Rhinoscleroma
| Rhinoscleroma | |
|---|---|
| Other names: Scleroma | |
 | |
| Photogravure of rhinoscleroma from Wolkowitsch. | |
Rhinoscleroma, is a chronic granulomatous bacterial disease of the nose that can sometimes infect the upper respiratory tract.[1] It most commonly affects the nasal cavity—the nose is involved in 95–100 per cent of cases—however, it can also affect the nasopharynx, larynx, trachea, and bronchi. Slightly more females than males are affected and patients are usually 10 to 30 years of age. Rhinoscleroma is considered a tropical disease and is mostly endemic to North Africa, South Asia and Central America, less common in the United States.
Signs and symptoms

Rhinoscleroma has been divided into 3 stages: catarrhal/atrophic, granulomatous, and sclerotic stages. The catarrhal stage begins with a nonspecific rhinitis, which progresses into purulent, fetid rhinorrhea, and crusting, which can last for weeks or even months. The granulomatous stage results in the development of a bluish red nasal mucosa and the development of intranasal rubbery nodules or polyps. Nose bleeds, nasal deformity, and destruction of the nasal cartilage are also noted (Hebra nose). The damage may result in anesthesia of the soft palate, enlargement of the uvula, dysphonia, and various degrees of airway obstruction. The fibrotic stage is characterized by sclerosis and fibrosis. Lymphadenitis is absent.
Causes
It is caused by Klebsiella rhinoscleromatis—subspecies of Klebsiella pneumoniae— a gram-negative, encapsulated, nonmotile, rod-shaped bacillus (diplobacillus), member of the family Enterobacteriaceae. It is sometimes referred to as the "Frisch bacillus," named for Anton von Frisch who identified the organism in 1882.[2] It is contracted directly by droplets or by contamination of material that is subsequently inhaled.[1]
Diagnosis
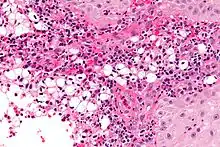
A positive culture in MacConkey agar is diagnostic, but cultures are only positive in 50–60% of cases. Diagnostic characteristics are most commonly found in the granulomatous stage and are described as being plasma cells with birefringent inclusions, Russell bodies, pseudoepitheliomatous hyperplasia, and groups of large vacuolated histiocytes containing Klebsiella rhinoscleromatis (Mikulicz cells).
Treatment
It is not lethal in nature and is responsive to tetracycline or ciprofloxacin. Surgical treatment include rhinoplasty. However, if left untreated the disease can lead to sepsis, bleeding, or other chronic conditions that can be fatal.
History
Hans von Hebra (1847–1902) wrote the classical description of the disease in a paper published in the January 1870 issue of the Wiener Medizinische Wochenschrift.[3][4] Hans von Hebra was the son of Czech born dermatologist Ferdinand Ritter von Hebra (1816–1880), founder of the New Vienna School of Dermatology. He was assisted by M. Kohn who provided much of the histology for the paper. M. Kohn is the birth name of Moritz Kaposi (1837–1902). In 1876, Mikulicz contributed to the microscopic histology. In 1882, Anton Von Frisch (1849–1917) discovered the gram-negative bacillus which causes the disease.[5]
Terminology
Hebra nose. Scleroma. Fr: Sclérome. Sp: Rinoscleroma. Ger: Sklerom. Nasen-Rachenrauminduration.
Archaic terms include: Syphilis of the nose. Nasal leprosy. Scleroma neonatorum. Scleroma respiratorum. Scrofulous lupus.[6]
See also
Notes
References
- DiBartolomeo, Joseph R. (1976), Scleroma of the nose and pharynx. Journal: West. J. Med., vol. 124., pp. 13–17.
- Frisch, Anton von (1882), Zur Aetiologie des Rhinoskleroms. Journal: Wiener Medizinische Wochenschrift; vol. 32, pp. 969–972.
- Hebra, Hans von (1870), Ueber ein eigenthümliches Neugebilde an der Nase; Rhinosclerom; nebst histologischem Befunde vom Dr. M. Kohn. Journal: Wiener Medizinische Wochenschrift; vol. 20, pp. 1–5.
- Morton, Leslie T. (1970), A medical bibliography (Garrison and Morton). Philadelphia & Toronto: J. B. Lippincott Company, p. 388.
- Palmer, P. E. S. & Reeder, M. M. (2000), The imaging of tropical diseases. Heidelberg: Springer Verlach; vols. 1 & 2 (ISBN 3-540-66219-7).
External links
| Classification | |
|---|---|
| External resources |
- DiBartolomeo, Scleroma of the nose and pharynx. Archived 2021-08-29 at the Wayback Machine