Vaginismus
Vaginismus is a condition in which involuntary muscle spasm interferes with vaginal intercourse or other penetration of the vagina.[2] This often results in pain with attempts at sex.[2] Often, it begins when vaginal intercourse is first attempted.[3]
| Vaginismus | |
|---|---|
| Other names | Vaginism, genito-pelvic pain disorder[1] |
 | |
| Muscles included | |
| Specialty | Gynecology |
| Symptoms | Pain with sex[2] |
| Usual onset | With first sexual intercourse[3] |
| Causes | Fear of pain[3] |
| Risk factors | History of sexual assault, endometriosis, vaginitis, prior episiotomy[2] |
| Diagnostic method | Based on the symptoms and examination[2] |
| Differential diagnosis | Dyspareunia[4] |
| Treatment | Behavior therapy, gradual vaginal dilatation[2] |
| Prognosis | Generally good with treatment[5] |
| Frequency | 0.5% of women[2] |
The formal diagnostic criteria specifically requires interference during vaginal intercourse and a desire for intercourse. However, the term vaginismus is sometimes used more broadly to refer to any muscle spasms occurring during the insertion of some or all types of objects into the vagina, sexually motivated or otherwise, including the usage of speculums and tampons.[5][6]
The underlying cause is generally a fear that penetration will hurt.[3] Risk factors include a history of sexual assault, endometriosis, vaginitis, or a prior episiotomy.[2] Diagnosis is based on the symptoms and examination.[2] It requires there to be no anatomical or physical problems and a desire for penetration on the part of the woman.[3][7]
Treatment may include behavior therapy such as graduated exposure therapy and gradual vaginal dilatation.[2][3] Surgery is not generally indicated.[5] Botulinum toxin (botox), a muscle spasm treatment, is being studied.[2] Estimates of how common the condition is vary.[8] One textbook estimates that 0.5% of women are affected.[2] Outcomes are generally good with treatment.[5]
Causes
Primary vaginismus
Vaginismus occurs when penetrative sex or other vaginal penetration cannot be experienced without pain. It is commonly discovered among teenage girls and women in their early twenties, as this is when many girls and young women first attempt to use tampons, have penetrative sex, or undergo a Pap smear. Awareness of vaginismus may not happen until vaginal penetration is attempted. Reasons for the condition may be unknown.[11]
A few of the main factors that may contribute to primary vaginismus include:
- chronic pain conditions and harm-avoidance behaviour[12]
- negative emotional reaction towards sexual stimulation, e.g. disgust both at a deliberate level and also at a more implicit level[13]
- strict conservative moral education, which also can elicit negative emotions[14]
Primary vaginismus is often unknown cause.[15]
Vaginismus has been classified by Lamont[16] according to the severity of the condition. Lamont describes four degrees of vaginismus: In first degree vaginismus, the person has spasm of the pelvic floor that can be relieved with reassurance. In second degree, the spasm is present but maintained throughout the pelvis even with reassurance. In third degree, the person elevates the buttocks to avoid being examined. In fourth degree vaginismus (also known as grade 4 vaginismus), the most severe form of vaginismus, the person elevates the buttocks, retreats and tightly closes the thighs to avoid examination. Pacik expanded the Lamont classification to include a fifth degree in which the person experiences a visceral reaction such as sweating, hyperventilation, palpitations, trembling, shaking, nausea, vomiting, losing consciousness, wanting to jump off the table, or attacking the doctor.[17]
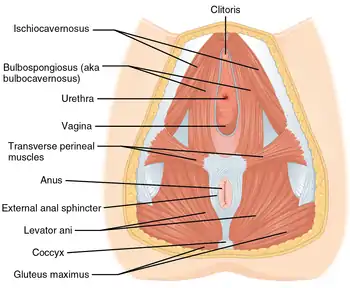
Although the pubococcygeus muscle is commonly thought to be the primary muscle involved in vaginismus, Pacik identified two additionally-involved spastic muscles in people who were treated under sedation. These include the entry muscle (bulbocavernosum) and the mid-vaginal muscle (puborectalis). Spasm of the entry muscle accounts for the common complaint that people often report when trying to have intercourse: "It's like hitting a brick wall".[11]
Secondary vaginismus
Secondary vaginismus occurs when a person who has previously been able to achieve penetration develops vaginismus. This may be due to physical causes such as a yeast infection or trauma during childbirth, while in some cases it may be due to psychological causes, or to a combination of causes. The treatment for secondary vaginismus is the same as for primary vaginismus, although, in these cases, previous experience with successful penetration can assist in a more rapid resolution of the condition. Peri-menopausal and menopausal vaginismus, often due to a drying of the vulvar and vaginal tissues as a result of reduced estrogen, may occur as a result of "micro-tears" first causing sexual pain then leading to vaginismus.[18]
Mechanism
Specific muscle involvement is unclear, but the condition may involve the pubococcygeus muscle, levator ani, bulbocavernosus, circumvaginal, or perivaginal muscles.[8]
Diagnosis
The diagnosis of vaginismus, as well as other diagnoses of female sexual dysfunction, can be made when "symptoms are sufficient to result in personal distress."[19] The DSM-IV-TR defines vaginismus as "recurrent or persistent involuntary spasm of the musculature of the outer third of the vagina that interferes with sexual intercourse, causing marked distress or interpersonal difficulty".[19]
Treatment
A Cochrane review found little high quality evidence regarding the treatment of vaginismus in 2012.[20] Specifically it is unclear if systematic desensitisation is better than other measures including nothing.[20]
Psychological
According to a 2011 study, those with vaginismus are twice as likely to have a history of childhood sexual interference and held less positive attitudes about their sexuality, whereas no correlation was noted for lack of sexual knowledge or (nonsexual) physical abuse.[21]
Physical

Often, when faced with a person experiencing painful intercourse, a gynecologist will recommend reverse Kegel exercises and provide some additional lubricants.[22][23][24][25] Although vaginismus has not been shown to affect a person's ability to produce lubrication, providing additional lubricant can be helpful in achieving successful penetration. This is due to the fact that women may not produce natural lubrication if anxious or in pain. Achieving sufficient arousal during foreplay is crucial for the release of lubrication which can contribute to the ease of sexual penetration and pain-free intercourse.
Though strengthening exercises such as Kegel exercises were previously considered to be a helpful intervention for pelvic pain, new research suggests that these exercises, which function to strengthen the pelvic floor, may not be helpful or may make conditions that are caused by over-active muscles such as vaginismus worse. Exercises that stretch or relax the pelvic floor may be a better treatment option for vaginismus.[26][27][28]
To help develop a treatment plan that best fits the needs of their patient, a gynecologist or general practitioner may refer a person experiencing painful intercourse to a Pelvic floor physical therapist or occupational therapist. These therapists specialize in the treatment of disorders of the pelvic floor muscles such as vaginismus, dyspareunia, vulvodynia, constipation, and fecal or urinary incontinence.[27][28] After performing a manual exam both internally and externally to assess muscle function and to isolate possible trigger points for pain or tightness on the muscles, pelvic floor physical or occupational therapists develop a treatment plan consisting of muscle exercises, muscle stretches, dilator training, electrostimulation, and/or biofeedback interventions.[27] Treatment of vaginismus often involves the use of Hegar dilators (sometimes called vaginal trainers), progressively increasing the size of the dilator inserted into the vagina. The technique is used to practice conscious diaphragmatic breathing (breathing in deeply allowing one's belly to expand) and allowing the pelvic floor muscles to lengthen during inhale; then exhale, bringing belly in and repeat.[29][30] Research suggests pelvic floor physical or occupational therapy is one of the safest and most effective treatments for vaginismus.[28]
Neuromodulators
Botulinum toxin A (Botox) has been considered as a treatment option, under the idea of temporarily reducing the hypertonicity of the pelvic floor muscles. Although no random controlled trials have been done with this treatment, experimental studies with small samples have shown it to be effective, with sustained positive results through 10 months.[8][31] Similar in its mechanism of treatment, lidocaine has also been tried as an experimental option.[8][32]
Anxiolytics and antidepressants are other pharmacotherapies that have been offered to people in conjunction with other psychotherapy modalities, or if these people's experience high levels of anxiety from their condition.[8] Evidence for these medications, however, is limited.[8]
Epidemiology
Estimates of how common the condition is varies.[8] A 2016 textbook estimated about 0.5% of women are affected,[2] while rates in Morocco and Sweden were estimated at 6%.[33]
Among those who attend clinics for sexual dysfunction, rates may be as high as 12 to 47%.[2][34]
See also
- Hymen
- Penis captivus
- Vulvodynia
References
- Maddux, James E.; Winstead, Barbara A. (2012). Psychopathology: Foundations for a Contemporary Understanding. Taylor & Francis. p. 332. ISBN 9781136482847.
- Ferri, Fred F. (2016). Ferri's Clinical Advisor 2017 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 1330. ISBN 9780323448383.
- "Vaginismus". Merck Manuals Professional Edition. April 2013. Archived from the original on 18 January 2021. Retrieved 15 October 2018.
- Domino, Frank J. (2010). The 5-Minute Clinical Consult 2011. Lippincott Williams & Wilkins. p. 1394. ISBN 9781608312597.
- "Vaginismus". NHS. 2018-01-11. Retrieved 15 October 2018.
- Nazario, Brunilda, MD. (2012). "Women's Health: Vaginismus". WebMD. Retrieved December 22, 2016.
- Braddom, Randall L. (2010). Physical Medicine and Rehabilitation E-Book. Elsevier Health Sciences. p. 665. ISBN 978-1437735635.
- Lahaie, MA; Boyer, SC; Amsel, R; Khalifé, S; Binik, YM (Sep 2010). "Vaginismus: a review of the literature on the classification/diagnosis, etiology and treatment". Women's Health. 6 (5): 705–19. doi:10.2217/whe.10.46. PMID 20887170.
- Reissing, Elke; Yitzchak Binik; Samir Khalife (May 1999). "Does Vaginismus Exist? A Critical Review of the Literature". The Journal of Nervous and Mental Disease. 187 (5): 261–274. doi:10.1097/00005053-199905000-00001. PMID 10348080.
- Katz, Ditza (2020). "Vaginismus: Symptoms, Causes & Treatment". Women's Therapy Center. Retrieved 2021-01-20.
{{cite web}}: CS1 maint: url-status (link) - Pacik PT (December 2009). "Botox treatment for vaginismus". Plast. Reconstr. Surg. 124 (6): 455e–6e. doi:10.1097/PRS.0b013e3181bf7f11. PMID 19952618.
- Borg, Charmaine; Peters, L. M.; Weijmar Schultz, W.; de Jong, P. J. (February 2012). "Vaginismus: Heightened Harm Avoidance and Pain Catastrophizing Cognitions". Journal of Sexual Medicine. 9 (2): 558–567. doi:10.1111/j.1743-6109.2011.02535.x. PMID 22024378.
- Borg, Charmaine; Peter J. De Jong; Willibrord Weijmar Schultz (June 2010). "Vaginismus and Dyspareunia: Automatic vs. Deliberate: Disgust Responsivity". Journal of Sexual Medicine. 7 (6): 2149–2157. doi:10.1111/j.1743-6109.2010.01800.x. PMID 20367766.
- Borg, Charmaine; Peter J. de Jong; Willibrord Weijmar Schultz (Jan 2011). "Vaginismus and Dyspareunia: Relationship with General and Sex-Related Moral Standards". Journal of Sexual Medicine. 8 (1): 223–231. doi:10.1111/j.1743-6109.2010.02080.x. PMID 20955317.
- "Vaginismus". Sexual Pain Disorders and Vaginismus. Armenian Medical Network. 2006. Retrieved 2008-01-07.
- Lamont, JA (1978). "Vaginismus". Am J Obstet Gynecol. 131 (6): 633–6. doi:10.1016/0002-9378(78)90822-0. PMID 686049.
- Pacik, PT.; Cole, JB. (2010). When Sex Seems Impossible. Stories of Vaginismus and How You Can Achieve Intimacy. Odyne Publishing. pp. 40–7.
- Pacik, Peter (2010). When Sex Seems Impossible. Stories of Vaginismus & How You Can Achieve Intimacy. Manchester, NH: Odyne. pp. 8–16. ISBN 978-0-9830134-0-2. Archived from the original on 2012-02-19. Retrieved 2011-12-29.
- American College of Obstetricians Gynecologists Committee on Practice Bulletins-Gynecology (April 2011). "Practice Bulletin No. 119: Female Sexual Dysfunction". Obstetrics & Gynecology. 117 (4): 996–1007. doi:10.1097/aog.0b013e31821921ce. ISSN 0029-7844. PMID 21422879.
- Melnik, T; Hawton, K; McGuire, H (12 December 2012). "Interventions for vaginismus". The Cochrane Database of Systematic Reviews. 12: CD001760. doi:10.1002/14651858.CD001760.pub2. PMC 7072531. PMID 23235583.
- Reissing ED, Binik YM, Khalifé S, Cohen D, Amsel R (2003). "Etiological correlates of vaginismus: sexual and physical abuse, sexual knowledge, sexual self-schema, and relationship adjustment". J Sex Marital Ther. 29 (1): 47–59. doi:10.1080/713847095. PMID 12519667. S2CID 46659017.
- "When sex hurts – vaginismus". The Society of Obstetricians and Gynecologists of Canada. n.d. Archived from the original on 2013-10-20.
- Herndon, Jaime (November 30, 2015). "Vaginismus". Healthline. George Kruick, MD. Retrieved December 22, 2016.
- Nazario, Brunilda, MD. (2012). "Women's Health: Vaginismus". WebMD. Retrieved December 22, 2016.
- "When sex gives more pain than pleasure". Harvard Health Publications. Harvard Health. May 2012. Retrieved December 22, 2016.
- Bradley, Michelle H.; Rawlins, Ashley; Brinker, C. Anna (August 2017). "Physical Therapy Treatment of Pelvic Pain". Physical Medicine and Rehabilitation Clinics of North America. 28 (3): 589–601. doi:10.1016/j.pmr.2017.03.009. PMID 28676366.
- Rosenbaum, Talli Yehuda (January 2007). "REVIEWS: Pelvic Floor Involvement in Male and Female Sexual Dysfunction and the Role of Pelvic Floor Rehabilitation in Treatment: A Literature Review". The Journal of Sexual Medicine. 4 (1): 4–13. doi:10.1111/j.1743-6109.2006.00393.x. PMID 17233772.
- Wallace, Shannon L.; Miller, Lucia D.; Mishra, Kavita (December 2019). "Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women". Current Opinion in Obstetrics and Gynecology. 31 (6): 485–493. doi:10.1097/GCO.0000000000000584. ISSN 1040-872X. PMID 31609735. S2CID 204703488.
- Doleys, Daniel (6 December 2012). Behavioral Medicine. Springer Science & Business Media. p. 377. ISBN 9781468440706.
- nhs, nhs (2015). "NHS Choices Vaginal Trainers to treat vaginismus". NHS Choices Vaginismus treatment. NHS.
- Pacik PT (2011). "Vaginismus: A Review of Current Concepts and Treatment using Botox Injections, Bupivacaine Injections and Progressive Dilation Under Anesthesia". Aesthetic Plastic Surgery Journal. 35 (6): 1160–1164. doi:10.1007/s00266-011-9737-5. PMID 21556985. S2CID 8754988.
- Melnik, T; Hawton, K; McGuire, H (Dec 12, 2012). "Interventions for vaginismus". The Cochrane Database of Systematic Reviews. 12: CD001760. doi:10.1002/14651858.CD001760.pub2. PMC 7072531. PMID 23235583.
- Lewis RW, Fugl-Meyer KS, Bosch R, et al. (July 2004). "Epidemiology/risk factors of sexual dysfunction". J Sex Med. 1 (1): 35–9. CiteSeerX 10.1.1.565.3552. doi:10.1111/j.1743-6109.2004.10106.x. PMID 16422981.
- Reissing ED, Binik YM, Khalifé S (May 1999). "Does vaginismus exist? A critical review of the literature". J. Nerv. Ment. Dis. 187 (5): 261–74. doi:10.1097/00005053-199905000-00001. PMID 10348080.