Therapeutic endoscopy
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.
| Therapeutic endoscopy | |
|---|---|
| Other names | interventional gastroenterology or interventional endoscopy or operative endoscopy |
A number of different techniques have been developed to allow treatment to be carried out endoscopically, to treat disorders such as bleeding, strictures and polyps.
Types of endoscopic therapy
Endoscopic haemostasis
Endoscopic injection of bleeding peptic ulcers with adrenaline has been practised since the 1970s,[1] endoscopic heater probes have been used since the 1980s,[2] and Argon plasma coagulation has been used since the 1990s. More recently, adrenaline injection tends to be combined with either heater probe coagulation or argon plasma coagulation to minimize the chance of an ulcer rebleeding. The disadvantage of this treatment is a low risk of perforation of the gastric wall and a low risk of peritonitis.[3] Combined therapy may work better than epinephrine alone. However, there is no evidence that one kind of treatment is more effective than the other.[3]
Injection sclerotherapy
Injection sclerotherapy has been used to treat oesophageal varices since the 1960s.[4] A sheathed needle is passed through a channel in the endoscope, unsheathed and pushed into a varix. A sclerosing agent, such as ethanolamine or absolute alcohol, is then injected into the varix to cause scarring and constriction of the varix with the aim of obliterating the varix (or varices). This technique has now largely been superseded by variceal band ligation.
Sclerotherapy has also been used in the treatment of gastric varices since the late 1980s.[5] In this case Histoacryl glue (cyanoacrylate) is commonly used as the sclerosant.[6] This technique is favoured over band ligation because the position of the varices in the stomach, most often in the gastric fundus, makes the placing of bands very difficult.
Argon plasma coagulation

Argon plasma coagulation (APC) has been used to provide tissue coagulation and haemostasis since the early part of the 1990s.[7] A stream of argon gas is passed through an endoscopic catheter; this is then ionized at the tip of the catheter by an electric current. The tip of the catheter is held close to the tissue to be treated, and the current arcs across to the tissue causing a superficial (2–3 mm) burn. The lack of contact between the catheter and the tissue stops the tendency of the catheter to stick to the tissue, reducing unwanted tissue damage.[8]
Its principal use is in providing haemostasis in gastrointestinal bleeding; angiodysplasia, GAVE,[9] bleeding malignant tumours and bleeding peptic ulcers can all be treated. Trials have also been carried out to assess its use in eradicating Barrett’s oesophagus, but have found that relapse is common.[10]
Dilatation

Dilatation of benign oesophageal strictures using semi-rigid bougies existed long before the advent of flexible endoscopes.[11] Since that time oesophageal dilatation has been carried out using either bougies or endoscopic balloons, and can be used to treat benign oesophageal strictures and achalasia.
Initially, bougies were used to dilate benign strictures of the oesophagus. These could be passed alongside the endoscope, allowing visualisation of the bougie passing through the stricture,[12] but the technique of passing a guidewire through the stricture endoscopically, then removing the endoscope and passing the bougie over the guidewire was more commonly used.[13]
More recently, balloon dilatation of the oesophageal strictures has become more common. It is thought that this technique carries a lower complication rate than the use of bougies, and since endoscopy balloons are single use items there are no concerns about equipment sterilization.[11] In addition to oesophageal dilatation, endoscopic balloons can also be used to dilate pyloric strictures.[14]
Polypectomy

Endoscopic polypectomy has been carried out since the early 1970s by both endoscopic snare removal and fulguration of polyps with hot biopsy forceps.[15][16]
Variceal banding
Oesophageal varices have been treated by band ligation since the late 1980s.[17]
Stenting
Expandable mesh stents can be deployed in the oesophagus at endoscopy, primarily in patients with inoperable oesophageal cancer which is causing dysphagia.[18]
Plastic stents can also be used to relieve obstruction of the common bile duct at ERCP.[19]
Percutaneous endoscopic gastrostomy
A method for inserting a feeding gastrostomy tube without the need for surgery was first described in 1980.[20] This endoscopic technique is of particular use as many patients who require feeding tubes (such as after patients with swallowing difficulties after a stroke) are at high risk for complications from anaesthesia and surgery; the endoscopic technique usually requires mild sedation only.
Foreign body removal
Foreign bodies commonly impact in the lower oesophagus, and removal of these by pushing them into the stomach has been practised since the Middle Ages.[11] Foreign body retrieval, using forceps and magnets, has been practised since the time of rigid oesophagoscopy and bronchoscopy.
Areas under development
Anti-reflux procedures
A number of techniques are being developed for the endoscopic treatment of gastro-oesophageal reflux disease as an alternative to laparoscopic Nissen fundoplication.[21]
Treatment of Barrett's oesophagus
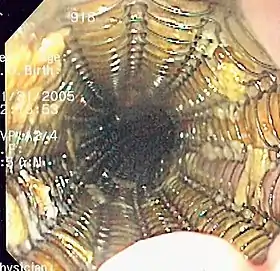
Endoscopic circumferential radiofrequency ablation is being developed in an effort to obviate long-term endoscopic surveillance in patients with Barrett's oesophagus, and to reduce the risk of development of oesophageal carcinoma. Previous techniques, such as Argon plasma coagulation, have been unsuccessful because of incomplete removal of the Barrett's mucosa and therefore relapse of part of the treated area.[10] Newer techniques using circumferential radiofrequency ablation, which allows larger areas of the oesophagus to be treated at one time giving a more uniform area of treatment, are showing more promising short-term results.[22]
Transoral gastroplasty (TOGA procedure)
Early trials are under way to evaluate an endoscopic technique for gastric stapling, a type of bariatric surgery, which aims to induce long-term weight loss in morbidly obese patients.[23]
References
- Hirao, M.; Kobayashi, T.; Masuda, K.; Yamaguchi, S.; Noda, K.; Matsuura, K.; Naka, H.; Kawauchi, H.; Namiki, M. (October 1985). "Endoscopic local injection of hypertonic saline-epinephrine solution to arrest hemorrhage from the upper gastrointestinal tract". Gastrointest. Endosc. 31 (5): 313–7. doi:10.1016/S0016-5107(85)72213-4. ISSN 0016-5107. PMID 3876253. Retrieved 2013-12-28.

- Sung, S. Y.; Chung, S. C. S.; Lo, K. K.; Leung, J. W. C. (1988). "Heater-probe treatment of bleeding peptic ulcers". Surg. Endosc. 2 (4): 234–236. doi:10.1007/BF00705328. PMID 3071870. S2CID 26190281.

- Vergara, Mercedes; Bennett, Cathy; Calvet, Xavier; Gisbert, Javier P. (2014-10-13). Vergara, Mercedes (ed.). "Epinephrine injection versus epinephrine injection and a second endoscopic method in high-risk bleeding ulcers". The Cochrane Database of Systematic Reviews (10): CD005584. doi:10.1002/14651858.CD005584.pub3. ISSN 1469-493X. PMID 25308912.
- Hunt, P. S.; Johnston, G. W.; Rodgers, H. W. (April 1969). "The emergency management of bleeding oesophageal varices with sclerosing injections". Br. J. Surg. 56 (4): 305–307. doi:10.1002/bjs.1800560416. PMID 4952481. S2CID 46306862.

- Sarin, S. K.; Kumar, A. (October 1989). "Gastric varices: profile, classification, and management". Am. J. Gastroenterol. 84 (10): 1244–1249. PMID 2679046.
- Kind, R.; Guglielmi, A.; Rodella, L.; Lombardo, F.; Catalano, F.; Ruzzenente, A.; Borzellino, G.; Girlanda, R.; Leopardi, F. (July 2000). "Bucrylate treatment of bleeding gastric varices: 12 years' experience". Endoscopy. 32 (7): 512–519. doi:10.1055/s-2000-3817. ISSN 0013-726X. PMID 10917182.

- Grund, K. E.; Storek, D.; Farin, G. (February 1994). "Endoscopic argon plasma coagulation (APC) first clinical experiences in flexible endoscopy". Endosc. Surg. Allied Technol. 2 (1): 42–46. ISSN 0942-6027. PMID 8081915.
- Farin, G.; Grund, K. E. (February 1994). "Technology of argon plasma coagulation with particular regard to endoscopic applications". Endosc. Surg. Allied Technol. 2 (1): 71–77. ISSN 0942-6027. PMID 8081921.
- Garcia, Jr., Nelson; Sanyal, Arun J. (April 2001). "Portal Hypertensive Gastropathy and Gastric Antral Vascular Ectasia". Curr. Treat. Options Gastroenterol. 4 (2): 163–171. doi:10.1007/s11938-001-0028-0. ISSN 1092-8472. PMID 11469974. S2CID 179379.

- Van Laethem, J-L.; Cremer, M; Peny, M.O.; Delhaye, M; Devière, J (December 1998). "Eradication of Barrett's mucosa with argon plasma coagulation and acid suppression: immediate and mid term results". Gut. 43 (6): 747–751. doi:10.1136/gut.43.6.747. PMC 1727342. PMID 9824599.

- Riley, S. A.; Attwood, S. E. A. (2004). "Guidelines on the use of oesophageal dilatation in clinical practice". Gut. 53 (suppl 1): i1–16. doi:10.1136/gut.53.suppl_1.i1. PMC 1867767. PMID 14724139.

- Chung, Shiroos; Safaie-Shirazi, Raphael S. K.; Denbesten, Lawrence (July 1976). "Dilation of esophageal strictures. A new technique controlled by fiberoptic endoscopy". Arch. Surg. 111 (7): 795–798. doi:10.1001/archsurg.1976.01360250071014. PMID 938225.

- Dupin B, Meric B, Dumon JF (October 1987). "Techniques, results and complications of oesophageal dilatation". Baillière's Clinical Gastroenterology. 1 (4): 809–20. doi:10.1016/0950-3528(87)90020-0. PMID 3329544.
- Lindor KD, Ott BJ, Hughes RW (September 1985). "Balloon dilatation of upper digestive tract strictures". Gastroenterology. 89 (3): 545–8. doi:10.1016/0016-5085(85)90449-4. PMID 4018500.
- Williams C (November 1972). "Use of the long colonoscope for examination of the whole colon and for polypectomy". Proc. R. Soc. Med. 65 (11): 967. PMC 1644729. PMID 4539317.
- Sivak MV, Sullivan BH (1973). "Gastroscopic polypectomy". Cleve Clin Q. 40 (3): 153–7. doi:10.3949/ccjm.40.3.153. PMID 4752356.
- Stiegmann GV, Goff JS, Sun JH, Wilborn S (February 1989). "Endoscopic elastic band ligation for active variceal hemorrhage". Am Surg. 55 (2): 124–8. PMID 2644882.
- Domschke W, Foerster EC, Matek W, Rödl W (May 1990). "Self-expanding mesh stent for esophageal cancer stenosis". Endoscopy. 22 (3): 134–6. doi:10.1055/s-2007-1012818. PMID 1694122.
- Zimmon DS, Clemett AR (October 1982). "Endoscopic stents and drains in the management of pancreatic and bile duct obstruction". Surg. Clin. North Am. 62 (5): 837–44. doi:10.1016/S0039-6109(16)42833-1. PMID 7123457.
- Gauderer, Michael W. L.; Ponsky, Jeffrey L.; Izant, Jr., Robert J. (December 1980). "Gastrostomy without laparotomy: a percutaneous endoscopic technique". J. Pediatr. Surg. 15 (6): 872–875. doi:10.1016/S0022-3468(80)80296-X. ISSN 0022-3468. PMID 6780678.

- Chen D, Barber C, McLoughlin P, Thavaneswaran P, Jamieson GG, Maddern GJ (January 2009). "Systematic review of endoscopic treatments for gastro-oesophageal reflux disease". Br J Surg. 96 (2): 128–136. doi:10.1002/bjs.6440. PMID 19160349. S2CID 22481876.
- Eldaif SM, Lin E, Singh KA, Force SD, Miller DL (February 2009). "Radiofrequency Ablation of Barrett's Esophagus: Short-Term Results". Ann. Thorac. Surg. 87 (2): 405–411. doi:10.1016/j.athoracsur.2008.11.043. PMID 19161747.
- Moreno, C.; Closset, J.; Dugardeyn, S.; Baréa, M.; Mehdi, A.; Collignon, L.; Zalcman, M.; Baurain, M.; Le Moine, O.; Devière, J. (May 2008). "Transoral gastroplasty is safe, feasible, and induces significant weight loss in morbidly obese patients: results of the second human pilot study". Endoscopy. 40 (5): 406–413. doi:10.1055/s-2007-995748. ISSN 0013-726X. PMID 18459077.