Bronchopulmonary dysplasia
| Bronchopulmonary dysplasia | |
|---|---|
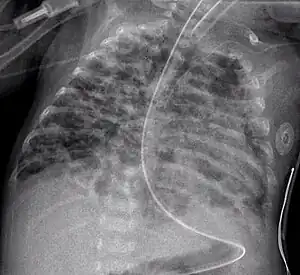 | |
| An X-ray showing bronchopulmonary dysplasia. Person is also intubated and has an oral gastric tube. | |
| Specialty | Pediatrics |
| Symptoms | Increased work of breathing[1] |
| Complications | Trouble feeding, GERD, pulmonary hypertension, delayed speech, heart problems, asthma, infections[2][3] |
| Usual onset | Newborn[3] |
| Duration | Long term[3] |
| Risk factors | Prematurity, prolonged mechanical ventilation or supplemental oxygen, sepsis, chorioamnionitis before birth, mother who smokes[2][3] |
| Diagnostic method | Based on needing respiratory support[2] |
| Prevention | Corticosteroids before birth, surfactant, caffeine, lowest possible supplemental oxygen[3] |
| Treatment | Oxygen therapy, continuous positive airway pressure (CPAP), bronchodilators, diuretics[2] |
| Prognosis | Often improve over few months[2] |
| Frequency | Relatively common[1] |
Bronchopulmonary dysplasia (BPD) is a lung disease in which babies need breathing support 28 days after birth or around the time they would have reached their original due date.[2] Symptoms include increased work of breathing, in the absence of other conditions.[1][3] Complications may include trouble feeding, GERD, pulmonary hypertension, delayed speech, heart problems like patent ductus arteriosus, asthma, and infections.[2][3]
The primary risk factors are prematurity, prolonged mechanical ventilation or supplemental oxygen, sepsis, and chorioamnionitis before birth.[2][3] Other risk factors include a mother who smokes.[3] The underlying mechanism involves incompletely or abnormally developed and fragile lungs.[2] It is a type of newborn breathing condition along with respiratory distress syndrome and meconium aspiration syndrome.[4]
Treatment may involve nutrition, oxygen therapy, continuous positive airway pressure (CPAP), bronchodilators, diuretics, and caffeine.[2][3] An antibody against respiratory syncytial virus (RSV) may also be given.[3] Prevention may include the use of surfactant replacement therapy and corticosteroids before birth.<re name=Mer2022/> Most of those affected gradually improve over two to four months.[2] Some may experience permanent breathing difficulties while other may die as a result.[2][3]
Bronchopulmonary dysplasia is relatively common.[1] About half of those with a birth weight of less than 1,500 grams are affected.[1] Males are more commonly affected than females.[3] The condition was first named in 1967.[1]
Signs and symptoms
Complications
Feeding problems are common in infants with bronchopulmonary dysplasia, often due to prolonged intubation. Such infants often display oral-tactile hypersensitivity (also known as oral aversion).[5]
Physical findings:
- hypoxemia;
- hypercapnia;
- crackles, wheezing, & decreased breath sounds;
- increased bronchial secretions;
- hyperinflation;
- frequent lower respiratory infections;
- delayed growth & development;
- cor pulmonale;
- CXR shows with hyperinflation, low diaphragm, atelectasis, cystic changes.
Cause
Prolonged high oxygen delivery in premature infants causes necrotizing bronchiolitis and alveolar septal injury, with inflammation and scarring. This results in hypoxemia. Today, with the advent of surfactant therapy and high frequency ventilation and oxygen supplementation, infants with BPD experience much milder injury without necrotizing bronchiolitis or alveolar septal fibrosis. Instead, there are usually uniformly dilated acini with thin alveolar septa and little or no interstitial fibrosis. It develops most commonly in the first 4 weeks after birth.
Diagnosis

Earlier criteria
The classic diagnosis of BPD may be assigned at 28 days of life if the following criteria are met:
- Positive pressure ventilation during the first 2 weeks of life for a minimum of 3 days.
- Clinical signs of abnormal respiratory function.
- Requirements for supplemental oxygen for longer than 28 days of age to maintain PaO2 above 50 mm Hg.
- Chest radiograph with diffuse abnormal findings characteristic of BPD.
Newer criteria
The 2006 National Institute of Health (US) criteria for BPD (for neonates treated with more than 21% oxygen for at least 28 days)[6] is as follows:,[7][8]
- Mild
- Breathing room air at 36 weeks' post-menstrual age or discharge (whichever comes first) for babies born before 32 weeks, or
- breathing room air by 56 days' postnatal age, or discharge (whichever comes first) for babies born after 32 weeks' gestation.
- Moderate
- Need for <30% oxygen at 36 weeks' postmenstrual age, or discharge (whichever comes first) for babies born before 32 weeks, or
- need for <30% oxygen to 56 days' postnatal age, or discharge (whichever comes first) for babies born after 32 weeks' gestation.
- Severe
- Need for >30% oxygen, with or without positive pressure ventilation or continuous positive pressure at 36 weeks' postmenstrual age, or discharge (whichever comes first) for babies born before 32 weeks, or
- need for >30% oxygen with or without positive pressure ventilation or continuous positive pressure at 56 days' postnatal age, or discharge (whichever comes first) for babies born after 32 weeks' gestation.
Management
Infants with bronchopulmonary dysplasia are often treated with diuretics that decrease fluid in the alveoli where gas exchange occurs and bronchodilators that relax the airway muscles to facilitate breathing.[9] Viral immunization is important for these children who have a higher risk of infections in the respiratory tract.[10]
Corticosteroids
There is evidence that steroids (systemic corticosteroid treatment) given to babies less than 7 days old can prevent bronchopulmonary dysplasia.[11] This treatment increases the risk of neurodevelopmental sequelae (cerebral palsy) and gastrointestinal perforation.[11]
For babies 7 days old and older, "late systemic postnatal corticosteroid treatment" may reduce the risk of death and of bronchopulmonary dysplasia.[12] There is some evidence that that this treatment does not increase the risk of cerebral palsy, however, long-term studies considering the neurodevelopmental outcomes is needed to further understand the risk of this treatment option.[12] Late systemic postnatal corticosteroid treatment is therefore only recommended for babies 7 days old or older who cannot be taken off of a ventilator.[12] The benefit and risks of systemic corticosteroid treatment in older babies who are not intubated (on a ventilator) is not known.[12]
Vitamin A
Vitamin A treatment in low birth weight babies may improve the 36-week mortality risk, decrease the days of mechanical ventilation, and decrease the incidence of bronchopulmonary dysplasia.[13]
Other
Oxygen therapy at home is recommended in those with significant low oxygen levels.[14]
Hypercarbia (too much carbon dioxide in the blood) may contribute to the development of bronchopulmonary dysplasia.[15] Monitoring the level of carbon dioxide in neonatal infants to ensure that the level is not too high or too low (hypocarbia) is important for improving outcomes for neonates in intensive care.[16] Carbon dioxide can be monitored by taking a blood sample (arterial blood gas), through the breath (exhalation), and it can be measured continuously through the skin by using a minimally invasive transcutaneous device.[16] The most effective and safest approach for measuring carbon dioxide in newborn infants is not clear.[16]
Epidemiology
The rate of BPD varies among institutions, which may reflect neonatal risk factors, care practices (e.g., target levels for acceptable oxygen saturation), and differences in the clinical definitions of BPD.[17][18][19]
See also
References
- 1 2 3 4 5 6 Sahni, M; Mowes, AK (January 2022). "Bronchopulmonary Dysplasia". PMID 30969701.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 5 6 7 8 9 10 11 12 "Newborn Breathing Conditions - Bronchopulmonary Dysplasia (BPD) | NHLBI, NIH". www.nhlbi.nih.gov. Archived from the original on 9 May 2022. Retrieved 20 June 2022.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 "Bronchopulmonary Dysplasia (BPD) - Pediatrics". Merck Manuals Professional Edition. Archived from the original on 20 June 2022. Retrieved 20 June 2022.
- ↑ "Newborn Breathing Conditions - What Are Newborn Breathing Conditions? | NHLBI, NIH". www.nhlbi.nih.gov. Archived from the original on 20 June 2022. Retrieved 20 June 2022.
- ↑ Gaining & Growing. "Bronchopulmonary dysplasia" Archived 2021-05-07 at the Wayback Machine, Gaining & Growing, March 20, 2007. (Retrieved June 12, 2008.)
- ↑ Kinsella, JP; Greenough, A; Abman, SH (Apr 29, 2006). "Bronchopulmonary dysplasia". Lancet. 367 (9520): 1421–31. doi:10.1016/S0140-6736(06)68615-7. PMID 16650652. S2CID 23716814.
- ↑ "Bronchopulmonary Dysplasia". Patient.info. Archived from the original on 20 August 2021. Retrieved 2 February 2014.
- ↑ Jobe, AH; Bancalari, E (June 2001). "Bronchopulmonary dysplasia". Am J Respir Crit Care Med. 163 (7): 1723–9. doi:10.1164/ajrccm.163.7.2011060. PMID 11401896.
- ↑ American Lung Association Scientific; Medical Editorial Review Panel. "Diagnosing and Treating Bronchopulmonary Dysplasia". American Lung Association. Archived from the original on 23 October 2021. Retrieved 4 December 2020.
- ↑ American Lung Association Scientific; Medical Editorial Review Panel. "Diagnosing and Treating Bronchopulmonary Dysplasia". American Lung Association. Archived from the original on 23 October 2021. Retrieved 4 December 2020.
- 1 2 Doyle, Lex W.; Cheong, Jeanie L.; Hay, Susanne; Manley, Brett J.; Halliday, Henry L. (2021-10-21). "Early (< 7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants". The Cochrane Database of Systematic Reviews. 10: CD001146. doi:10.1002/14651858.CD001146.pub6. ISSN 1469-493X. PMC 8530019. PMID 34674229.
- 1 2 3 4 Doyle, Lex W.; Cheong, Jeanie L.; Hay, Susanne; Manley, Brett J.; Halliday, Henry L. (2021-11-11). "Late (≥ 7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants". The Cochrane Database of Systematic Reviews. 11: CD001145. doi:10.1002/14651858.CD001145.pub5. ISSN 1469-493X. PMC 8580679. PMID 34758507.
- ↑ Huang, Li; Zhu, Diqing; Pang, Gaofeng (2021). "The effects of early vitamin A supplementation on the prevention and treatment of bronchopulmonary dysplasia in premature infants: a systematic review and meta-analysis". Translational Pediatrics. 10 (12): 3218–3229. doi:10.21037/tp-21-496. ISSN 2224-4344. PMC 8753470. PMID 35070836. Archived from the original on 2022-03-24. Retrieved 2022-03-24.
- ↑ Hayes D, Jr; Wilson, KC; Krivchenia, K; Hawkins, SMM; Balfour-Lynn, IM; Gozal, D; Panitch, HB; Splaingard, ML; Rhein, LM; Kurland, G; Abman, SH; Hoffman, TM; Carroll, CL; Cataletto, ME; Tumin, D; Oren, E; Martin, RJ; Baker, J; Porta, GR; Kaley, D; Gettys, A; Deterding, RR (1 February 2019). "Home Oxygen Therapy for Children. An Official American Thoracic Society Clinical Practice Guideline". American Journal of Respiratory and Critical Care Medicine. 199 (3): e5–e23. doi:10.1164/rccm.201812-2276ST. PMC 6802853. PMID 30707039.
- ↑ Hochwald, Ori; Borenstein-Levin, Liron; Dinur, Gil; Jubran, Huda; Ben-David, Shlomit; Kugelman, Amir (July 2019). "Continuous Noninvasive Carbon Dioxide Monitoring in Neonates: From Theory to Standard of Care". Pediatrics. 144 (1). doi:10.1542/peds.2018-3640. ISSN 1098-4275. PMID 31248940.
- 1 2 3 Bruschettini, Matteo; Romantsik, Olga; Zappettini, Simona; Ramenghi, Luca Antonio; Calevo, Maria Grazia (2016-02-13). "Transcutaneous carbon dioxide monitoring for the prevention of neonatal morbidity and mortality". The Cochrane Database of Systematic Reviews. 2: CD011494. doi:10.1002/14651858.CD011494.pub2. ISSN 1469-493X. PMID 26874180.
- ↑ Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, et al. (2007). "Trends in neonatal morbidity and mortality for very low birthweight infants". Am J Obstet Gynecol. 196 (2): 147.e1–8. doi:10.1016/j.ajog.2006.09.014. PMID 17306659. S2CID 27489509.
- ↑ Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M, et al. (2000). "Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network". Pediatrics. 105 (6): 1194–201. doi:10.1542/peds.105.6.1194. PMID 10835057.
- ↑ Ellsbury DL, Acarregui MJ, McGuinness GA, Eastman DL, Klein JM (2004). "Controversy surrounding the use of home oxygen for premature infants with bronchopulmonary dysplasia". J Perinatol. 24 (1): 36–40. doi:10.1038/sj.jp.7211012. PMID 14726936.
External links
| Classification | |
|---|---|
| External resources |
|
- Bhandari, A; Bhandari, V (Jan 2007). "Bronchopulmonary dysplasia: an update". Indian Journal of Pediatrics. 74 (1): 73–7. doi:10.1007/s12098-007-0032-z. PMID 17264460. S2CID 36330658. Archived from the original on 2022-05-15. Retrieved 2022-03-24.
- Bronchopulmonary Dysplasia Archived 2017-11-10 at the Wayback Machine on National Institutes of Health