January 2013). "Differences between Two Clinical Staphylococcus capitis Subspecies as Revealed by Biofilm, Antibiotic Resistance, and Pulsed-Field Gel Electrophoresis Profiling". Journal of Clinical Microbiology. 51 (1): 9–14. doi:10.1128/JCM.05124-11. ISSN 0095-1137. PMC 3536240. PMID 23052315.
- Tevell, S.; Hellmark, B.; Nilsdotter-Augustinsson, Å.; Söderquist, B. (January 2017). "Staphylococcus capitis isolated from prosthetic joint infections". European Journal of Clinical Microbiology & Infectious Diseases. 36 (1): 115–122. doi:10.1007/s10096-016-2777-7. ISSN 0934-9723. PMC 5203848. PMID 27680718.
- Sandoe, J A T; Kerr, K G; Reynolds, G W; Jain, S (1999-09-01). "Staphylococcus capitis endocarditis: two cases and review of the literature". Heart. 82 (3): e1. doi:10.1136/hrt.82.3.e1. ISSN 1355-6037. PMC 1729175. PMID 10455099.
- Butin, M.; Rasigade, J.-P.; Subtil, F.; Martins-Simões, P.; Pralong, C.; Freydière, A.-M.; Vandenesch, F.; Tigaud, S.; Picaud, J.-C.; Laurent, F. (November 2017). "Vancomycin treatment is a risk factor for vancomycin-nonsusceptible Staphylococcus capitis sepsis in preterm neonates". Clinical Microbiology and Infection. 23 (11): 839–844. doi:10.1016/j.cmi.2017.03.022. PMID 28373147.