Facts about Hypoplastic Left Heart Syndrome
Hypoplastic (pronounced hi-puh-PLAS-tik) left heart syndrome or HLHS is a birth defect that affects normal blood flow through the heart.
What is Hypoplastic Left Heart Syndrome?
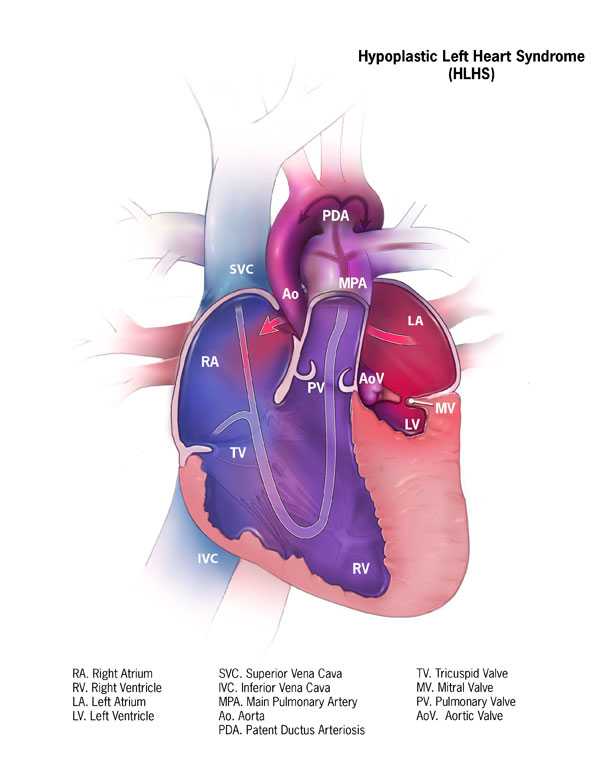
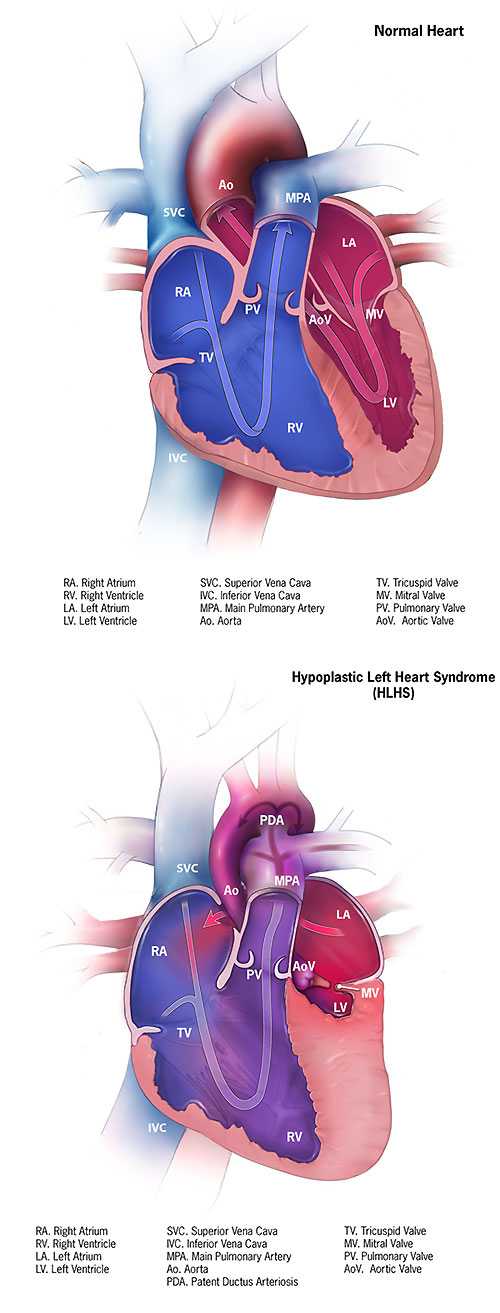
Hypoplastic left heart syndrome (HLHS) is a birth defect that affects normal blood flow through the heart. As the baby develops during pregnancy, the left side of the heart does not form correctly. Hypoplastic left heart syndrome is one type of congenital heart defect. Congenital means present at birth.
Hypoplastic left heart syndrome affects a number of structures on the left side of the heart that do not fully develop, for example:
- The left ventricle is underdeveloped and too small.
- The mitral valves is not formed or is very small.
- The aortic valve is not formed or is very small.
- The ascending portion of the aorta is underdeveloped or is too small.
- Often, babies with hypoplastic left heart syndrome also have an atrial septal defect, which is a hole between the left and right upper chambers (atria) of the heart.
In a baby without a congenital heart defect, the right side of the heart pumps oxygen-poor blood from the heart to the lungs. The left side of the heart pumps oxygen-rich blood to the rest of the body. When a baby is growing in a mother’s womb during pregnancy, there are two small openings between the left and right sides of the heart: the patent ductus arteriosus and the patent foramen ovale. Normally, these openings will close a few days after birth.
In babies with hypoplastic left heart syndrome, the left side of the heart cannot pump oxygen-rich blood to the body properly. During the first few days of life for a baby with hypoplastic left heart syndrome, the oxygen-rich blood bypasses the poorly functioning left side of the heart through the patent ductus arteriosus and the patent foramen ovale. The right side of the heart then pumps blood to both the lungs and the rest of the body. However, among babies with hypoplastic left heart syndrome, when these openings close, it becomes hard for oxygen-rich blood to get to the rest of the body.
Learn more about how the heart works »
Occurrence
The Centers for Disease Control and Prevention (CDC) estimates that each year about 960 babies in the United States are born with hypoplastic left heart syndrome.1 In other words, about 1 out of every 4,344 babies born in the United States each year is born with hypoplastic left heart syndrome.
Did You Know?
Women can take steps before and during pregnancy to reduce the risk of having a baby born with birth defects. Such steps include taking a daily multivitamin with folic acid (400 micrograms), not smoking, and not drinking alcohol during pregnancy.
Teagan’s Story

Teagan was born with hypoplastic left heart syndrome. Read his story as well as other stories from families affected by hypoplastic left heart syndrome »
Causes and Risk Factors
The causes of heart defects such as hypoplastic left heart syndrome among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. These types of heart defects also are thought to be caused by a combination of genes and other risk factors, such as things the mother comes in contact with in the environment or what the mother eats or drinks or the medicines the mother uses.
Read more about CDC’s work on causes and risk factors »
Diagnosis
Hypoplastic left heart syndrome may be diagnosed during pregnancy or soon after the baby is born.
During Pregnancy
During pregnancy, there are screening tests (also called prenatal tests,) to check for birth defects and other conditions. Hypoplastic left heart syndrome may be diagnosed during pregnancy with an ultrasound, (which creates pictures of the body). Some findings from the ultrasound may make the health care provider suspect a baby may have hypoplastic left heart syndrome. If so, the health care provider can request a fetal echocardiogram, an ultrasound of the baby’s heart, to confirm the diagnosis.This test can show problems with the structure of the heart and how the heart is working with this defect.
After the Baby Is Born
Babies with hypoplastic left heart syndrome might not have trouble for the first few days of life while the patent ductus arteriosus and the patent foramen ovale (the normal openings in the heart) are open, but quickly develop signs after these openings are closed, including:
- Problems breathing,
- Pounding heart,
- Weak pulse, or
- Ashen or bluish skin color.
During a physical examination, a doctor can see these signs or might hear a heart murmur (an abnormal whooshing sound caused by blood not flowing properly). If a murmur is heard or other signs are present, the health care provider might request one or more tests to make a diagnosis, the most common being an echocardiogram. Echocardiography also is useful for helping the health care provider follow the child’s health over time.
Treatments
Treatments for some health problems associated with hypoplastic left heart syndrome might include:
Medicines
Some babies and children will need medicines to help strengthen the heart muscle, lower their blood pressure, and help the body get rid of extra fluid.
Nutrition
Some babies with hypoplastic left heart syndrome become tired while feeding and do not eat enough to gain weight. To make sure babies have a healthy weight gain, a special high-calorie formula might be prescribed. Some babies become extremely tired while feeding and might need to be fed through a feeding tube.
Surgery
Soon after a baby with hypoplastic left heart syndrome is born, multiple surgeries done in a particular order are needed to increase blood flow to the body and bypass the poorly functioning left side of the heart. The right ventricle becomes the main pumping chamber to the body. These surgeries do not cure hypoplastic left heart syndrome, but help restore heart function. Sometimes medicines are given to help treat symptoms of the defect before or after surgery. Surgery for hypoplastic left heart syndrome usually is done in three separate stages:
- Norwood Procedure
This surgery usually is done within the first 2 weeks of a baby’s life. Surgeons create a “new” aorta and connect it to the right ventricle. They also place a tube from either the aorta or the right ventricle to the vessels supplying the lungs (pulmonary arteries). Thus, the right ventricle can pump blood to both the lungs and the rest of the body. This can be a very challenging surgery. After this procedure, an infant’s skin still might look bluish because oxygen-rich and oxygen-poor blood still mix in the heart. - Bi-directional Glenn Shunt Procedure
This usually is performed when an infant is 4 to 6 months of age. This procedure creates a direct connection between the pulmonary artery and the vessel (the superior vena cava) returning oxygen-poor blood from the upper part of the body to the heart. This reduces the work the right ventricle has to do by allowing blood returning from the body to flow directly to the lungs. - Fontan Procedure
This procedure usually is done sometime during the period when an infant is 18 months to 3 years of age. Doctors connect the pulmonary artery and the vessel (the inferior vena cava) returning oxygen-poor blood from the lower part of the body to the heart, allowing the rest of the blood coming back from the body to go to the lungs. Once this procedure is complete, oxygen-rich and oxygen-poor blood no longer mix in the heart and an infant’s skin will no longer look bluish.
Infants who have these surgeries are not cured; they may have lifelong complications.
Infants with hypoplastic left heart syndrome will need regular follow-up visits with a cardiologist (a heart doctor) to monitor their progress. If the hypoplastic left heart syndrome defect is very complex, or the heart becomes weak after the surgeries, a heart transplant may be needed. Infants who receive a heart transplant will need to take medicines for the rest of their lives to prevent their body from rejecting the new heart.
References
- Parker SE, Mai CT, Canfield MA, et al; for the National Birth Defects Prevention Network. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol. 2010;88:1008-16.
- Page last reviewed: November 8, 2016
- Page last updated: November 8, 2016
- Content source:


 ShareCompartir
ShareCompartir