Granuloma inguinale
| Granuloma inguinale | |
|---|---|
| Other names: Granuloma inguinale tropicum, granuloma genitoinguinale, granuloma venereum, lupoid form of groin ulceration, serpiginous ulceration of the groin, ulcerating granuloma of the pudendum, ulcerating sclerosing granuloma[1] | |
.jpg.webp) | |
| Genital ulcers of granuloma inguinale | |
| Specialty | Infectious diseases |
| Treatment | Antibiotics for 3 or more weeks, no sex for 3 weeks, treat partners[2] |
| Medication | Azithromycin 500 milligrams/day or 1 gram/week, or doxycycline 100 milligrams twice daily[2] |
Granuloma inguinale, also known Donovanosis, is a bacteria infection caused by Klebsiella granulomatis, which results in genital ulcers.[2]
It is endemic in many less-developed regions.[2] Oral manifestations are also notably seen . The lesions of oral cavity are usually secondary to active genital lesions.
The disease often goes untreated because of the scarcity of medical treatment in the countries in which it is found. In addition, the painless genital ulcers can be mistaken for syphilis.[3] The ulcers ultimately progress to destruction of internal and external tissue, with extensive leakage of mucus and blood from the highly vascular lesions. The destructive nature of donovanosis also increases the risk of superinfection by other pathogenic microbes.
Symptoms and signs
Small, painless nodules appear after about 10–40 days of contact with the bacteria. Later, the nodules burst, creating open, fleshy, oozing lesions. The infection spreads, mutilating the infected tissue. The infection will continue to destroy the tissue until treated. The lesions occur at the region of contact typically found on the shaft of the penis, the labia, or the perineum. Rarely, the vaginal wall or cervix is the site of the lesion. At least one case in India led to partial autoamputation of the penis. The patient tested positive for HIV-2 and had been infected for six years.[4]
Mechanism
The microorganism spreads from one host to another through contact with the open sores.[5]
Diagnosis
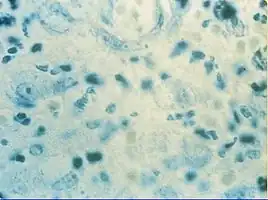
The diagnosis is based on the patient's sexual history and on physical examination revealing a painless, "beefy-red ulcer" with a characteristic rolled edge of granulation tissue. In contrast to syphilitic ulcers, inguinal lymphadenopathy is generally mild or absent. Tissue biopsy and Wright-Giemsa stain are used to aid in the diagnosis. The presence of Donovan bodies in the tissue sample confirms donovanosis. Donovan bodies are rod-shaped, oval organisms that can be seen in the cytoplasm of mononuclear phagocytes or histiocytes in tissue samples from patients with granuloma inguinale.[6]
They appear deep purple when stained with Wright's stain.[6] These intracellular inclusions are the encapsulated Gram-negative rods of the causative organisms.[6] They were discovered by Charles Donovan.[7]
Classification
The first known name for this condition was "serpiginous ulcer", which dates to 1882.[8][9] The proper clinical designation for donovanosis is "granuloma inguinale".[3] A granuloma is a nodular type of inflammatory reaction, and inguinale refers to the inguinal region, which is commonly involved in this infection. The disease is commonly known as donovanosis, after the Donovan bodies seen on microscopy, which are a diagnostic sign.[10]
The causative organism, Klebsiella granulomatis, was called Calymmatobacterium granulomatis, and some sources still use this classification,[11][12] from the Greek kalymma (a hood or veil), referring to the lesions that contain the bacteria. Prior to this, it was called Donovania granulomatis, named after the Donovan bodies.[3]
The specific name granulomatis refers to the granulomatous lesions. The organism was recently reclassified under the genus Klebsiella,[13] a drastic taxonomic change since it involved changing the organism's phylum. However, polymerase chain reaction techniques using a colorimetric detection system showed a 99% similarity with other species in the genus Klebsiella.[14] The clinical appearances of this lesion orally are classified into three types: Ulcerative, exuberant, cicatricial.[15]
Prevention
The disease is effectively treated with antibiotics, therefore, developed countries have a very low incidence of donovanosis; about 100 cases reported each year in the United States. However, sexual contact with individuals in endemic regions dramatically increases the risk of contracting the disease. Using condoms, sexually transmitted disease testing before beginning a sexual relationship, and avoidance of these sexual contacts are effective preventative measures for donovanosis.[16]
Treatment
Recommended regimen is azithromycin 1 gram oral/iv once per week, alternatively doxycycline 100 mg orally twice a day or ciprofloxacin 750 mg orally twice a day or erythromycin base 500 mg orally four times a day or trimethoprim-sulfamethoxazole one double-strength (160 mg/800 mg) tablet orally twice a day. All antibiotic regimens should last for at least 3 weeks and until all lesions have completely healed. Normally, the infection will begin to subside within a week of treatment, but the full treatment period must be followed to minimize the possibility of relapse.
The CDC 2015 guidelines give azithromycin as the antibiotic of choice.[17]
See also
References
- ↑ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- 1 2 3 4 Wilson, Janet D.; Anderson, Jane (2020). "37. Sexually transmitted infections and human immunodeficiency virus". In Feather, Adam; Randall, David; Waterhouse, Mona (eds.). Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. p. 1425. ISBN 978-0-7020-7870-5. Archived from the original on 2023-11-10. Retrieved 2023-11-09.
- 1 2 3 Murray, Patrick R; Rosenthal, Ken S; Pfaller, Michael A (2005). Medical Microbiology (5th ed.). Philadelphia: Elsevier Mosby. p. 336. ISBN 978-0-323-03303-9.
- ↑ Chandra Gupta TS, Rayudu T, Murthy SV (2008). "Donovanosis with auto-amputation of penis in a HIV-2 infected person". Indian J Dermatol Venereol Leprol. 74 (5): 490–2. doi:10.4103/0378-6323.44308. PMID 19052412.
- ↑ "Granuloma Inguinale (Donovanosis)". Archived from the original on 2021-03-19. Retrieved 2021-07-12.
- 1 2 3 thefreedictionary.com > Donovan bodies Archived 2017-05-19 at the Wayback Machine Retrieved on Nov 29, 2009
- ↑ Donovan, C. (1905). "Ulcerating Granuloma of the Pudenda". Ind Med Gaz. 40 (11): 414–418. PMC 5162824. PMID 29004684.
- ↑ Rashid RM, Janjua SA, Khachemoune A (2006). "Granuloma inguinale: a case report". Dermatol. Online J. 12 (7): 14. PMID 17459300. Archived from the original on 2013-06-19. Retrieved 2021-07-12.
- ↑ McLeod K. (1882). "Precis of operations performed in the wards of the first surgeon, Medical College Hospital, during the year 1881". Ind Med Gaz. 11 (5): 113–119. PMC 5136093. PMID 28997806.
- ↑ Santiago-Wickey JN, Crosby B, Inguinale G. "Granuloma Inguinale". National Center for Biotechnology Information, U.S. National Library of Medicine. Archived from the original on 28 August 2021. Retrieved 12 July 2021.
- ↑ "granuloma inguinale" at Dorland's Medical Dictionary
- ↑ O'Farrell N (December 2002). "Donovanosis". Sex Transm Infect. 78 (6): 452–7. doi:10.1136/sti.78.6.452. PMC 1758360. PMID 12473810.
- ↑
- Boye K, Hansen DS (February 2003). "Sequencing of 16S rDNA of Klebsiella: taxonomic relations within the genus and to other Enterobacteriaceae". Int. J. Med. Microbiol. 292 (7–8): 495–503. doi:10.1078/1438-4221-00228. PMID 12635932.
- ↑ Carter JS, Bowden FJ, Bastian I, Myers GM, Sriprakash KS, Kemp DJ (October 1999). "Phylogenetic evidence for reclassification of Calymmatobacterium granulomatis as Klebsiella granulomatis comb. nov". Int. J. Syst. Bacteriol. 49 (Pt 4): 1695–700. doi:10.1099/00207713-49-4-1695. PMID 10555350.
- ↑ "Donovanosis". The Lecturio Medical Concept Library. Archived from the original on 12 July 2021. Retrieved 12 July 2021.
- ↑ "Granuloma Inguinale". MSD. Archived from the original on 12 July 2021. Retrieved 12 July 2021.
- ↑ "Granuloma Inguinale (Donovanosis) - 2015 STD Treatment Guidelines". www.cdc.gov. Archived from the original on 2021-03-19. Retrieved 2018-08-23.
External links
| Classification | |
|---|---|
| External resources |
.jpg.webp)