Interim Guidance for Emergency Medical Services (EMS) Systems and 9-1-1 Public Safety Answering Points (PSAPs) for Management of Patients Under Investigation (PUIs) for Ebola Virus Disease (EVD) in the United States
Updated: September 10, 2015
The recommendations on this page are no longer in effect and will not be updated.
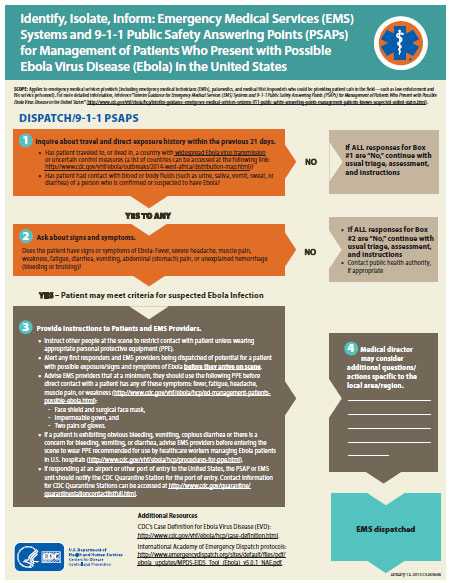
Algorithm for Emergency Medical Services and 9-1-1 Public Safety Answering Points [PDF – 4 pages]
Special note: The likelihood of contracting Ebola virus disease (EVD) in the United States is extremely low unless a person has direct contact with the blood or body fluids (like urine, saliva, vomit, sweat, and diarrhea) of a person infected with EVD and showing symptoms. The majority of patients with fever and other non-specific signs and symptoms* in the United States do not have EVD. The transmission risk posed to those in direct contact with patients with EVD and early symptoms is lower than the risk from a patient hospitalized with severe EVD. Nevertheless, because early EVD symptoms are similar to those seen with other febrile illnesses, providers should consider and assess patients for the possibility of EVD. The guidance provided in this document reflects lessons learned from the recent experience caring for patients with EVD in U.S. healthcare settings. Although inpatient hospital settings generally present a higher risk of Ebola virus transmission to healthcare personnel, transports by emergency medical services (EMS) present unique challenges because of the uncontrolled nature of the work, the potential for resuscitation procedures being needed, enclosed space during transport, and a varying range of patient acuity. When preparing for and responding to patients under investigation (PUIs) for EVD, close coordination and frequent communications are important among 9-1-1 Public Safety Answering Points (PSAPs)— commonly known as 9-1-1 call centers, the EMS system, healthcare facilities, and the public health system.
* Signs and symptoms of EVD include: fever, severe headache, muscle pain, weakness, fatigue, diarrhea, vomiting, abdominal (stomach) pain, or unexplained hemorrhage (bleeding or bruising). Symptoms may appear anywhere from 2 to 21 days after exposure to EVD, but the average is 8 to 10 days.
Page Summary
What’s New: This version of the guidance has been updated to clarify the minimum personal protective equipment (PPE) levels for EMS personnel and first responders. The updated information reflects the PPE guidance described in CDC's Identify, Isolate, Inform: Emergency Department Evaluation and Management for Patients Under Investigation (PUIs) for Ebola Virus Disease (EVD) and Guidance on Personal Protective Equipment To Be Used by Healthcare Workers During Management of Patients with Ebola Virus Disease (EVD) in U.S. Hospitals, Including Procedures for Putting On (Donning) and Removing (Doffing).
Who this is for: EMS providers (including emergency medical technicians [EMTs], paramedics, and medical first responders who could be providing patient care in the field–such as law enforcement and fire service personnel–as well as managers of 9-1-1 PSAPS, EMS agencies, EMS systems, and agencies with medical first responders.
What this is for: Guidance to assure EMS and first responders are safe and patients are appropriately managed while handling inquiries and responding to PUIs.
How to use: Employers and supervisors should use this information to understand and explain to staff how to respond and stay safe. Supervisors can use this information to prepare and train EMS personnel. Individual providers can use this information to stay safe when responding to PUIs.
Key Points
- The likelihood of contracting EVD in the United States is extremely low unless a person has direct contact with the blood or body fluids (like urine, saliva, vomit, sweat, and diarrhea) of a person with EVD and showing symptoms.
- It is important for PSAPs to question callers about:
- Having traveled internationally or having had contact with a person with confirmed EVD within the previous 21 days; AND
- Signs and symptoms of EVD (such as fever, severe headache, muscle pain, weakness, fatigue, diarrhea, vomiting, abdominal pain, and unexplained hemorrhage).
- Managers of 9-1-1 PSAPs, EMS Agencies, EMS systems, and agencies with medical first responders such as fire and law enforcement should collaborate with local public health authorities to develop coordinated plans for responding to a PUI in a given jurisdiction, including the possibility of designating certain teams for this response.
- All personnel should be trained regarding Ebola response protocols. Those who may respond to a PUI also should be trained in the use of the appropriate PPE consistent with their response role.
- If PSAP call takers have information alerting them to a PUI, they should make sure first responders and EMS providers are made aware of the potential for a patient with possible exposure/signs and symptoms of Ebola before the responders arrive on scene. This will enable EMS providers to select and correctly put on PPE following the principles described in CDC’s Identify, Isolate, Inform: Emergency Department Evaluation and Management for Patients Under Inverstigation (PUIs) for Ebola Virus Disease (EVD) and Guidance on Personal Protective Equipment To Be Used by Healthcare Workers During Management of Patients with Ebola Virus Disease (EVD) in U.S. Hospitals, Including Procedures for Putting On (Donning) and Removing (Doffing). The fundamental principle of standard and transmission-based precautions is to prevent contact with blood or potentially infectious body fluid. However, as prehospital patient care frequently is provided in an uncontrolled environment with unique operational challenges, EMS systems must design their procedures to accommodate their local operational challenges. For PPE use, responders also may wish to review the Interagency Board’s Recommendations on Selection and Use of Personal Protective Equipment for First Responders against Ebola Exposure Hazards (PDF).
- Before working with PUIs, providers should have repeated training and have demonstrated competency in all Ebola-related infection control practices and procedures, specifically in donning/doffing proper PPE.
- When EMS providers arrive at the scene, they should immediately check for symptoms and risk factors for EVD and don PPE appropriate to the situation. When transporting a PUI, EMS providers should notify the receiving healthcare facility in advance, so that proper infection control precautions are prepared at the healthcare facility before arrival. Medical directors and EMS agencies should collaborate with healthcare and public health agencies to define local or regional protocols for transporting a PUI to an appropriate facility for Ebola triage and care.
- Local protocols should be developed for cleaning and disinfecting of the ambulance and equipment as well as disposing of medical waste consistent with this guidance.
The guidance provided in this document is based on current knowledge of Ebola. Updates will be posted as needed on the CDC Ebola webpage.The information contained in this document is intended to complement existing guidance for healthcare personnel, Identify, Isolate, Inform: Emergency Department Evaluation and Management for Patients Under Investigation (PUIs) for Ebola Virus Disease (EVD) and Infection Prevention and Control Recommendations for Hospitalized Patients Under Investigation (PUIs) for Ebola Virus Disease (EVD) in U.S. Hospitals.
Background
The current Ebola outbreak in West Africa has increased the possibility of patients with EVD traveling from affected countries to the United States.1 The likelihood of contracting EVD is extremely low unless a person has had direct unprotected contact with blood or body fluids (like urine, saliva, vomit, sweat, and diarrhea) of a person with EVD and showing symptoms. Initial signs and symptoms of EVD include fever, chills, fatigue, weakness, and muscle aches, followed approximately 4 to 6 days after illness onset by diarrhea, nausea, vomiting, and abdominal pain. Other symptoms such as chest pain, shortness of breath, headache, or confusion also may develop. Signs and symptoms may become increasingly severe and may include jaundice (yellow skin), severe weight loss, mental confusion, bleeding inside and outside the body, and complications such as shock and multiorgan failure.2
EVD can cause severe illness, and extra care is needed when coming into direct contact with a recent traveler from a country with an EVD outbreak who also has signs and symptoms of EVD. The initial signs and symptoms of EVD are similar to many other more common diseases found in West Africa, such as malaria and typhoid. EVD should be considered in anyone with a fever who has traveled to, or lived in, an area where EVD is present.3 In general, the majority of febrile patients presenting to first responders and EMS in the United States do not have EVD, and the risk posed by patients with early, limited symptoms is lower than from a patient hospitalized with severe EVD.
The incubation period for EVD, from exposure to when signs or symptoms appear, ranges from 2 to 21 days (most commonly 8 to 10 days). Any patient with signs or symptoms of EVD should be considered infectious.
Key safe work practices include avoiding
- Unprotected exposure to blood or body fluids of patients with EVD through contact with skin, mucous membranes of the eyes, nose, or mouth.
- Injuries with contaminated needles or other sharp objects.
- Aerosol-generating procedures when possible.
Coordination among 9-1-1 PSAPs and the EMS system is important. Training and exercising with healthcare facilities and the public health system are critical when preparing to respond to PUIs. Each 9-1-1 and EMS system should include an EMS medical director to provide appropriate medical oversight.
Case Definition for EVD
CDC’s most current case definition for Ebola may be accessed at: Case Definition for Ebola Virus Disease (EVD)
Recommendations for 9-1-1 PSAPs
State and local EMS authorities should coordinate with state and local public health, PSAPs, and other emergency call centers to use modified caller queries about EVD, outlined below, when they consider the risk of EVD to be higher in their community. This should be decided from information provided by local, state, and federal public health authorities, including the city or county health department(s), state health department(s), and CDC.
Modified Caller Queries
It will be important for PSAPs to question callers and determine the possibility of anyone having EVD. This information should be communicated immediately to EMS providers before arrival in order to assign the appropriate EMS resources. Local or state public health officials should also be notified. PSAPs should utilize medical dispatch procedures that are coordinated with their EMS medical director and with the local public health department.
- If PSAP call takers suspect a caller is reporting symptoms of EVD, they should screen callers for risk factors within the past 3 weeks (21 days):
- Having traveled internationally.
- Contact with blood or body fluids (including but not limited to urine, saliva, vomit, sweat, and diarrhea) of a PUI or patient with confirmed EVD.
- If PSAP call takers have information alerting them to a PUI, they should make sure any first responders and EMS providers are made aware of the potential for a patient with possible exposure/signs and symptoms of EVD before the responders arrive on scene.
- If responding to a report of an ill traveler at an airport or other port of entry to the United States, the PSAP or EMS unit should notify the CDC Quarantine Station for the port of entry. For contact information check the CDC Quarantine Station Contact List. The PSAP or EMS unit also may call CDC’s Emergency Operations Center at 770-488-7100 to be connected with the appropriate quarantine station.
Recommendations for EMS and Medical First Responders
For the purposes of this section, “EMS provider” means prehospital EMS and medical first responders. These EMS provider practices should be based on the most up-to-date Ebola clinical recommendations and information from appropriate public health authorities and EMS medical direction.
When state and local EMS authorities determine there is an increased risk (based on information provided by local, state, and federal public health authorities, including the city or county health department[s], state health department[s], and the CDC), they may direct EMS providers to modify their practices as described below.
Patient assessment
- To minimize potential exposure, only one EMS provider should approach the patient and perform the initial screening from at least 3 feet away from the patient. Based on the initial screening, if the EMS provider suspects the patient could have EVD, then PPE should be put on before coming into close contact with the patient. Keep other emergency responders further away, while assuring they are still able to support the provider with primary assessment duties.
- No one should have direct contact with a patient who may have EVD without wearing appropriate PPE.
- During patient assessment and management, EMS personnel should consider the signs, symptoms, and risk factors of EVD. A relevant exposure history should be taken including:
- Residence in, or travel to, a country or area with widespread Ebola virus transmission or cases in urban settings with uncertain control measures.
- Contact with blood or body fluids (including but not limited to urine, saliva, vomit, sweat, and diarrhea) of a PUI or patient with confirmed EVD.
- Patients who meet the criteria should be further questioned regarding the presence of signs or symptoms of EVD such as fever, severe headache, muscle pain, weakness, fatigue, diarrhea, vomiting, abdominal pain, diarrhea, and unexplained hemorrhage.
Safety and PPE
- If PSAP call takers advise the patient is suspected of having EVD, EMS personnel should put on the PPE appropriate for PUIs before entering the scene. PPE options are described in detail below.
- To minimize potential exposure, only one EMS provider should approach the patient and perform the initial screening from at least 3 feet away from the patient. If, based on the initial screening, the EMS provider suspects the patient might have EVD, then PPE should be put on before coming into close contact with the patient. Keep the other emergency responders further away, while assuring they are still able to support the provider with primary assessment duties.
- No one should have direct contact with a patient who may have EVD without wearing appropriate PPE.
Based on the clinical presentation of the patient, there are two PPE options.
- If the patient is not exhibiting obvious bleeding, vomiting, or diarrhea and there is no concern for bleeding, vomiting, or diarrhea, EMS personnel should follow the PPE guidance for clinically stable PUIs.
- If the patient is exhibiting obvious bleeding, vomiting, or diarrhea or there is concern for potential bleeding, vomiting, or diarrhea then EMS personnel should wear PPE described in Guidance on Personal Protective Equipment To Be Used by Healthcare Workers During Management of Patients with Ebola Virus Disease (EVD) in U.S. Hospitals, Including Procedures for Putting On (Donning) and Removing (Doffing).
- PPE should be put on before entering a scene with a PUI and continue to be worn until providers no longer are in contact with the patient. PPE should be carefully put on and taken off under the supervision of a trained observer as described in Guidance on Personal Protective Equipment To Be Used by Healthcare Workers During Management of Patients with Ebola Virus Disease (EVD) in U.S. Hospitals, Including Procedures for Putting On (Donning) and Removing (Doffing).
- If the patient exhibits obvious bleeding, vomiting, copious diarrhea or a clinical condition that warrants invasive or aerosol-generating procedures (such as intubation, suctioning, active resuscitation), then use PPE designated for the care of hospitalized patients.
- If blood, body fluids, secretions, or excretions from a PUI come into direct contact with the EMS provider’s unprotected skin or mucous membranes, then the EMS provider should immediately stop working. They should wash the affected skin surfaces with a cleansing or antiseptic solution, and mucous membranes (e.g., conjunctiva) should be irrigated with a large amount of water or eyewash solution, as per usual protocols. All waste should be placed in a biohazard bag. EMS providers should report exposure to an occupational health provider, supervisor, or designated infection control officer for immediate care.
Patient management
- No one should have direct contact with a PUI without wearing appropriate PPE.
- Use caution when approaching a PUI. On rare occasions, illness can cause delirium, with erratic behavior, such as flailing or staggering. This type of behavior can place EMS providers at additional risk of exposure.
- Keep the patient separated from others as much as possible.
- Limit the number of providers who care for a PUI. All EMS personnel having direct contact with a PUI must wear PPE.
- Limit the use of needles and other sharps as much as possible. Needles and sharps should be handled with extreme care and disposed in puncture-proof, sealed containers specific to the care of this patient, in accordance with OSHA’s Bloodborne Pathogens Standard, 29 CFR 1910.10306. Do not dispose of used needles and sharps in containers that have sharps from other patients in them.
- Consider giving the patient oral medicine to reduce nausea, per medical director protocols and consistent with scope of practice.
- If patient is vomiting, give them a large red biohazard bag to contain any emesis.
- If patient has profuse diarrhea, consider wrapping the patient in an impermeable sheet to reduce contamination of other surfaces.
- Prehospital resuscitation procedures such as endotracheal intubation, open suctioning of airways, and cardiopulmonary resuscitation frequently result in a large amount of body fluids, such as saliva and vomit. Performing these procedures in a less controlled environment (for example, a moving vehicle) increases risk of exposure to infectious pathogens for EMS providers. Perform these procedures under safer circumstances (when the vehicle has stopped, upon arrival at the hospital destination) and wear the PPE recommended by CDC to use during aerosol-generating procedures.
Prehospital care considerations
Prehospital patient care is frequently provided in an uncontrolled environment with unique operational challenges. EMS systems must design their procedures to accommodate their local operational challenges while still following the principles of CDC PPE guidance.
- It may be as simple as having one provider put on PPE and manage the patient while the other provider does not engage in patient care but serves in the role of trained observer.
- There may be situations where a patient must be carried and multiple providers are required to put on PPE. EMS providers wearing PPE who have cared for the patient must remain in the back of the ambulance and should not serve as the driver.
- EMS agencies may consider sending additional resources to eliminate the need for putting on PPE (field-donning) by additional providers. For example, a dedicated driver for the EMS unit may not need to wear PPE if the patient compartment is isolated from the cab.
- Doffing of PPE must be performed with meticulous care to prevent self-contamination. See guidance on PPE doffing and ensure training emphasizes adherence to a standardized protocol.
Additional Considerations
- Prepare and use safe procedures to treat and transport the patient to the hospital.
- The EMS provider driving the ambulance should contact the receiving hospital and follow local or regional protocols to transport the patient to the receiving hospital.
- Remove and keep nonessential equipment away from the patient on the scene and in the ambulance. This will eliminate or minimize contamination.
- Avoid contamination of reusable porous surfaces not designated for single use. Cover the stretcher with an impermeable material.
- Conduct appropriate patient assessment according to established protocols, using minimal equipment.
EMS Transport of Patient to a Healthcare Facility
People who may have an exposure history and signs and symptoms suggestive of EVD should be transported to a healthcare facility prepared to further evaluate and manage the patient as instructed by EMS medical direction and local/regional protocols. These should be consistent with the predefined transportation/destination plan developed by public health officials, hospital, medical and EMS personnel.
- Isolate the ambulance driver from the patient compartment.
- During transport, ensure that an appropriate disinfectant (EPA approved hospital grade disinfectant with a nonenveloped virus claim) is available in spray bottles or as commercially prepared wipes.
Interfacility transport
EMS personnel involved in the interfacility transfer of PUIs or patients with confirmed EVD should follow donning and doffing procedures as recommended in CDC guidance. Provide patient care as needed to minimize the contact with patient and follow infection control guidelines noted below.
Infection control
EMS providers can safely manage a PUI by following the recommendations for appropriate PPE and following these CDC recommendations:
- Limit activities, especially during transport, -that can increase the risk of exposure to infectious material.
- Limit the use of needles and other sharps as much as possible. Needles and sharps should be handled with extreme care and disposed in puncture-proof, sealed containers that are specific to the care of the patient, in accordance with OSHA’s Bloodborne Pathogens standard, 29 CFR 1910.1030. Do not dispose of used needles and sharps in containers that have sharps from other patients in them.
- Invasive procedures should be limited to those essential for patient management.
- Donning and doffing of PPE must be supervised by a trained observer to ensure proper completion of established PPE protocols. In collaboration with the receiving hospital, EMS agencies should consider how best to facilitate a supervised doffing process.
Documentation of patient care
- Documentation of patient care should be done after EMS providers have completed their personal cleaning and decontamination of equipment and vehicle. Any written documentation should match the verbal communication given to the emergency department providers at time of patient handover.
- EMS documentation should include a listing of public safety providers involved in the response and level of contact with the patient (for example, no contact with patient, provided direct patient care). This documentation may need to be shared with local public health authorities.
Cleaning EMS Transport Vehicles after Transporting a PUI for EVD
The following are general guidelines for cleaning or maintaining EMS transport vehicles and equipment after transporting a PUI:
- EMS providers performing cleaning and disinfection where body fluids from a PUI are present (vomit, diarrhea, sweat, urine or blood) should wear PPE as recommended by the CDC. If no body fluids from a patient with EVD are present then minimal PPE should be worn:
- Face shield and surgical face mask
- Impermeable gown
- Two pairs of gloves
- Use a U.S. Environmental Protection Agency (EPA)-registered hospital disinfectant with a label claim for a nonenveloped virus (for example, norovirus, rotavirus, adenovirus, poliovirus)4,5 to disinfect environmental surfaces in rooms of PUIs or patients with confirmed EVD. Cleaning and decontaminating surfaces or objects soiled with blood or body fluids are addressed below. There should be the same careful attention to the safety of EMS providers during cleaning and disinfection of transport vehicle as during care of the patient.
- Patient-care surfaces (including stretchers, railings, door handles, medical equipment control panels, and adjacent flooring, walls, and work surfaces), as well as stretcher wheels, brackets, and other areas are likely to become contaminated and should be cleaned and disinfected thoroughly after each transport.
- A blood spill or spill of other body fluids or substances (like urine, saliva, vomit, sweat, and diarrhea) should be managed by personnel wearing correct PPE. This includes removing bulk spill matter, cleaning the soiled site, and then disinfecting the site. For large spills, a chemical disinfectant with sufficient potency is needed to overcome the tendency of proteins in blood and other body substances to neutralize the disinfectant’s active ingredient. Follow the chemical disinfectant product’s labeled instructions and dispose of the potentially contaminated materials used during the cleaning and disinfecting process as recommended in CDC guidance.
- Contaminated reusable patient care equipment (such as glucometer, blood pressure cuff) should be placed in biohazard bags and labeled for cleaning and disinfection or disposal according to agency policies and manufacturer recommendations. Reusable equipment should be cleaned and disinfected according to manufacturer’s instructions by trained personnel wearing correct PPE. Avoid contamination of reusable porous surfaces not designated as single use.
- Use only a mattress and pillow with plastic or other covering that fluids cannot penetrate.
- To reduce exposure among staff to potentially contaminated textiles (cloth products) while laundering, discard used linens and nonfluid-impermeable pillows or mattresses as appropriate at the receiving facility.
Ebola is a Category A infectious substance regulated by the U.S. Department of Transportation’s Hazardous Materials Regulations (HMR, 49 C.F.R., Parts 171-180). Any item transported for disposal that is contaminated or suspected of being contaminated with a Category A infectious substance must be packaged and transported in accordance with the HMR. This includes: disposable medical equipment; sharps; linens; and used health care products such as soiled absorbent pads or dressings, kidney-shaped emesis pans, portable toilets; used PPE such as, gowns or coveralls, masks, gloves, goggles, face shields, respirators, and booties; and byproducts of cleaning contaminated or suspected of being contaminated with a Category A infectious substance.7 EMS systems should work with designated receiving hospitals to dispose of waste from PUIs.
Follow-up and/or Reporting Measures by EMS Providers After Caring for a PUI for EVD
- EMS providers should be aware of the follow-up and/or reporting measures they should take after caring for a PUI.
- EMS agencies should develop policies for monitoring and management of EMS providers potentially exposed to Ebola virus.
- EMS agencies should develop sick-leave policies for EMS providers that are nonpunitive, flexible, and consistent with public health guidance.
- Ensure all EMS providers, including staff who are not directly employed by the healthcare facility but provide essential daily services, are aware of the sick-leave policies.
- EMS providers with exposure to blood, bodily fluids, secretions, or excretions from a PUI should immediately
- Stop working and wash the affected skin surfaces with a cleansing or antiseptic solution, and mucous membranes (such as conjunctiva of the eye) should be irrigated with a large amount of water or eyewash solution, as per usual protocols. All wipes and solution should be placed in a biohazard bag.
- Contact occupational health/supervisor/designated infection control officer for immediate assessment and access to postexposure management services.
- Receive medical evaluation and follow-up care, based upon EMS agency policy and consultation with local, state, and federal public health authorities.
1 2014 Ebola Outbreak in West Africa – Outbreak Distribution Map
2 Ebola Virus Disease (EVD) Information for Clinicians in U.S. Healthcare Settings
3 Case Definition for Ebola Virus Disease (EVD)
4 US Environmental Protection Agency Office of Pesticide Programs, List G: EPA Registered Hospital Disinfectants Effective Against Norovirus (Norwalk-like virus)[PDF- 3 pages]
5 Disinfectants for Use Against the Ebola Virus
6 Occupational Safety and Health Standards
7 FAQ: Department of Transportation Guidance for Transporting Ebola Contaminated Items, a Category A Infectious Substance
- Page last reviewed: December 29, 2015
- Page last updated: December 29, 2015
- Content source:



 ShareCompartir
ShareCompartir