Zolpidem
Zolpidem, sold under the brand name Ambien, among others, is a medication primarily used for the short-term treatment of sleeping problems.[8][10] Guidelines recommend that it be used only after cognitive behavioral therapy for insomnia and behavioral changes, such as sleep hygiene, have been tried.[11][12][13] It decreases the time to sleep onset by about fifteen minutes and at larger doses helps people stay asleep longer.[5] It is taken by mouth and is available in conventional tablets, sublingual tablets, or oral spray.[8]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Ambien and Ambien CR, Stilnox, others[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a693025 |
| Pregnancy category |
|
| Dependence liability | Moderate[3] |
| Routes of administration | By mouth (tablet), sublingual, oromucosal (spray), rectal |
| Drug class | Nonbenzodiazepine, sedative-hypnotic |
| ATC code |
|
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 70% (by mouth) |
| Protein binding | 92% |
| Metabolism | Liver through CYP3A4 (~60%), CYP2C9 (~20%), and CYP1A2 (~14%)[7] |
| Metabolites | (ZCA) zolpidem 6-carboxylic acid; (ZPCA) zolpidem phenyl-4-carboxylic acid |
| Onset of action | ≤ 30 Minutes |
| Elimination half-life | 2.0 - 3 hours[8][9] |
| Duration of action | 3 hours |
| Excretion | Kidney (56%) fecal (34%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.115.604 |
| Chemical and physical data | |
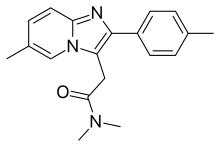
| Formula | C19H21N3O |
| Molar mass | 307.397 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| | |
Common side effects include daytime sleepiness, headache, nausea, and diarrhea.[8] More severe side effects include memory problems and hallucinations.[5] The previously recommended dose was decreased in 2013, by the US Food and Drug Administration (FDA), to the immediate-release 10 mg for men, and 5 mg for women, in an attempt to reduce next-day somnolence.[14] Newer extended-release formulations include the 6.25 mg for women, and 12.5 mg or 6.25 mg for men, which also cause next-day somnolence when used in higher doses. Additionally, driving the next morning is not recommended with either higher doses or the long-acting formulation.[14] While flumazenil, a GABAA–receptor antagonist, can reverse zolpidem's effects, usually supportive care is all that is recommended in overdose.[15]
Zolpidem is a nonbenzodiazepine which acts as a sedative and hypnotic.[8][15] Zolpidem is a GABAA receptor agonist of the imidazopyridine class.[8] It works by increasing GABA effects in the central nervous system by binding to GABAA receptors at the same location as benzodiazepines.[8] It generally has a half-life of two to three hours.[8] This, however, is increased in those with liver problems.[8]
Zolpidem was approved for medical use in the United States in 1992.[8][16] It became available as a generic medication in 2007.[17] Zolpidem is a Schedule IV controlled substance under the Controlled Substances Act of 1970 (CSA).[5][6] More than ten million prescriptions are filled each year in the United States, making it one of the most commonly used treatments for sleeping problems.[18][19] In 2020, it was the 47th most commonly prescribed medication in the United States, with more than 14 million prescriptions.[20][21]
Medical uses

Zolpidem is labelled for short-term (usually about two to six weeks) treatment of insomnia at the lowest possible dose.[8][10] It may be used for both improving sleep onset, sleep onset latency, and staying asleep.[5]
Guidelines from NICE, the European Sleep Research Society, and the American College of Physicians recommend medication for insomnia (including possibly zolpidem) only as a second line treatment after non-pharmacological treatment options have been tried (e.g. cognitive behavioral therapy for insomnia).[11][12][13] This is based in part on a 2012 review which found that zolpidem's effectiveness is nearly as much due to psychological effects as to the medication itself.[22]
A lower-dose version (3.5 mg for men and 1.75 mg for women) is given as a tablet under the tongue and used for middle-of-the-night awakenings. It can be taken if there are at least 4 hours between the time of administration and when the person must be awake.[23]
Contraindications
Zolpidem should not be taken by people with obstructive sleep apnea, myasthenia gravis, severe liver disease, respiratory depression; or by children, or people with psychotic illnesses. It should not be taken by people who are or have been addicted to other substances.[10]
Use of zolpidem may impair driving skills with a resultant increased risk of road traffic accidents. This adverse effect is not unique to zolpidem, but also occurs with other hypnotic drugs. Caution should be exercised by motor vehicle drivers.[10] In 2013, the FDA recommended the dose for women be reduced and that prescribers should consider lower doses for men due to impaired function the day after taking the drug.[24][25]
Zolpidem should not be prescribed to older people, who are more sensitive to the effects of hypnotics including zolpidem and are at an increased risk of falls and adverse cognitive effects, such as delirium and neurocognitive disorder.[26][27]
Zolpidem has not been assigned to a pregnancy category by the FDA.[2] Animal studies have revealed evidence of incomplete ossification and increased intrauterine fetal death at doses greater than seven times the maximum recommended human dose or higher; however, teratogenicity was not observed at any dose level. There are no controlled data in human pregnancy. In one case report, zolpidem was found in cord blood at delivery. Zolpidem is recommended for use during pregnancy only when benefits outweigh risks.[28]
Adverse effects

The most common adverse effects of short-term use include headache (reported by 7% of people in clinical trials), drowsiness (2%), dizziness (1%), and diarrhea (1%); the most common side effects of long-term use included drowsiness (8%), dizziness (5%), allergy (4%), sinusitis (4%), back pain (3%), diarrhea (3%), drugged feeling (3%), dry mouth (3%), lethargy (3%), sore throat (3%), abdominal pain (2%), constipation (2%), heart palpitations (2%), lightheadedness (2%), rash (2%), abnormal dreams (1%), amnesia (1%), chest pain (1%), depression (1%), flu-like symptoms (1%), and sleep disorder (1%).[6]
Zolpidem increases risk of depression, falls and bone fracture, poor driving, suppressed respiration, and has been associated with an increased risk of death.[29] Upper and lower respiratory infections are also common (experienced by between 1 and 10% of people).[10]
Residual 'hangover' effects, such as sleepiness and impaired psychomotor and cognitive function, may persist into the day following nighttime administration. Such effects may impair the ability of users to drive safely and increase risks of falls and hip fractures.[15][30] Around 3% of people taking zolpidem are likely to break a bone as a result of a fall due to impaired coordination caused by the drug.[31]
Some users have reported unexplained sleepwalking while using zolpidem, as well as sleep driving, night eating syndrome while asleep, and performing other daily tasks while sleeping.[15] Research by Australia's National Prescribing Service found these events occur mostly after the first dose taken, or within a few days of starting therapy.[32] In February 2008, the Australian Therapeutic Goods Administration attached a boxed warning concerning this adverse effect.[33]
Tolerance, dependence and withdrawal

As zolpidem is associated with drug tolerance and substance dependence, its prescription guidelines are only for severe insomnia and short periods of use at the lowest effective dose.[10][11][12][13][34] Tolerance to the effects of zolpidem can develop in some people in just a few weeks.[35] Abrupt withdrawal may cause delirium, seizures, or other adverse effects, especially if used for prolonged periods and at high doses.[35][36] When drug tolerance and physical dependence to zolpidem develop, treatment usually entails a gradual dose reduction over a period of months to minimize withdrawal symptoms, which can resemble those seen during benzodiazepine withdrawal.[36] Failing that, an alternative method may be necessary for some people, such as a switch to a benzodiazepine equivalent dose of a longer-acting benzodiazepine drug, as for diazepam or chlordiazepoxide, followed by a gradual reduction in dose of the long-acting benzodiazepine.[36] In people who are difficult to treat, an inpatient flumazenil administration allows for rapid competitive binding of flumazenil to GABAA–receptor as an antagonist, thus stopping (and effectively detoxifying) zolpidem from being able to bind as an agonist on GABAA–receptor; slowly drug dependence or addiction to zolpidem will wane.[37]
Alcohol has cross tolerance with GABAA receptor positive allosteric modulators, such as the benzodiazepines and the nonbenzodiazepine drugs. For this reason, alcoholics or recovering alcoholics may be at increased risk of physical dependency or abuse of zolpidem.[10] It is not typically prescribed in people with a history of alcoholism, recreational drug use, physical dependency, or psychological dependency on sedative-hypnotic drugs.[10] A 2014 review found evidence of drug-seeking behavior, with prescriptions for zolpidem making up 20% of falsified or forged prescriptions.[38]
Rodent studies of the tolerance-inducing properties have shown that zolpidem has less tolerance-producing potential than benzodiazepines, but in primates, the tolerance-producing potential of zolpidem was the same as seen with benzodiazepines, therefore further research is necessary.[39]
Overdose
Overdose can lead to coma or death.[10] When overdose occurs, there are often other drugs in the person's system.[10][15]
Zolpidem overdose can be treated with the GABAA receptor antagonist flumazenil, which displaces zolpidem from its binding site on the GABAA receptor to rapidly reverse the effects of the zolpidem. It is unknown if dialysis is helpful.[10]
Detection in body fluids
Zolpidem may be quantitated in blood or plasma to confirm a diagnosis of poisoning in people who are hospitalized, to provide evidence in an impaired driving arrest, or to assist in a medicolegal death investigation. Blood or plasma zolpidem concentrations are usually in a range of 30–300 μg/L in persons receiving the drug therapeutically, 100–700 μg/L in those arrested for impaired driving, and 1000–7000 μg/L in victims of acute overdosage. Analytical techniques, in general, involve gas or liquid chromatography.[40][41][42]
Pharmacology
Mechanism of action

Zolpidem is a ligand of high-affinity positive modulator sites of GABAA receptors, which enhances GABAergic inhibition of neurotransmission in the central nervous system. It selectively binds to α1 subunits of this pentameric ion channel. Accordingly, it has strong hypnotic properties and weak anxiolytic, myorelaxant, and anticonvulsant properties.[9] Opposed to diazepam, zolpidem is able to bind to binary αβ GABA receptors, where it was shown to bind to the α1–α1 subunit interface.[43] Zolpidem has about 10-fold lower affinity for the α2- and α3- subunits than for α1, and no appreciable affinity for α5 subunit-containing receptors.[44][45] ω1 type GABAA receptors are the α1-containing GABAA receptors and are found primarily in the brain, the ω2 receptors are those that contain the α2-, α3-, α4-, α5-, or α6 subunits, and are found primarily in the spine. Thus, zolpidem favours binding to GABAA receptors located in the brain rather than the spine.[46] Zolpidem has no affinity for γ1 and γ3 subunit-containing receptors and, like the vast majority of benzodiazepine-like drugs, it lacks affinity for receptors containing α4 and α6.[47] Zolpidem modulates the receptor presumably by inducing a receptor conformation that enables an increased binding strength of the orthosteric agonist GABA towards its cognate receptor without affecting desensitization or peak currents.[48]
Like zaleplon, zolpidem may increase slow wave sleep but cause no effect on stage 2 sleep.[49] A meta-analysis that compared benzodiazepines against nonbenzodiazepines has shown few consistent differences between zolpidem and benzodiazepines in terms of sleep onset latency, total sleep duration, number of awakenings, quality of sleep, adverse events, tolerance, rebound insomnia, and daytime alertness.[50]
Pharmokinetics
Microsome studies indicate zolpidem is metabolized by CYP3A4 (61%) CYP2C9 (22%), CYP1A2 (14%), CYP2D6 (<3%), and CYP2C19 (<3%).[7] It is principally metabolized into three metabolites, none of which are believed to be pharmocologically active. The absolute bioavailability of zolpidem is about 70%. The drug reaches peak concentration in about 2 hours and has a half life in healthly adults of about 2-3 hours.[8][9] Zolpidem's half life is decreased in children and increased in the elderly and people with liver issues. While some studies show men metabolize zolipdem faster than women (possibly due to testosterone),[51] others do not.[9] A review found only a 33% lower clearance in women compared to men, suggesting the FDA's dosage reduction of 50% for women may have been too large.[52]
Interactions
People should not consume alcohol while taking zolpidem, and should not be prescribed opioid drugs nor take such illicit drugs recreationally.[53] Opioids can also increase the risk of becoming psychologically dependent on zolpidem. Use of opioids with zolpidem increases the risk of respiratory depression and death.[10] The US Food and Drug Administration (FDA) is advising that the opioid addiction medications buprenorphine and methadone should not be withheld from patients taking benzodiazepines or other drugs that depress the central nervous system (CNS).[54]
Next day sedation can be worsened if people take zolpidem while they are also taking antipsychotics, other sedatives, anxiolytics, antidepressant agents, antiepileptic drugs, and antihistamines. Some people taking antidepressants have had visual hallucinations when they also took zolpidem.[10]
Cytochrome P450 inhibitors, particularly CYP3A4 and CYP1A2 inhibitors such as fluvoxamine, ciprofloxacin, and clarithromycin[55] will increase the effects of a given dose of zolpidem.[10] Cytochrome P450 activators like St. John's Wort may decrease the activity of zolpidem.[10] One study found that caffeine increases the concentration over time curve of zolpidem by about 20% and furthermore found that caffeine cannot adequately compensate for the impaired cognition caused by zolpidem.[56]
Chemistry
Three syntheses of zolpidem are common. 4-methylacetophenone is used as a common precursor. This is brominated and reacted with 2-amino-5-methylpyridine to give the imidazopyridine. From here the reactions use a variety of reagents to complete the synthesis, either involving thionyl chloride or sodium cyanide. These reagents are challenging to handle and require thorough safety assessments.[57][58][59] Though such safety procedures are common in industry, they make clandestine manufacture difficult.
A number of major side-products of the sodium cyanide reaction have been characterised and include dimers and mannich products.[60]
History
Zolpidem was used in Europe starting in 1988, and was brought to market there by Synthelabo.[61] Synthelabo and Searle collaborated to bring it to market in the US, and it was approved in the United States in 1992 under the brand name "Ambien".[61][16] It became available as a generic medication in 2007.[17]
In 2015, the American Geriatrics Society said that zolpidem, eszopiclone and zaleplon met the Beers criteria and should be avoided in individuals 65 and over "because of their association with harms balanced with their minimal efficacy in treating insomnia."[26][27] The AGS stated the strength of the recommendation that older adults avoid zolpidem is "strong" and the quality of evidence supporting it is "moderate."[27]
Society and culture
Prescriptions in the US for all sleeping pills (including zolpidem) steadily declined from around 57 million tablets in 2013, to around 47 million in 2017, possibly in relation to concern about prescribing addictive drugs in the midst of the opioid crisis.[62]
Military use
The United States Air Force uses zolpidem as one of the hypnotics approved as a "no-go pill" (with a six-hour restriction on subsequent flight operation) to help aviators and special duty personnel sleep in support of mission readiness. (The other hypnotics used are temazepam and zaleplon.) "Ground tests" are required prior to authorization issued to use the medication in an operational situation.[63]
Recreational use
Zolpidem has potential for either medical misuse when the drug is continued long term without or against medical advice, or for recreational use when the drug is taken to achieve a "high".[64][65] The transition from medical use of zolpidem to high-dose addiction or drug dependence can occur with use, but some believe it may be more likely when used without a doctor's recommendation to continue using it, when physiological drug tolerance leads to higher doses than the usual 5 mg or 10 mg, when consumed through inhalation or injection, or when taken for purposes other than as a sleep aid.[64] Recreational use is more prevalent in those having been dependent on other drugs in the past, but tolerance and drug dependence can still sometimes occur in those without a history of drug dependence. Chronic users of high doses are more likely to develop physical dependence on the drug, which may cause severe withdrawal symptoms, including seizures, if abrupt withdrawal from zolpidem occurs.[66]
Other drugs, including benzodiazepines and zopiclone, are also found in high numbers of suspected drugged drivers.[15] Many drivers have blood levels far exceeding the therapeutic dose range, suggesting a high degree of excessive-use potential for benzodiazepines, zolpidem and zopiclone.[40] US Congressman Patrick J. Kennedy says that he was using zolpidem (Ambien) and promethazine (Phenergan) when caught driving erratically at 3 a.m.[67] "I simply do not remember getting out of bed, being pulled over by the police, or being cited for three driving infractions," Kennedy said.
Nonmedical use of zolpidem is increasingly common in the US, Canada, and the UK. Some users have reported decreased anxiety, mild euphoria, perceptual changes, visual distortions, and hallucinations.[68] Zolpidem was used by Australian Olympic swimmers at the London Olympics in 2012, leading to controversy.[69]
Regulation
For the stated reason of its potential for recreational use and dependence, zolpidem (along with the other benzodiazepine-like Z-drugs) is a Schedule IV substance under the Controlled Substances Act in the US. The United States patent for zolpidem was held by the French pharmaceutical corporation Sanofi-Aventis.[70]
Use in crime
The Z-drugs including zolpidem have been used as date rape drugs.[15][71] Zolpidem is available legally by prescription, and broadly prescribed unlike other date rape drugs: gamma-hydroxybutyrate (GHB), which is used to treat narcolepsy, or flunitrazepam (Rohypnol), which is only prescribed as a second-line choice for insomnia.[72] Zolpidem can typically be detected in bodily fluids for 36 hours, though it may be possible to detect it by hair testing much later, which is due to the short elimination half-life of 2.5–3 hours.[15] This use of the drug was highlighted during proceedings against Darren Sharper, who was accused of using the tablets he was prescribed to facilitate a series of rapes.[72][73]
Sleepwalking
Zolpidem received widespread media coverage in Australia after the death of a student who fell 20 metres (66 ft) from the Sydney Harbour Bridge while under the influence of zolpidem.[74]
Brands
As of September 2018, zolpidem was marketed under many brands: Adorma, Albapax, Ambien, Atrimon, Belbien, Bikalm, Cymerion, Dactive, Dalparan, Damixan, Dormeben, Dormilam, Dormilan, Dormizol, Eanox, Edluar, Flazinil, Fulsadem, Hypnogen, Hypnonorm, Intermezzo, Inzofresh, Ivadal, Ivedal, Le Tan, Lioram, Lunata, Medploz, Mondeal, Myslee, Nasen, Niterest, Nocte, Nottem, Noxidem, Noxizol, Nuo Bin, Nytamel, Nyxe, Olpitric, Onirex, Opsycon, Patz, Polsen, Sanval, Semi-Nax, Sleepman, Somex, Somidem, Somit, Somnil, Somnipax, Somnipron, Somno, Somnogen, Somnor, Sonirem, Sove, Soza, Stilnoct, Stilnox, Stilpidem, Stimin, Sublinox, Sucedal, Sumenan, Vicknox, Viradex, Xentic, Zasan, Zaviana, Ziohex, Zipsoon, Zodem, Zodenox, Zodium, Zodorm, Zolcent, Zoldem, Zoldorm, Zoldox, Zolep, Zolfresh, Zolip, Zolman, Zolmia, Zolnox, Zolnoxs, Zolodorm, Zolnyt, Zolpeduar, Zolpel, Zolpi, Zolpi-Q, Zolpic, Zolpidem, Zolpidem tartrate, Zolpidemi tartras, Zolpidemtartraat, Zolpidemtartrat, Zolpidemum, Zolpigen, Zolpihexal, Zolpimist, Zolpineo, Zolpinox, Zolpirest, Zolpistar, Zolpitop, Zolpitrac, Zolpium, Zolprem, Zolsana, Zolta, Zoltar, Zolway, Zomnia, Zonadin, Zonoct, Zopid, Zopidem, Zopim, and Zorimin.[1]
Research
While cases of zolpidem improving aphasia in people with stroke have been described, use for this purpose has unclear benefit.[75] Zolpidem has also been studied in persistent vegetative states with unclear effect.[76] A 2017 systematic review concluded that while there is preliminary evidence of benefit for treating disorders of movement and consciousness other than insomnia (including Parkinson's disease), more research is needed.[77] More recent research has found zolpidem treatment to be effective in the short term, but only in a small proportion of cases (estimated at around 5%) and only when the brain injury is of a specific type. Tolerance to the beneficial effects also develops rapidly, and so for these reasons while zolpidem may sometimes be used as a "last resort" treatment, it has numerous disadvantages and research continues into novel treatments that might provide the same kind of benefits in a larger proportion of patients, and with a more sustained benefit.[78]
Animal studies in FDA files for zolpidem showed a dose dependent increase in some types of tumors, although the studies were too small to reach statistical significance.[79] Some observational epidemiological studies have found a correlation between use of benzodiazepines and certain hypnotics including zolpidem and an increased risk of getting cancer, but others have found no correlation; a 2017 meta-analysis of such studies found a correlation, stating that use of hypnotics was associated with a 29% increased risk of cancer, and that "zolpidem use showed the strongest risk of cancer" with an estimated 34% increased risk, but noted that the results were tentative because some of the studies failed to control for confounders like cigarette smoking and alcohol use, and some of the studies analyzed were case–controls, which are more prone to some forms of bias.[80] Similarly, a meta-analysis of benzodiazepine drugs also shows their use is associated with increased risk of cancer.[81]
References
- "International brands for zolpidem". Drugs.com. Retrieved 15 March 2018.
- "Zolpidem Use During Pregnancy". Drugs.com. 30 June 2020. Retrieved 14 August 2020.
- Attarian HP (2016). Clinical Handbook of Insomnia. Springer. p. 109. ISBN 9783319414003.
- "Scheduling of zolpidem (Stilnox)". Therapeutic Goods Administration (TGA). 21 February 2008. Retrieved 15 August 2020.
- Matheson E, Hainer BL (July 2017). "Insomnia: Pharmacologic Therapy". American Family Physician. 96 (1): 29–35. PMID 28671376.
- "Ambien- zolpidem tartrate tablet, film coated". DailyMed. 29 August 2019. Retrieved 15 August 2020.
- Von Moltke LL, Greenblatt DJ, Granda BW, Duan SX, Grassi JM, Venkatakrishnan K, et al. (July 1999). "Zolpidem metabolism in vitro: responsible cytochromes, chemical inhibitors, and in vivo correlations". British Journal of Clinical Pharmacology. 48 (1): 89–97. doi:10.1046/j.1365-2125.1999.00953.x. PMC 2014868. PMID 10383565.
- "Zolpidem Tartrate". The American Society of Health-System Pharmacists. Retrieved 15 March 2018.
- Salvà P, Costa J (September 1995). "Clinical pharmacokinetics and pharmacodynamics of zolpidem. Therapeutic implications". Clinical Pharmacokinetics. 29 (3): 142–153. doi:10.2165/00003088-199529030-00002. PMID 8521677. S2CID 23391285.
- "Stilnoct 10mg Film-Coated Tablets - Summary of Product Characteristics (SmPC)". UK Electronic Medicines Compendium. 21 May 2018. Archived from the original on 20 August 2018. Retrieved 19 August 2018.
- "Guidance on the use of zaleplon, zolpidem and zopiclone for the short-term management of insomnia". NICE. 28 April 2004.
- Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, et al. (December 2017). "European guideline for the diagnosis and treatment of insomnia". Journal of Sleep Research. 26 (6): 675–700. doi:10.1111/jsr.12594. PMID 28875581.

- Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD (July 2016). "Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians". Annals of Internal Medicine. 165 (2): 125–33. doi:10.7326/M15-2175. PMID 27136449.

- "FDA Drug Safety Communication: FDA approves new label changes and dosing for zolpidem products and a recommendation to avoid driving the day after using Ambien CR". U.S. Food and Drug Administration (FDA). 14 May 2013.
- Gunja N (June 2013). "The clinical and forensic toxicology of Z-drugs". Journal of Medical Toxicology. 9 (2): 155–62. doi:10.1007/s13181-013-0292-0. PMC 3657020. PMID 23404347.
- "Drug Approval Package: Ambien (Zolpidem Tartrate) NDA 19908". U.S. Food and Drug Administration (FDA). 24 December 1999. Retrieved 15 August 2020.
- "FDA Approves First Generic Versions of Ambien (Zolpidem Tartrate) for the Treatment of Insomnia". U.S. Food and Drug Administration (FDA) (Press release). Archived from the original on 6 March 2010. Retrieved 24 January 2010.
- "Zolpidem". LiverTox. Archived from the original on 16 March 2018. Retrieved 15 March 2018.
- "Some Sleep Drugs Can Impair Driving". U.S. Food and Drug Administration (FDA). 13 June 2013. Retrieved 15 March 2018.
- "The Top 300 of 2020". ClinCalc. Retrieved 7 October 2022.
- "Zolpidem - Drug Usage Statistics". ClinCalc. Retrieved 7 October 2022.
- Huedo-Medina TB, Kirsch I, Middlemass J, Klonizakis M, Siriwardena AN (December 2012). "Effectiveness of non-benzodiazepine hypnotics in treatment of adult insomnia: meta-analysis of data submitted to the Food and Drug Administration". BMJ. 345: e8343. doi:10.1136/bmj.e8343. PMC 3544552. PMID 23248080.
- "Intermezzo (Zolpidem Tartarate)". rxlist.com. Retrieved 5 February 2018.
- "FDA Requires Lower Dosing of Zolpidem". The Medical Letter on Drugs and Therapeutics. The Medical Letter. 55 (1408): 5. 21 January 2013. PMID 23348358. Retrieved 14 April 2013.
- "FDA Drug Safety Communication: Risk of next-morning impairment after use of insomnia drugs; FDA requires lower recommended doses for certain drugs containing zolpidem (Ambien, Ambien CR, Edluar, and Zolpimist)". U.S. Food and Drug Administration (FDA). 10 January 2013. Archived from the original on 22 July 2017. Retrieved 14 April 2013.
- Merel SE, Paauw DS (July 2017). "Common Drug Side Effects and Drug-Drug Interactions in Elderly Adults in Primary Care". Journal of the American Geriatrics Society. 65 (7): 1578–1585. doi:10.1111/jgs.14870. PMID 28326532. S2CID 6621392.

- By the American Geriatrics Society 2015 Beers Criteria Update Expert Panel (November 2015). "American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults" (PDF). Journal of the American Geriatrics Society. 63 (11): 2227–46. doi:10.1111/jgs.13702. PMID 26446832. S2CID 38797655.
- Drugsdb.eu. "Zolpidem Pregnancy Warnings". Archived from the original on 18 August 2018. Retrieved 1 February 2014.
- Kripke DF (February 2016). "Mortality Risk of Hypnotics: Strengths and Limits of Evidence" (PDF). Drug Safety. 39 (2): 93–107. doi:10.1007/s40264-015-0362-0. PMID 26563222. S2CID 7946506.
- Vermeeren A (2004). "Residual effects of hypnotics: epidemiology and clinical implications". CNS Drugs. 18 (5): 297–328. doi:10.2165/00023210-200418050-00003. PMID 15089115. S2CID 25592318.
- Park SM, Ryu J, Lee DR, Shin D, Yun JM, Lee J (October 2016). "Zolpidem use and risk of fractures: a systematic review and meta-analysis". Osteoporosis International. 27 (10): 2935–44. doi:10.1007/s00198-016-3605-8. PMID 27105645. S2CID 4701575.
- "Zolpidem and sleep-related behaviours" (PDF). NPS Position Statement. National Prescribing Service Limited. July 2008. Archived from the original (PDF) on 10 April 2012.
- "Zolpidem ("Stilnox") – updated information – February 2008". Therapeutic Goods Administration (TGA). 21 February 2008. Archived from the original on 3 June 2009. Retrieved 22 June 2009.
- Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M (October 2008). "Clinical guideline for the evaluation and management of chronic insomnia in adults". Journal of Clinical Sleep Medicine. 4 (5): 487–504. doi:10.5664/jcsm.27286. PMC 2576317. PMID 18853708.
- Gunja N (June 2013). "In the Zzz zone: the effects of Z-drugs on human performance and driving". Journal of Medical Toxicology. 9 (2): 163–71. doi:10.1007/s13181-013-0294-y. PMC 3657033. PMID 23456542.
- Janhsen K, Roser P, Hoffmann K (January 2015). "The problems of long-term treatment with benzodiazepines and related substances". Deutsches Ärzteblatt International. 112 (1–2): 1–7. doi:10.3238/arztebl.2015.0001. PMC 4318457. PMID 25613443.
- Quaglio G, Lugoboni F, Fornasiero A, Lechi A, Gerra G, Mezzelani P (September 2005). "Dependence on zolpidem: two case reports of detoxification with flumazenil infusion". International Clinical Psychopharmacology. 20 (5): 285–7. doi:10.1097/01.yic.0000166404.41850.b4. PMID 16096519.
- Victorri-Vigneau C, Gérardin M, Rousselet M, Guerlais M, Grall-Bronnec M, Jolliet P (2014). "An update on zolpidem abuse and dependence". Journal of Addictive Diseases. 33 (1): 15–23. doi:10.1080/10550887.2014.882725. PMID 24467433. S2CID 30959471.
- Petroski RE, Pomeroy JE, Das R, Bowman H, Yang W, Chen AP, Foster AC (April 2006). "Indiplon is a high-affinity positive allosteric modulator with selectivity for alpha1 subunit-containing GABAA receptors". The Journal of Pharmacology and Experimental Therapeutics. 317 (1): 369–77. doi:10.1124/jpet.105.096701. PMID 16399882. S2CID 46510829.
- Jones AW, Holmgren A, Kugelberg FC (April 2007). "Concentrations of scheduled prescription drugs in blood of impaired drivers: considerations for interpreting the results". Therapeutic Drug Monitoring. 29 (2): 248–60. doi:10.1097/FTD.0b013e31803d3c04. PMID 17417081. S2CID 25511804.
- Gock SB, Wong SH, Nuwayhid N, Venuti SE, Kelley PD, Teggatz JR, Jentzen JM (October 1999). "Acute zolpidem overdose--report of two cases". Journal of Analytical Toxicology. 23 (6): 559–62. doi:10.1093/jat/23.6.559. PMID 10517569.
- Baselt R (2011). Disposition of Toxic Drugs and Chemicals in Man (9th ed.). Seal Beach, CA: Biomedical Publications. pp. 1836–1838.
- Che Has AT, Absalom N, van Nieuwenhuijzen PS, Clarkson AN, Ahring PK, Chebib M (June 2016). "Zolpidem is a potent stoichiometry-selective modulator of α1β3 GABAA receptors: evidence of a novel benzodiazepine site in the α1-α1 interface". Scientific Reports. 6: 28674. Bibcode:2016NatSR...628674C. doi:10.1038/srep28674. PMC 4921915. PMID 27346730.
- Pritchett DB, Seeburg PH (May 1990). "Gamma-aminobutyric acidA receptor alpha 5-subunit creates novel type II benzodiazepine receptor pharmacology". Journal of Neurochemistry. 54 (5): 1802–4. doi:10.1111/j.1471-4159.1990.tb01237.x. PMID 2157817. S2CID 86674799.
- Smith AJ, Alder L, Silk J, Adkins C, Fletcher AE, Scales T, Kerby J, Marshall G, Wafford KA, McKernan RM, Atack JR (May 2001). "Effect of alpha subunit on allosteric modulation of ion channel function in stably expressed human recombinant gamma-aminobutyric acid(A) receptors determined using (36)Cl ion flux". Molecular Pharmacology. 59 (5): 1108–18. doi:10.1124/mol.59.5.1108. PMID 11306694. S2CID 86156878.
- Rowlett JK, Woolverton WL (November 1996). "Assessment of benzodiazepine receptor heterogeneity in vivo: apparent pA2 and pKB analyses from behavioral studies". Psychopharmacology. 128 (1): 1–16. doi:10.1007/s002130050103. PMID 8944400. S2CID 25654504. Archived from the original on 12 January 2002.
- Wafford KA, Thompson SA, Thomas D, Sikela J, Wilcox AS, Whiting PJ (September 1996). "Functional characterization of human gamma-aminobutyric acidA receptors containing the alpha 4 subunit". Molecular Pharmacology. 50 (3): 670–8. PMID 8794909.
- Perrais D, Ropert N (January 1999). "Effect of zolpidem on miniature IPSCs and occupancy of postsynaptic GABAA receptors in central synapses". The Journal of Neuroscience. 19 (2): 578–88. doi:10.1523/JNEUROSCI.19-02-00578.1999. PMC 6782193. PMID 9880578.
- Noguchi H, Kitazumi K, Mori M, Shiba T (March 2004). "Electroencephalographic properties of zaleplon, a non-benzodiazepine sedative/hypnotic, in rats". Journal of Pharmacological Sciences. 94 (3): 246–51. doi:10.1254/jphs.94.246. PMID 15037809.
WARNING: The reference indicates that zaleplon-Sonata, not zolpidem, increases Slow-wave sleep
- Dündar Y, Dodd S, Strobl J, Boland A, Dickson R, Walley T (July 2004). "Comparative efficacy of newer hypnotic drugs for the short-term management of insomnia: a systematic review and meta-analysis". Human Psychopharmacology. 19 (5): 305–22. doi:10.1002/hup.594. PMID 15252823. S2CID 10888200.
- Olubodun JO, Ochs HR, von Moltke LL, Roubenoff R, Hesse LM, Harmatz JS, et al. (September 2003). "Pharmacokinetic properties of zolpidem in elderly and young adults: possible modulation by testosterone in men". British Journal of Clinical Pharmacology. 56 (3): 297–304. doi:10.1046/j.0306-5251.2003.01852.x. PMC 1884349. PMID 12919178.
- Greenblatt DJ, Harmatz JS, Roth T (May 2019). "Zolpidem and Gender: Are Women Really At Risk?". Journal of Clinical Psychopharmacology. 39 (3): 189–199. doi:10.1097/JCP.0000000000001026. PMID 30939589. S2CID 92998845.
- "FDA Drug Safety Communication: FDA warns about serious risks and death when combining opioid pain or cough medicines with benzodiazepines; requires its strongest warning". U.S. Food and Drug Administration (FDA). 31 August 2016. Retrieved 18 August 2018.
- "FDA urges caution about withholding opioid addiction medications". U.S. Food and Drug Administration. 20 September 2017. Retrieved 15 August 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lee CM, Jung EH, Byeon JY, Kim SH, Jang CG, Lee YJ, Lee SY (December 2019). "Effects of steady-state clarithromycin on the pharmacokinetics of zolpidem in healthy subjects". Archives of Pharmacal Research. 42 (12): 1101–1106. doi:10.1007/s12272-019-01201-5. PMID 31820397. S2CID 209164976.
- Cysneiros RM, Farkas D, Harmatz JS, von Moltke LL, Greenblatt DJ (July 2007). "Pharmacokinetic and pharmacodynamic interactions between zolpidem and caffeine". Clinical Pharmacology and Therapeutics. 82 (1): 54–62. doi:10.1038/sj.clpt.6100211. PMID 17443132. S2CID 46250744.
- Johnson DS, Li JJ (2007). The art of drug synthesis. Hoboken, N.J.: Wiley-Interscience. pp. Chapter 15, Section 2. ISBN 9780471752158.
- IN 246080, Rawalnath SR, Crasta Santosh R, Saxena A, "Process for the preparation of zolpidem", published 21 December 2005, issued 14 February 2011
- Sumalatha Y (2009). "A simple and efficient synthesis of hypnotic agent, zolpidem and its related substances". Arkivoc. 2009 (2): 315–320. doi:10.3998/ark.5550190.0010.230.
- Sumalatha Y (2009). "Synthesis and spectral characterization of zolpidem related substances - hypnotic agent". Arkivoc. 2009 (7): 143–149. doi:10.3998/ark.5550190.0010.714.
- Morris S (22 December 1992). "Searle Wins Ok To Sell Sleep Aid". Chicago Tribune.
- Crow D (1 June 2018). "Ambien defence: the real side effects of sleeping pills". Financial Times.
- "Air Force Special Operations Command Instruction 48-101" (PDF). e-publishing.af.mil. 30 November 2012. Archived from the original (PDF) on 11 June 2014. Retrieved 8 March 2014.
- Brett J, Murnion B (October 2015). "Management of benzodiazepine misuse and dependence". Australian Prescriber. 38 (5): 152–5. doi:10.18773/austprescr.2015.055. PMC 4657308. PMID 26648651.
- Griffiths RR, Johnson MW (2005). "Relative abuse liability of hypnotic drugs: a conceptual framework and algorithm for differentiating among compounds". The Journal of Clinical Psychiatry. 66 (Suppl 9): 31–41. PMID 16336040.
- Barrero-Hernández FJ, Ruiz-Veguilla M, López-López MI, Casado-Torres A (2002). "[Epileptic seizures as a sign of abstinence from chronic consumption of zolpidem]" [Epileptic seizures as a sign of abstinence from chronic consumption of zolpidem]. Revista de Neurología (in Spanish). 34 (3): 253–6. doi:10.33588/rn.3403.2001316. PMID 12022074.
- "Kennedy To Enter Drug Rehab After Car Crash; Congressman Wrecked Car Near Capitol". Archived from the original on 28 March 2020. Retrieved 23 June 2009.
- Mulvihill K. "Ambien Abuse on Rise Among Teens". KSL. Archived from the original on 20 February 2009. Retrieved 22 June 2009.
- "Swimming Australia's 'Stilnox six' given final warning as AOC decides not to issue any further sanctions". ABC News. www.abc.net.au. 23 August 2013. Retrieved 3 August 2016.
- US 4382938, Kaplan J-P, George P, "Imidazo[1,2-a] pyridine derivatives and their application as pharmaceuticals", published 10 May 1983, issued 17 July 1984, assigned to Synthelabo
- "Zolpidem most frequently used date rape drug in Korea". The Korea Herald. 29 February 2016.
- Schrotenboer B (26 March 2014). "Darren Sharper case spotlights sleep drug's dark side". USA Today.
- Red C (17 February 2014). "In the rape case against Darren Sharper, former LAPD detective says Ambien is used often and can be similar to GHB". Daily News. New York.
- "Stilnox blamed for Harbour Bridge death". nineMSN News. 23 February 2007. Archived from the original on 15 June 2007.
- de Boissezon X, Peran P, de Boysson C, Démonet JF (July 2007). "Pharmacotherapy of aphasia: myth or reality?". Brain and Language. 102 (1): 114–25. doi:10.1016/j.bandl.2006.07.004. PMID 16982084. S2CID 38304960.
- Georgiopoulos M, Katsakiori P, Kefalopoulou Z, Ellul J, Chroni E, Constantoyannis C (2010). "Vegetative state and minimally conscious state: a review of the therapeutic interventions". Stereotactic and Functional Neurosurgery. 88 (4): 199–207. doi:10.1159/000314354. PMID 20460949.
- Bomalaski MN, Claflin ES, Townsend W, Peterson MD (September 2017). "Zolpidem for the Treatment of Neurologic Disorders: A Systematic Review". JAMA Neurology. 74 (9): 1130–1139. doi:10.1001/jamaneurol.2017.1133. PMID 28655027. S2CID 10756280.
- Arnts H, van Erp WS, Boon LI, Bosman CA, Admiraal MM, Schrantee A, et al. (September 2020). "Awakening after a sleeping pill: Restoring functional brain networks after severe brain injury". Cortex; A Journal Devoted to the Study of the Nervous System and Behavior. 132: 135–146. doi:10.1016/j.cortex.2020.08.011. PMID 32979847.
- Kripke DF (2016). "Hypnotic drug risks of mortality, infection, depression, and cancer: but lack of benefit". F1000Research. 5: 918. doi:10.12688/f1000research.8729.1. PMC 4890308. PMID 27303633.
- Kim DH, Kim HB, Kim YH, Kim JY (July 2018). "Use of Hypnotics and Risk of Cancer: A Meta-Analysis of Observational Studies". Korean Journal of Family Medicine. 39 (4): 211–218. doi:10.4082/kjfm.17.0025. PMC 6056405. PMID 29973038.
- Kim HB, Myung SK, Park YC, Park B (February 2017). "Use of benzodiazepine and risk of cancer: A meta-analysis of observational studies". International Journal of Cancer. 140 (3): 513–525. doi:10.1002/ijc.30443. PMID 27667780.
External links
- "Zolpidem". Drug Information Portal. U.S. National Library of Medicine.