Total intravenous anaesthesia
Total intravenous anesthesia (TIVA) refers to the intravenous administration of anesthetic agents to induce a temporary loss of sensation or awareness. The first study of TIVA was done in 1872 using chloral hydrate,[1] and the common anesthetic agent propofol was licensed in 1986. TIVA is currently employed in various procedures as an alternative technique of general anesthesia in order to improve post-operative recovery.
TIVA is maintained by intravenous infusion devices and assisted by electroencephalography (EEG) monitoring. These techniques facilitate the use of propofol, etomidate, ketamine, and other intravenous anesthetic agents. During or after TIVA, patients may be subjected to an elevated risk of anesthesia awareness, hyperalgesia and neurotoxicity.[2] Considering these risks, special consideration is given to obese, elderly and pediatric patients.
History
In the mid-19th century, specific equipment was developed to enable intravenous anesthesia. Francis Rynd developed the hollow needle in 1845,[1] and Charles Gabriel Pravaz developed the syringe in 1853,[1] which allowed drugs to be administered intravenously.
Using this new mode of delivery, many chemical compounds were tested as intravenous anesthetics. This was pioneered by Pierre-Cyprian Ore in 1872, who reported using chloral hydrate as an intravenous anesthetic.[1] However, these early trials were associated with high mortality.[1] Hedonal was later developed in 1909 for general anesthesia, although with limited success due to its long duration of effect.[3] These insufficiencies encouraged the development of paraldehyde by Noel & Souttar,[4] magnesium sulfate by Peck & Meltzer[5] as well as ethanol by Nakagawa[6] as intravenous anesthetic agents.
Propofol (di-isopropyl phenol) was synthesized by Glen and colleagues in the early 1970s,[7] but its first formulations were temporarily withdrawn due to a number of adverse reactions during clinical studies.[1] In 1983, a lipid emulsion formulation of propofol was available, which carried great potential during clinical trials.[8] It was licensed for use in Europe in 1986 and received FDA approval in the US in 1989.[1] Propofol is now used worldwide with a well-defined pharmacological profile for a variety of medical uses.
Medical uses
TIVA is used to induce general anesthesia while avoiding the disadvantages of volatile anesthesia (and traditional inhalation agents).[9] Intravenous anesthetic agents are titrated at safe doses to maintain stage III surgical anesthesia (unconsciousness, amnesia immobility, and absence of response to noxious stimulation).[10] The use of TIVA is advantageous in cases where volatile anesthesia is of high risk or is impossible, such as cases involving morbidly obese patients.[11][12] TIVA has also been used for anesthetic delivery at sites of trauma such as serious accidents, disasters and wars.[1]
The overall goals of TIVA include:[13]
- Smooth induction of anesthesia
- Reliable and measurable maintenance of anesthesia
- Rapid emergence out of the effects of infused drugs as soon as the infusion is terminated.
Propofol-based TIVA significantly improves post-operative recovery profile and comfort, minimizes nausea and vomiting, facilitates rapid recovery, greater hemodynamic stability, preservation of hypoxic pulmonary vasoconstriction, reduction in intracerebral pressure, and reduces the risk of organ toxicity.[14] Despite these advantages, it accounts for a small proportion of general anesthetics due to the relatively expensive cost of preparation and maintenance.[15]
Techniques
Dosing considerations
The doses for intravenous sedative-hypnotic and adjuvant agents vary individually. Pharmacodynamic and pharmacokinetic factors need to be considered for each patient (e.g. patients with impaired kidney or liver function, blood abnormalities and myocardial dysfunction, etc.)[16] There are also risks of adverse effects related to doses such as hypotension and respiratory depression.[17] In terms of adjuvant agents, the co-administration of anesthetic drugs from different classes often produce synergistic hypnotic effects.[18][19] This is especially common for agents acting on gamma-aminobutyric acid (GABA) receptors that are combined with drugs acting on different types of receptors.[20][21]
The drug interactions between sedative-hypnotic agents and adjuvant agents suggest that dosing regimens cannot be fixed.[22] Instead, dosing should be based on adjusted body weight or estimated lean body weight, especially for obese patients. It is recommended that drug doses be titrated in brief intervals (around 20 to 60 seconds).[23]
Equipment
The delivery of intravenous anesthetics is dependent on different types of infusion devices. Examples of infusion devices include smart pumps, syringe pumps and target-controlled infusion (TCI) devices.[24]
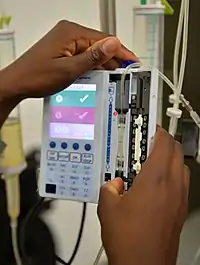
Smart pumps are commonly used to administer potent anesthetics and various vasoactive drugs such as vasopressors, inotropes, vasodilators, which need to be continuously titrated in the operating room.[25] Smart pumps are advantageous since they administer safe doses with a programmed infusion rate within pre-existing limits based on the institutional standardized medication library.[26]
Syringe pumps are smaller infusion pumps that allow the administration of small amounts of induction agents at a precise rate.[27] The accuracy of syringe pumps is dependent on the selection of syringes during pump programming. Most pumps are able to identify the size of the syringe automatically when the syringe manufacturer's name is input correctly.[28]
Target-controlled infusion (TCI) systems are assisted by computer systems that make use of pharmacokinetic and pharmacodynamic modelling to maintain a target concentration of anesthetic in the brain.[29][30] TCI requires clinicians to input a target concentration for an anesthetic or other agents, and the computer will calculate the amount of agent required for the input concentration, then the infusion pump will be used to deliver the calculated bolus dose.[31] Subsequently, the computer continuously recalculates how much drug is in the system and influences the amount of drug required to maintain the desired concentration at the effect site.[32]

Maintenance
During TIVA, the continuous assessment of heart rate, blood pressure, and state of consciousness is essential when titrating anesthetic agents.[20][24] Processed electroencephalogram (EEG) monitoring is used to assess anesthetic depth.[33] However, there are 30 seconds of lag time between the subject's state of consciousness and the processed EEG signal. This limits its usefulness during the induction of anesthesia.[20][21]
Intravenous agents
Propofol, etomidate and ketamine are common intravenous sedative-hypnotic agents for the induction of TIVA.[34] Their highly lipophilic nature allows the rapid onset of anesthesia upon intravenous injection.[17] It also enables penetration through the blood-brain barrier and effective perfusion to the brain. However, the rapid redistribution of these agents from the brain to other muscle and fat tissues causes it to have a short duration of action. Adjuvant agents are typically administered in addition to sedative-hypnotic agents to supplement the induction of TIVA.[17]
Propofol
Propofol is usually the selected sedative-hypnotic agent to maintain general anesthesia through TIVA because of its rapid onset and offset, beneficial properties and few adverse effects.[35] Its rapid onset of action is due to its high lipid-solubility, rapid redistribution from the brain to other parts of the body, and rapid clearance (20 to 30 mL/kg/minute).[35] Most propofol is conjugated in the liver with pharmacologically inactive metabolites.[35] Although it has a long terminal elimination half-life of 4 to 30 hours, plasma concentrations remain low after the typical induction dose.[35]
Its advantages include “antiemetic, antipruritic, bronchodilatory, and anticonvulsant properties”,[36] which makes it suitable for patients with kidney or liver insufficiency.[37] Potential adverse effects of propofol include hypotension and respiratory depression caused by inadequate dosing, pain on injection, and risk of contamination.[38]
Etomidate
Etomidate is suitable for patients with hemodynamic instability since it does not compromise blood pressure, cardiac output, or heart rate.[39][40] Its advantages include anticonvulsant properties and hemodynamic stability. Potential adverse effects include a higher incidence of postoperative nausea and vomiting, transient acute adrenal insufficiency, pain during injection, involuntary myoclonic movements, absence of analgesic effects and mild increases in airway resistance.[39][41]
Ketamine
Ketamine is suitable for hypotensive patients, or patients with risks of developing hypotension (e.g. those who have hypovolemia, hemorrhage, sepsis or severe cardiovascular compromise).[42][43] This is because ketamine is associated with increased blood pressure, heart rate and cardiac output.[44] Its advantages include profound analgesic properties, bronchodilation, and the ability to maintain airway reflexes and respiratory drive.[45] It could also be induced via the intramuscular route if TIVA access gets lost. However, its potential adverse effects impact cardiovascular and neurological functions.
Potential adverse effects on cardiovascular activities are listed below:[46]
- Increase in myocardial oxygen demand due to a rise in heart rate, blood pressure and cardiac output
- Increase in pulmonary arterial pressure, which could be fatal in patients with ischemic heart disease, systemic or pulmonary hypertension
- Increase in the toxicity of cocaine and tricyclic antidepressants on cardiovascular structures
- Exacerbates hypertension, tachycardia arrhythmia in pheochromocytoma
- Though rare, direct mild myocardial depressant effects
Potential adverse effects on neurological activities are listed below:[46]
- Higher incidence of psychotomimetic effects
- Increase in cerebral blood flow and intracranial pressure, which may increase the cerebral metabolic rate of oxygen
- Unique EEG effects might lead to misinterpretation of processed EEG values
Adjuvant agents
Opioid, lidocaine and midazolam are adjuvant agents frequently administered to minimize pain during the injection of the induction agents.[47][48] They are also used to lessen the sympathetic stress response, cough reflex during laryngoscopy or intubation, and supplement sedation by synergistic effects.[49][50] The dose of sedative-hypnotic agents should be reduced due to the synergistic effects when combined with adjuvant agents.[50]
Choice of specific adjuvant agents is dependent upon the patient and procedure-specific factors.[51] Opioid is a commonly administered adjuvant agent as the analgesic component of TIVA. However, when used with propofol, it might exacerbate the adverse hypotensive effects.[50] Other potential adverse effects include respiratory depression, bradycardia, delirium and potential for acute tolerance.[52]
Risks and complications
Accidental awareness during general anesthesia (AAGA)
Patients under TIVA have a higher risk of AAGA. Unlike inhaled anesthetic agents, intravenous agents do not have an indicative end-tidal anesthetic concentration (ETAC) for the monitoring of administered drugs, so the determination of successful delivery is usually left to the anesthetist's clinical judgment.[2]
The high incidence of AAGA with TIVA can be attributed to several factors. Firstly, the target concentration of anesthetic agents required to maintain unresponsiveness is not well understood.[2] Although there have been studies aiming to establish the target concentration of propofol, there is a high degree of variability with the established dosing range.[53] Secondly, intravenous delivery may be impaired by lax monitoring of the intravenous catheter and the insertion site.[2] Thirdly, the use of neuromuscular blockades is a risk factor of AAGA and also hinders communication of distress in the case of accidental awareness.[2]
Opioid-induced hyperalgesia
TIVA techniques which involve the continued administration of opioids (E.g. Remifentanil) at high doses can cause opioid-induced hyperalgesia.[54] This may lead to difficult postoperative pain control, as patients with hyperalgesia experience increased chronic pain and require more analgesics following surgery.[53]
Neurotoxicity
Prolonged anesthetic exposure can result in the death of neural cells and defective synaptogenesis,[55] caused by increased expression of neurologically harmful substances.[2] The resulting neurologic injuries may lead to a persistent subtle decline of cognitive abilities, especially in elderly or very young patients.[2] Animal studies suggest that propofol may have similar neurotoxic properties as it is associated with apoptotic degeneration of oligodendrocytes.[2]
Special populations
Obese patients
Obese patients present technical and physiological challenges to TIVA. Physical tasks such as surgical positioning, intravenous insertion and ventilation are complicated by excess fat.[56] Associated physiological and pharmacological changes include higher susceptibility to hypoxemia, decrease in resting metabolic rate and lower cardiac output per kg body weight.[57] The use of dosing models derived from non-obese patients is therefore unsuitable for obese patients.[58]
Even within the obese population, the large variability between individuals limits the accuracy of pharmacokinetic models in predicting and informing anesthetic titration.[56]
Pediatrics
Infants differ from adults in the consideration of pharmacokinetics, pharmacodynamics and side effects.[59] In terms of pharmacokinetics, protein binding, organ function and body composition are significantly different.[60] Pharmacodynamic effects such as the capacity of target organs to respond to drugs are also changed.[59] Based on this knowledge, doses are adjusted to achieve optimal clinical response and avoid toxicity in pediatric patients.[61] Generally, clearance (drug elimination from the body) is greater in children due to the nonlinear scaling between body size and function.[59]
Elderly patients
Aging is associated with an increase in fat and a reduction in lean body mass and total body water.[62] These factors increase the volume of distribution of lipid-soluble drugs, lower their plasma concentration and delay elimination.[63] Aged patients typically have a higher sensitivity to drug action due to a reduction in the initial drug clearance, resulting in higher plasma concentration and hence greater initial drug effect..[63]
References
- Sear, John William (2017), "When and How Did It All Begin? A Brief History of Intravenous Anesthesia", Total Intravenous Anesthesia and Target Controlled Infusions, Cham: Springer International Publishing, pp. 3–8, doi:10.1007/978-3-319-47609-4_1, ISBN 978-3-319-47607-0, retrieved 2021-04-01
- Johnson, Ken B. (2017), "Advantages, Disadvantages, and Risks of TIVA/TCI", Total Intravenous Anesthesia and Target Controlled Infusions, Cham: Springer International Publishing, pp. 621–631, doi:10.1007/978-3-319-47609-4_32, ISBN 978-3-319-47607-0, retrieved 2021-04-01
- Kissin, Igor; Wright, A.J. (1988-08-01). "The Introduction of Hedonal". Anesthesiology. 69 (2): 242–245. doi:10.1097/00000542-198808000-00014. ISSN 0003-3022. PMID 3044190. S2CID 39156836.
- NOEL, H.; SOUTTAR, H. S. (1913). "The Anaesthetic Effects of the Intravenous Injection of Paraldehyde". Annals of Surgery. 57 (1): 64–67. doi:10.1097/00000658-191301000-00004. ISSN 0003-4932. PMC 1407440. PMID 17862957.
- PECK, CHARLES H. (1916-10-14). "Anesthesia in Human Beings by Intravenous Injection of Magnesium Sulphate". Journal of the American Medical Association. LXVII (16): 1131. doi:10.1001/jama.1916.02590160009004. ISSN 0002-9955.
- Naragawa, Koshiro (1921). "Experimentelle Studien über die intravenöse Infusionsnarkose mittels Alkohols". The Tohoku Journal of Experimental Medicine. 2 (1): 81–126. doi:10.1620/tjem.2.81. ISSN 1349-3329.
- James, Roger; Glen, John B. (1980). "Synthesis, biological evaluation, and preliminary structure-activity considerations of a series of alkylphenols as intravenous anesthetic agents". Journal of Medicinal Chemistry. 23 (12): 1350–1357. doi:10.1021/jm00186a013. ISSN 0022-2623.
- CUMMINGS, G. C.; DIXON, J.; KAY, N. H.; WINDSOR, J. P. W.; MAJOR, E.; MORGAN, M.; SEAR, J. W.; SPENCE, A. A.; STEPHENSON, D. K. (1984). "Dose requirements of ICI 35,868 (Propofol, 'Diprivan') in a new formulation for induction of anaesthesia". Anaesthesia. 39 (12): 1168–1171. doi:10.1111/j.1365-2044.1984.tb06425.x. ISSN 0003-2409. PMID 6335003. S2CID 26653276.
- Murray, W. B. (2009-11-01). "Provider Needs for Distributed Simulation Education System in Total Intravenous Anesthesia and Target Controlled Infusion". Fort Belvoir, VA. doi:10.21236/ada542258.
{{cite journal}}: Cite journal requires|journal=(help) - van den Berg, J.P.; Vereecke, H.E.M.; Proost, J.H.; Eleveld, D.J.; Wietasch, J.K.G.; Absalom, A.R.; Struys, M.M.R.F. (2017). "Pharmacokinetic and pharmacodynamic interactions in anaesthesia. A review of current knowledge and how it can be used to optimize anaesthetic drug administration". British Journal of Anaesthesia. 118 (1): 44–57. doi:10.1093/bja/aew312. ISSN 0007-0912. PMID 28039241.
- De Jong, Audrey; Verzilli, Daniel; Geniez, Marie; Chanques, Gérald; Nocca, David; Jaber, Samir (May 2018). "Pourquoi le patient obèse morbide est-il un patient à risque anesthésique élevé ?". La Presse Médicale (in French). 47 (5): 453–463. doi:10.1016/j.lpm.2018.01.016. PMID 29609909.
- De Jong, Audrey; Rollé, Amélie; Souche, François-Régis; Yengui, Olfa; Verzilli, Daniel; Chanques, Gérald; Nocca, David; Futier, Emmanuel; Jaber, Samir (April 2020). "How can I manage anaesthesia in obese patients?". Anaesthesia Critical Care & Pain Medicine. 39 (2): 229–238. doi:10.1016/j.accpm.2019.12.009. PMID 32068132. S2CID 211159649.
- Yuill, Gordon; Simpson, Milda (2002). "An introduction to total intravenous anaesthesia". BJA CEPD Reviews. 2 (1): 24–26. doi:10.1093/bjacepd/2.1.24. ISSN 1472-2615.
- Engbers, Frank H. M. (2000), "Total Intravenous Anaesthesia: The Equipment", On the Study and Practice of Intravenous Anaesthesia, Dordrecht: Springer Netherlands, pp. 71–87, doi:10.1007/978-94-015-9604-6_6, ISBN 978-90-481-5366-4, retrieved 2021-04-01
- Smith, Ian (2003). "Total Intravenous Anaesthesia: Is it Worth the Cost?". CNS Drugs. 17 (9): 609–619. doi:10.2165/00023210-200317090-00001. ISSN 1172-7047. PMID 12828497. S2CID 53919586.
- Reekers, Marije; Boer, Fred; Vuyk, Jaap (2003), "Basic Concepts of Recirculatory Pharmacokinetic Modelling", Advances in Modelling and Clinical Application of Intravenous Anaesthesia, Boston, MA: Springer US, vol. 523, pp. 19–26, doi:10.1007/978-1-4419-9192-8_2, ISBN 978-1-4613-4830-6, PMID 15088836, retrieved 2021-04-01
- Garcia, Paul; Whalin, Matthew Keith; Sebel, Peter S. (2013), "Intravenous Anesthetics", Pharmacology and Physiology for Anesthesia, Elsevier, pp. 137–158, doi:10.1016/b978-1-4377-1679-5.00009-0, ISBN 978-1-4377-1679-5, retrieved 2021-04-01
- Prabhakar, Amit; Lambert, Todd; Kaye, Rachel J.; Gaignard, Scott M.; Ragusa, Joseph; Wheat, Shannon; Moll, Vanessa; Cornett, Elyse M.; Urman, Richard D.; Kaye, Alan David (December 2019). "Adjuvants in clinical regional anesthesia practice: A comprehensive review". Best Practice & Research Clinical Anaesthesiology. 33 (4): 415–423. doi:10.1016/j.bpa.2019.06.001. PMID 31791560. S2CID 208611069.
- Hendrickx, Jan F. A.; Eger, Edmond I; Sonner, James M.; Shafer, Steven L. (August 2008). "Is Synergy the Rule? A Review of Anesthetic Interactions Producing Hypnosis and Immobility". Anesthesia & Analgesia. 107 (2): 494–506. doi:10.1213/ane.0b013e31817b859e. ISSN 0003-2999. PMID 18633028. S2CID 8125002.
- Bowdle, T. Andrew (2009), "Can We Prevent Recall during Anesthesia?", Evidence-Based Practice of Anesthesiology, Elsevier, pp. 291–295, doi:10.1016/b978-1-4160-5996-7.00043-2, ISBN 978-1-4160-5996-7, retrieved 2021-04-01
- Jäntti, Ville; Sloan, Tod B. (2008), "EEG and anesthetic effects", Intraoperative Monitoring of Neural Function, Elsevier, pp. 77–93, doi:10.1016/s1567-4231(07)08004-5, ISBN 978-0-444-51824-8, retrieved 2021-04-01
- Hendrickx, Jan F. A.; Eger, Edmond I; Sonner, James M.; Shafer, Steven L. (2008). "Is Synergy the Rule? A Review of Anesthetic Interactions Producing Hypnosis and Immobility". Anesthesia & Analgesia. 107 (2): 494–506. doi:10.1213/ane.0b013e31817b859e. ISSN 0003-2999. PMID 18633028. S2CID 8125002.
- MacCallum, Caroline A.; Russo, Ethan B. (2018-03-01). "Practical considerations in medical cannabis administration and dosing". European Journal of Internal Medicine. 49: 12–19. doi:10.1016/j.ejim.2018.01.004. ISSN 0953-6205. PMID 29307505.
- Nimmo, A. F.; Absalom, A. R.; Bagshaw, O.; Biswas, A.; Cook, T. M.; Costello, A.; Grimes, S.; Mulvey, D.; Shinde, S.; Whitehouse, T.; Wiles, M. D. (2018-10-31). "Guidelines for the safe practice of total intravenous anaesthesia (TIVA)". Anaesthesia. 74 (2): 211–224. doi:10.1111/anae.14428. ISSN 0003-2409. PMID 30378102. S2CID 53107969.
- Ohashi, Kumiko; Dalleur, Olivia; Dykes, Patricia C.; Bates, David W. (2014-10-08). "Benefits and Risks of Using Smart Pumps to Reduce Medication Error Rates: A Systematic Review". Drug Safety. 37 (12): 1011–1020. doi:10.1007/s40264-014-0232-1. ISSN 0114-5916. PMID 25294653. S2CID 9308973.
- Kan, Karen; Levine, Wilton C. (2021-01-01). "Infusion Pumps". Anesthesia Equipment: 351–367. doi:10.1016/B978-0-323-67279-5.00016-9. ISBN 9780323672795. S2CID 243158761.
- Seo, Kwang-Suk; Lee, Kiyoung (2016). "Smart syringe pumps for drug infusion during dental intravenous sedation". Journal of Dental Anesthesia and Pain Medicine. 16 (3): 165–173. doi:10.17245/jdapm.2016.16.3.165. ISSN 2383-9309. PMC 5586553. PMID 28884149.
- Alexovič, Michal; Horstkotte, Burkhard; Šrámková, Ivana; Solich, Petr; Sabo, Ján (2017-01-01). "Automation of dispersive liquid–liquid microextraction and related techniques. Approaches based on flow, batch, flow-batch and in-syringe modes". TrAC Trends in Analytical Chemistry. 86: 39–55. doi:10.1016/j.trac.2016.10.003. ISSN 0165-9936.
- Absalom, Anthony R.; Glen, John (Iain) B.; Zwart, Gerrit J. C.; Schnider, Thomas W.; Struys, Michel M. R. F. (2016). "Target-Controlled Infusion". Anesthesia & Analgesia. 122 (1): 70–78. doi:10.1213/ane.0000000000001009. ISSN 0003-2999. PMID 26516798. S2CID 41023659.
- Struys, Michel M. R. F.; De Smet, Tom; Glen, John (Iain) B.; Vereecke, Hugo E. M.; Absalom, Anthony R.; Schnider, Thomas W. (2016). "The History of Target-Controlled Infusion". Anesthesia & Analgesia. 122 (1): 56–69. doi:10.1213/ane.0000000000001008. ISSN 0003-2999. PMID 26516804. S2CID 39391491.
- Morton, Neil S. (2012-12-18). "Total Intravenous Anesthesia (TIVA) and Target Controlled Infusions (TCI) in Children". Current Anesthesiology Reports. 3 (1): 37–41. doi:10.1007/s40140-012-0005-2. ISSN 2167-6275.
- Schnider, Thomas W.; Minto, Charles F.; Struys, Michel M. R. F.; Absalom, Anthony R. (2016). "The Safety of Target-Controlled Infusions". Anesthesia & Analgesia. 122 (1): 79–85. doi:10.1213/ane.0000000000001005. ISSN 0003-2999. S2CID 25742249.
- "Correspondence". Anaesthesia and Intensive Care. 30 (6): 813–818. 2002. doi:10.1177/0310057x0203000618. ISSN 0310-057X.
- Hendrickx, Jan F. A.; Eger, Edmond I; Sonner, James M.; Shafer, Steven L. (2008). "Is Synergy the Rule? A Review of Anesthetic Interactions Producing Hypnosis and Immobility". Anesthesia & Analgesia. 107 (2): 494–506. doi:10.1213/ane.0b013e31817b859e. ISSN 0003-2999. PMID 18633028. S2CID 8125002.
- McGrenaghan, Eoghan; Wilson, Ming (2019). "Total intravenous anaesthesia". Anaesthesia & Intensive Care Medicine. 20 (2): 130–135. doi:10.1016/j.mpaic.2018.12.010. ISSN 1472-0299. S2CID 81449338.
- Shafer, Steven L. (1993). "Advances in propofol pharmacokinetics and pharmacodynamics". Journal of Clinical Anesthesia. 5 (6): 14–21. doi:10.1016/0952-8180(93)90003-w. ISSN 0952-8180. PMID 8292364.
- Gray, P. A.; Park, G. R.; Cockshott, I. D.; Douglas, E. J.; Shuker, B.; Simons, P. J. (1992). "Propofol metabolism in man during the anhepatic and reperfusion phases of liver transplantation". Xenobiotica. 22 (1): 105–114. doi:10.3109/00498259209053107. ISSN 0049-8254. PMID 1615701.
- Yeoh, Chuen Jye; Hwang, Nian Chih (2020). "Volatile Anesthesia Versus Total Intravenous Anesthesia During Cardiopulmonary Bypass: A Narrative Review on the Technical Challenges and Considerations". Journal of Cardiothoracic and Vascular Anesthesia. 34 (8): 2181–2188. doi:10.1053/j.jvca.2020.03.013. ISSN 1053-0770. S2CID 216248614.
- Hulsman, N.; Hollmann, M.W.; Preckel, B. (2018). "Newer propofol, ketamine, and etomidate derivatives and delivery systems relevant to anesthesia practice". Best Practice & Research Clinical Anaesthesiology. 32 (2): 213–221. doi:10.1016/j.bpa.2018.08.002. ISSN 1521-6896. PMID 30322461. S2CID 53503078.
- Forman, Stuart A.; Warner, David S. (2011-03-01). "Clinical and Molecular Pharmacology of Etomidate". Anesthesiology. 114 (3): 695–707. doi:10.1097/aln.0b013e3181ff72b5. ISSN 0003-3022. PMC 3108152. PMID 21263301.
- Hohl, Corinne M.; Kelly-Smith, Carolyn H.; Yeung, Titus C.; Sweet, David D.; Doyle-Waters, Mary M.; Schulzer, Michael (2010). "The Effect of a Bolus Dose of Etomidate on Cortisol Levels, Mortality, and Health Services Utilization: A Systematic Review". Annals of Emergency Medicine. 56 (2): 105–113.e5. doi:10.1016/j.annemergmed.2010.01.030. ISSN 0196-0644. PMID 20346542.
- Schwenk, Eric S.; Viscusi, Eugene R.; Buvanendran, Asokumar; Hurley, Robert W.; Wasan, Ajay D.; Narouze, Samer; Bhatia, Anuj; Davis, Fred N.; Hooten, William M.; Cohen, Steven P. (2018). "Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Acute Pain Management From the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists". Regional Anesthesia and Pain Medicine. 43 (5): 456–466. doi:10.1097/aap.0000000000000806. ISSN 1098-7339. PMC 6023582. PMID 29870457.
- Morris, C.; Perris, A.; Klein, J.; Mahoney, P. (2009). "Anaesthesia in haemodynamically compromised emergency patients: does ketamine represent the best choice of induction agent?". Anaesthesia. 64 (5): 532–539. doi:10.1111/j.1365-2044.2008.05835.x. ISSN 0003-2409. S2CID 16287093.
- Zhou, Jon Y.; Hamilton, Perry; Macres, Stephen; Peña, Matthew; Tang, Schirin (2020). "Update on Ketamine". Advances in Anesthesia. 38: 97–113. doi:10.1016/j.aan.2020.07.005. ISSN 0737-6146. PMID 34106842. S2CID 224909438.
- Rascón-Martínez, D.M.; Carrillo-Torres, O.; Ramos-Nataren, R.G.; Rendón-Jaramillo, L. (2018). "Advantages of ketamine as a perioperative analgesic". Revista Médica del Hospital General de México. 81 (4): 253–261. doi:10.1016/j.hgmx.2016.10.007. ISSN 0185-1063.
- Hudetz, Judith A.; Pagel, Paul S. (2010). "Neuroprotection by Ketamine: A Review of the Experimental and Clinical Evidence". Journal of Cardiothoracic and Vascular Anesthesia. 24 (1): 131–142. doi:10.1053/j.jvca.2009.05.008. ISSN 1053-0770. PMID 19640746.
- Prabhakar, Hemanshu (28 March 2017). Essentials of neuroanesthesia. ISBN 978-0-12-805299-0. OCLC 959033559.
- Reves, J.G.; Fragen, Robert; Vinik, Ronald; Greenblatt, David (1985). "Midazolam". Anesthesiology. 62 (3): 310–324. doi:10.1097/00000542-198503000-00017. ISSN 0003-3022. S2CID 28308031.
- Shaban, Amira A. (2016). "Effect of small dose propofol or midazolam to prevent laryngospasm and coughing following oropharyngeal surgeries: Randomized controlled trial". Egyptian Journal of Anaesthesia. 32 (1): 13–19. doi:10.1016/j.egja.2015.09.008. ISSN 1110-1849.
- Marinella, M.A. (October 1997). "Propofol for sedation in the intensive care unit: essentials for the clinician". Respiratory Medicine. 91 (9): 505–510. doi:10.1016/s0954-6111(97)90082-2. ISSN 0954-6111. PMID 9415349.
- Winacoo, Jeffrey; Maykel, Justin (2009). "Operative Anesthesia and Pain Control". Clinics in Colon and Rectal Surgery. 22 (1): 041–046. doi:10.1055/s-0029-1202885. ISSN 1531-0043. PMC 2780232. PMID 20119555.
- Warner, Louise O.; Balch, Daniel R.; Davidson, Patricia J. (1997). "Is intravenous lidocaine an effective adjuvant for endotracheal intubation in children undergoing induction of anesthesia with halothane-nitrous oxide?". Journal of Clinical Anesthesia. 9 (4): 270–274. doi:10.1016/s0952-8180(97)00003-2. ISSN 0952-8180. PMID 9195347.
- Reves, J.G.; Glass, Peter S.A.; Lubarsky, David A.; McEvoy, Matthew D.; Martinez-Ruiz, Ricardo (2010), "Intravenous Anesthetics", Miller's Anesthesia, Elsevier, pp. 719–768, doi:10.1016/b978-0-443-06959-8.00026-1, ISBN 978-0-443-06959-8, retrieved 2021-04-01
- Hayhurst, Christina J.; Durieux, Marcel E. (2016-02-01). "Differential Opioid Tolerance and Opioid-induced Hyperalgesia". Anesthesiology. 124 (2): 483–488. doi:10.1097/aln.0000000000000963. ISSN 0003-3022. PMID 26594912.
- Creeley, Catherine E.; Olney, John W. (2010). "The Young: Neuroapoptosis Induced by Anesthetics and What to Do About It". Anesthesia & Analgesia. 110 (2): 442–448. doi:10.1213/ANE.0b013e3181c6b9ca. ISSN 0003-2999. PMID 19955510. S2CID 14304084.
- Sepúlveda V., Pablo O.; Cortínez, Luis Ignacio (2017), "Intravenous Anesthesia in Obese Patients", Total Intravenous Anesthesia and Target Controlled Infusions, Cham: Springer International Publishing, pp. 429–440, doi:10.1007/978-3-319-47609-4_24, ISBN 978-3-319-47607-0, retrieved 2021-04-13
- Cheymol, Georges (2000). "Effects of Obesity on Pharmacokinetics". Clinical Pharmacokinetics. 39 (3): 215–231. doi:10.2165/00003088-200039030-00004. ISSN 0312-5963. PMID 11020136. S2CID 20056863.
- Eleveld, Douglas J.; Proost, Johannes H.; Absalom, Anthony R.; Struys, Michel M.R.F. (2011). "Obesity and Allometric Scaling of Pharmacokinetics". Clinical Pharmacokinetics. 50 (11): 751–753. doi:10.2165/11594080-000000000-00000. ISSN 0312-5963. PMID 21973272. S2CID 41800410.
- Anderson, Brian J. (2017), "Pharmacokinetics and Pharmacodynamics in the Pediatric Patient", Total Intravenous Anesthesia and Target Controlled Infusions, Cham: Springer International Publishing, pp. 441–516, doi:10.1007/978-3-319-47609-4_25, ISBN 978-3-319-47607-0, retrieved 2021-04-13
- Kearns, Gregory L.; Abdel-Rahman, Susan M.; Alander, Sarah W.; Blowey, Douglas L.; Leeder, J. Steven; Kauffman, Ralph E. (2003-09-18). "Developmental Pharmacology — Drug Disposition, Action, and Therapy in Infants and Children". New England Journal of Medicine. 349 (12): 1157–1167. doi:10.1056/nejmra035092. ISSN 0028-4793. PMID 13679531.
- Anderson, B. J.; Holford, N. H. G. (2013-07-05). "Understanding dosing: children are small adults, neonates are immature children". Archives of Disease in Childhood. 98 (9): 737–744. doi:10.1136/archdischild-2013-303720. ISSN 0003-9888. PMID 23832061. S2CID 31723102.
- Hughes, Virginia A; Frontera, Walter R; Roubenoff, Ronenn; Evans, William J; Singh, Maria A Fiatarone (2002-08-01). "Longitudinal changes in body composition in older men and women: role of body weight change and physical activity". The American Journal of Clinical Nutrition. 76 (2): 473–481. doi:10.1093/ajcn/76.2.473. ISSN 0002-9165. PMID 12145025.
- Servin, Frederique S. (2017), "TCI in Special Patients Groups: The Elderly and Obese", Total Intravenous Anesthesia and Target Controlled Infusions, Cham: Springer International Publishing, pp. 571–578, doi:10.1007/978-3-319-47609-4_29, ISBN 978-3-319-47607-0, retrieved 2021-04-13