Mycoplasma hominis infection
| Mycoplasma hominis infection | |
|---|---|
| Specialty | Infectious disease |
The exact role of Mycoplasma hominis (and to a lesser extent Ureaplasma) in regards to a number of conditions related to pregnant women and their (unborn) offspring is controversial. This is mainly because many healthy adults have genitourinary colonization with Mycoplasma, published studies on pathogenicity have important design limitations and the organisms are very difficult to detect.[1] The likelihood of colonization with M. hominis appears directly linked to the number of lifetime sexual partners[2] Neonatal colonization does occur, but only through normal vaginal delivery. Caesarean section appears protective against colonization and is much less common. Neonatal colonization is transient.[3]
Signs and symptoms
Those with urogenital or extragenital infections caused by M. hominis have symptoms similar to other sexually transmitted infections and its presence cannot be determined by its symptoms. The precise role this organism plays in causing disease remains speculative.[4] Diagnosis remains a challenge because the organism is difficult to culture in vitro. PCR-based techniques are still rare outside research scenarios.[5] The following conditions have been linked to Mycoplasma hominis:
- Pyelonephritis
- Cystitis
- Pelvic inflammatory disease (PID)
- Endometritis
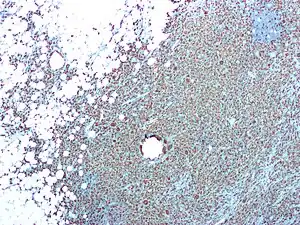
- Chorioamnionitis
- surgical and nonsurgical wound infections
- Bacteremia
- Pneumonia
- Meningitis
- Salpingitis
- Urethritis
- Septic arthritis
- Cervicitis
Mycoplasma hominis is often present in polymicrobial infections.[6]
Neonatal infection
Neonates, especially if preterm, are susceptible to M. hominis infection.[7] Meningoencephalitis in neonates has been described and M. hominis may be a significant causative agent of neonatal sepsis or meningitis.[8] M. hominis has been associated with chorioamnionits.[9] M. hominis is associated with miscarriage.[10]
Diagnosis

In terms of the diagnosis of Mycoplasma hominis infection, it can be done via culture or PCR[11][12]
Prevention
If symptomatic, testing is recommended.[13] The risk of contracting Mycoplasma infection can be reduced by the following:
- Using barrier methods such as condoms
- Seeking medical attention if you are experiencing symptoms suggesting a sexually transmitted infection.
- Seeking medical attention after learning that a current or former sex partner has, or might have had a sexually transmitted infection.
- Getting a STI history from your current partner and insisting they be tested and treated before intercourse.
- Avoiding vaginal activity, particularly intercourse, after the end of a pregnancy (delivery, miscarriage, or abortion) or certain gynecological procedures, to ensure that the cervix closes.
- Abstinence[14]
Treatment
Mycoplasmas have a triple-layered membrane and lack a cell wall. Therefore, mycoplasmas are not affected by penicillins and other antibiotics that interfere with the cell wall synthesis. The growth of mycoplasmas in their host is inhibited by other broad-spectrum antibiotics. These broad-spectrum antibiotics inhibit the multiplication of the mycoplasma but does not kill them. Tetracyclines, macrolides, ketolides, quinolones are used to treat mycoplasma infections. In addition to the penicillins, mycoplasmas are resistant to rifampicin. Mycoplasmas may be difficult to eradicate from human or animal hosts or from cell cultures by antibiotic treatment because of resistance to the antibiotic, or because it does not kill the mycoplasma cell. Mycoplasma cells are able to invade the cells of their hosts.[15]
References
- ↑ Waites, KB; Schelonka, RL; Xiao, L; Grigsby, PL; Novy, MJ (August 2009). "Congenital and opportunistic infections: Ureaplasma species and Mycoplasma hominis". Seminars in Fetal & Neonatal Medicine. 14 (4): 190. doi:10.1016/j.siny.2008.11.009. PMID 19109084.
- ↑ McCormack, WM; Almeida, PC; Bailey, PE; Grady, EM; Lee, YH (18 September 1972). "Sexual activity and vaginal colonization with genital mycoplasmas". JAMA. 221 (12): 1375–7. doi:10.1001/jama.1972.03200250017004. PMID 5068553.
- ↑ Foy, HM; Kenny, GE; Levinsohn, EM; Grayston, JT (June 1970). "Acquisition of mycoplasmata and T-strains during infancy". The Journal of Infectious Diseases. 121 (6): 579–87. doi:10.1093/infdis/121.6.579. PMID 4912072.
- ↑ Waites, KB; Schelonka, RL; Xiao, L; Grigsby, PL; Novy, MJ (August 2009). "Congenital and opportunistic infections: Ureaplasma species and Mycoplasma hominis". Seminars in Fetal & Neonatal Medicine. 14 (4): 190. doi:10.1016/j.siny.2008.11.009. PMID 19109084.
- ↑ Degré, SG; Fang, ZY; Sobolski, J; Abramowicz, M; Unger, P; Berkenboom, G (1990). Detection of silent myocardial ischemia in asymptomatic selected population and in unstable angina. Advances in Cardiology. Vol. 37. pp. 215–22. doi:10.1159/000418829. ISBN 978-3-8055-5196-0. PMID 2120910.
- ↑ "Ureaplasma Infection Clinical Presentation: History, Physical, Causes". Archived from the original on 2015-06-21. Retrieved 2015-06-21.
- ↑ Goldenberg, RL; Andrews, WW; Goepfert, AR; Faye-Petersen, O; Cliver, SP; Carlo, WA; Hauth, JC (January 2008). "The Alabama Preterm Birth Study: umbilical cord blood Ureaplasma urealyticum and Mycoplasma hominis cultures in very preterm newborn infants". American Journal of Obstetrics and Gynecology. 198 (1): 43.e1–5. doi:10.1016/j.ajog.2007.07.033. PMC 2278008. PMID 18166302.
- ↑ Waites, K.B. (1990). "Mycoplasma infections of the central nervous system in humans and animals". Zentralblatt für Bakteriologie: Suplement.
- ↑ Romero, R; Garite, TJ (January 2008). "Twenty percent of very preterm neonates (23-32 weeks of gestation) are born with bacteremia caused by genital Mycoplasmas". American Journal of Obstetrics and Gynecology. 198 (1): 1–3. doi:10.1016/j.ajog.2007.11.031. PMID 18166295.
- ↑ Cunningham, F, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL, Casey BM, Sheffield JS (2013). "Abortion". Williams Obstetrics. McGraw-Hill. p. 5.
- ↑ Ozturk, Sukran; Yildiz, Sulhiye; Dursun, Polat; Yener Ilce, Burcu; Kaymaz, Ozlem (October 2019). "Mycoplasma hominis profile in women: Culture, kit, molecular diagnosis, antimicrobial resistance, and treatment". Microbial Pathogenesis. 135: 103635. doi:10.1016/j.micpath.2019.103635. ISSN 1096-1208. Archived from the original on 15 September 2022. Retrieved 27 August 2022.
- ↑ Ahmed, Jaweed; Rawre, Jyoti; Dhawan, Neha; Khanna, Neena; Dhawan, Benu (January 2021). "Mycoplasma hominis: An under recognized pathogen". Indian Journal of Medical Microbiology. 39 (1): 88–97. doi:10.1016/j.ijmmb.2020.10.020. ISSN 1998-3646. Archived from the original on 15 September 2022. Retrieved 27 August 2022.
- ↑ Smith KJ, Cook RL, Roberts MS (2007). "Time from sexually transmitted infection acquisition to pelvic inflammatory disease development: influence on the cost-effectiveness of different screening intervals". Value in Health. 10 (5): 358–66. doi:10.1111/j.1524-4733.2007.00189.x. PMID 17888100.
- ↑ "Prevention - STD Information from CDC". Center For Disease Control. Archived from the original on 2014-12-09. Retrieved 2015-02-21.
- ↑ Taylor-Robinson, D (1997). "Antibiotic susceptibilities of mycoplasmas and treatment of mycoplasmal infections". Journal of Antimicrobial Chemotherapy. 40 (5): 622–630. doi:10.1093/jac/40.5.622. ISSN 1460-2091. PMID 9421309.
External links
| Classification | |
|---|---|
| External resources |