Balloon pulmonary angioplasty
| Balloon pulmonary angioplasty | |
|---|---|
| Other names: BPA | |
 | |
| Specialty | Cardiovascular medicine |
Balloon pulmonary angioplasty (BPA) is an emerging minimally invasive procedure to treat chronic thromboembolic pulmonary hypertension (CTEPH) in people who are not suitable for pulmonary thromboendarterectomy (PTE) or still have residual pulmonary hypertension and areas of narrowing in the pulmonary arterial tree following previous PTE.[1][2]
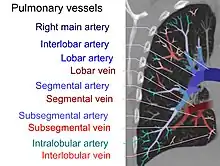
The procedure uses balloons to open pulmonary arteries that have been narrowed or blocked by webs, bands and fibrous tissue[2] and therefore restores blood flow to the lungs, reduces shortness of breath, and improves exercise tolerance. More data on its safety and effectiveness are still required.[3][4]
Medical uses
BPA may be considered in people with symptomatic CTEPH who are not suitable for surgery.[3][5] PTE is an established treatment for CTEPH but is only performed at a few specialist centres, requires surgical competence and intermittent total circulatory arrest under deep hypothermia.[6][7] However, co-existing illnesses and inaccessible clots may contraindicate performing the operation.[6][7] Up to 40% of those diagnosed with CTEPH are considered ineligible for surgery.[6][7] Selection criteria may vary between centres.[1]
Technique
BPA is performed by specialists in a catheterization laboratory. Each procedure takes between two and four hours and most people undergo up to six treatments with the first two sessions being performed a fortnight apart and subsequent treatments being individually tailored upon follow-up assessment.[8]
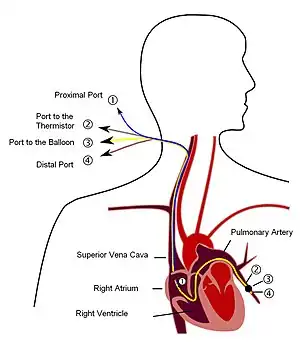
A local anesthetic and moderate sedation are used but a general anaesthetic is not required, hence the person remains awake throughout the procedure. After inserting the catheter into the vein of the neck (right internal jugular vein) or groin (right femoral vein), a hollow tube is introduced through the catheter and passed to the affected blocked lung arteries.[8][7]
X-rays and pressures in the narrowed arteries are assessed by the specialist team before a thin wire with a deflated balloon is guided through the blood vessels to the site of blockage, where the balloon is then inflated.[8] This mainly disrupts the organised thrombus and to a lesser degree presses it against the walls of the arteries.[9] This increases the size of the lumen of the arteries, thus opening them and allowing the blood flow to be restored.[9] The balloon is then deflated and removed.[8] A number of arteries can be treated during each BPA procedure.[8]
Recovery and follow-up
One overnight stay in hospital is usually required. This is followed by a check up appointment within three months.[8] The overall survival has been shown to be comparable with PTE and better than with medication only.[9]
Complications
The pulmonary arteries have thinner walls than the blood vessels of the heart and therefore injury by rupture or dissection caused by over-dilatation of the balloon or piercing pulmonary arteries by the tip of the guide wire, resulting in haemorrhage, are risks.[9] Injury to the lung including reperfusion oedema is also a possibility and these injuries are less likely with more experienced specialists.[9]
History
BPA was originally developed and established for treating children with congenital pulmonary stenosis. Subsequently, it was first tried for the treatment of CTEPH in 1988. Initial results of performing BPA in inoperable CTEPH were reported in 2001, but had a high mortality.[10] Since 2012, reports of the effect of BPA has mainly come from the National Hospital Organization Okayama Medical Center in Japan[9] where the procedure was refined and where smaller balloons were used. In addition, the number of balloon inflations per session were carefully limited to one or two lung vessel segments with targeting only one lung lobe during each session. Intravascular imaging was also introduced.[3]
Research
More data on its safety and effectiveness are still required.[11] Long-term results on disease recurrence, the requirement for stenting and long-term survival also need to be evaluated.[6] In addition, studies to clarify BPA's comparability with the drug riociguat are needed.[5]
See also
References
- 1 2 Auger, William R. (2020). "Surgical and Percutaneous Interventions for Chronic Thromboembolic Pulmonary Hypertension". In Jerry D. Estep (ed.). Right Ventricular Function and Failure, An Issue of Cardiology Clinics. Miriam Jacob. Elsevier. p. 262-264. ISBN 978-0-323-76000-3. Archived from the original on 2022-02-08. Retrieved 2022-02-05.
- 1 2 Brenot, Philippe; Mayer, Eckhard; Ghofrani, Hossein-Ardeschir; Kurzyna, Marcin; Matsubara, Hiromi; Ogo, Takeshi; Meyer, Bernhard C.; Lang, Irene (31 March 2017). "Balloon pulmonary angioplasty in chronic thromboembolic pulmonary hypertension". European Respiratory Review. 26 (143): 160119. doi:10.1183/16000617.0119-2016. ISSN 1600-0617. PMID 28356406.
- 1 2 3 Sirenko, Yuriy; Coghlan, Gerry; Kaymaz, Cihangir; Mahdhaoui, Abdallah; Dijk, Van; J, Arie P.; Srbinovska-Kostovska, Elizabeta; Schwerzmann, Markus; Wikström, Gerhard (2016-01-01). "2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertensionThe Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT)". European Heart Journal. 37 (1): 67–119. doi:10.1093/eurheartj/ehv317. ISSN 0195-668X. PMID 26320113. Archived from the original on 2020-11-25. Retrieved 2022-02-05.
- ↑ Saggar, R.; Kao, S. D.; Khan, S. N.; Moriarty, J. M. (23 July 2018). "Balloon Pulmonary Angioplasty for Chronic Thromboembolic Pulmonary Hypertension". CardioVascular and Interventional Radiology. 41 (12): 1826–1839. doi:10.1007/s00270-018-2012-2. ISSN 1432-086X. PMC 4372623. PMID 30039506.(subscription required)
- 1 2 "Balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension". www.nice.org.uk. 27 April 2016. Archived from the original on 26 December 2018. Retrieved 26 December 2018.
- 1 2 3 4 Ogawa, Aiko; Matsubara, Hiromi (17 February 2015). "Balloon Pulmonary Angioplasty: A Treatment Option for Inoperable Patients with Chronic Thromboembolic Pulmonary Hypertension". Frontiers in Cardiovascular Medicine. 2: 4. doi:10.3389/fcvm.2015.00004. ISSN 2297-055X. PMC 4671397. PMID 26664876.
- 1 2 3 4 Specialised Commissioning Team (April 2018). "Clinical Commissioning Policy: Balloon pulmonary angioplasty for chronic Document Name thromboembolic pulmonary hypertension (all ages)" (PDF). NHS England. Archived (PDF) from the original on 26 December 2018. Retrieved 26 December 2018.
- 1 2 3 4 5 6 "Balloon Pulmonary Angioplasty | UC San Diego Health". UC Health - UC San Diego. Archived from the original on 25 January 2021. Retrieved 24 December 2018.
- 1 2 3 4 5 6 Matsubara, Hiromi; Ogawa, Aiko (2017). "15. Balloon pulmonary hypertension". In Fukumoto, Yoshihiro (ed.). Diagnosis and Treatment of Pulmonary Hypertension: From Bench to Bedside. Springer. p. 193. ISBN 9789812878397. Archived from the original on 2022-02-08. Retrieved 2022-02-05.
- ↑ Matsubara, Hiromi.; Ogawa, Aiko (2016). "49. Balloon Pulmonary Angioplasty". In Peacock, Andrew J.; Naeije, Robert; Rubin, Lewis J. (eds.). Pulmonary Circulation: Diseases and Their Treatment, Fourth Edition. CRC Press. p. 530. ISBN 978-1-4987-1991-9. Archived from the original on 2022-02-08. Retrieved 2022-02-05.
- ↑ Wiedenroth, Christoph B.; Olsson, Karen M.; Guth, Stefan; Breithecker, Andreas; Haas, Moritz; Kamp, Jan-Christopher; Fuge, Jan; Hinrichs, Jan B.; Roller, Fritz (28 December 2017). "Balloon pulmonary angioplasty for inoperable patients with chronic thromboembolic disease". Pulmonary Circulation. 8 (1): 2045893217753122. doi:10.1177/2045893217753122. ISSN 2045-8932. PMC 5798689. PMID 29283044.