Pyomyositis
| Pyomyositis | |
|---|---|
| Other names: Tropical pyomyositis or Myositis tropicans | |
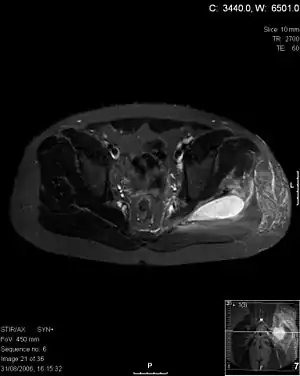 | |
| Transverse T2 magnetic resonance imaging section through the hip region showing abscess collection in a patient with pyomyositis. | |
| Diagnostic method | Diagnostic method used for PM includes ultrasound, CT scan and MRI. Ultrasound can be helpful in showing muscular heterogeneity or a purulent collection but it is not useful during the first stage of the disease. CT scan can confirm the diagnosis before abscesses occur with enlargement of the involved muscles and hypodensity when abscess is present, terogenous attenuation and fluid collection with rim enhancement can be found. MRI is useful to assess PM and determine its localization and extension |
Pyomyositis is a bacterial infection of the skeletal muscles which results in an abscess. Pyomyositis is most common in tropical areas but can also occur in temperate zones.
Signs and symptoms

The clinical presentation of pyomyositis is as follows:[1]
- Pain in affected muscle
- Fever
- Abscess formation
Risk factors
In terms of factors that may place an individual at risk of developing pyomyositis we find:[1]
- Muscle trauma
- Infected insect bites
- Diabetes
- Illicit drug injections
- Connective tissue disorders
Diagnosis
Diagnosis is done via the following manner:
- Pus discharge culture and sensitivity
- X ray of the part to rule out osteomyelitis
- Creatinine phosphokinase (more than 50,000 units)
- MRI is useful
- Ultrasound guided aspiration
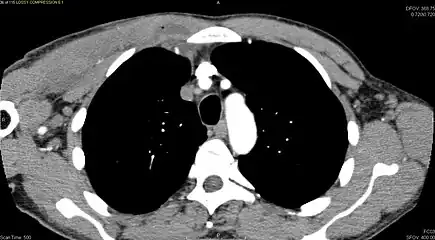 CT with IV contrast showing enlargement and heterogeneous hypodensity in the right pectoralis major muscle. A focal abscess collection with gas within it is present medially. There are enlarged axillary lymph nodes and some extension into the right hemithorax. Note the soft tissue and phlegmon surrounding the right internal mammary artery and vein. The patient was HIV+ and the pyomyositis is believed to be due to direct inoculation of the muscle related to parenteral drug abuse. The patient admitted to being a "pocket shooter"
CT with IV contrast showing enlargement and heterogeneous hypodensity in the right pectoralis major muscle. A focal abscess collection with gas within it is present medially. There are enlarged axillary lymph nodes and some extension into the right hemithorax. Note the soft tissue and phlegmon surrounding the right internal mammary artery and vein. The patient was HIV+ and the pyomyositis is believed to be due to direct inoculation of the muscle related to parenteral drug abuse. The patient admitted to being a "pocket shooter"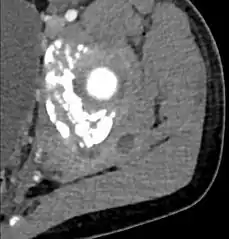 CT exam showing a multiloculated fluid collection in the left gluteus minimus muscle found to be a staph aureus pyomyositis in a 12-year-old healthy boy.
CT exam showing a multiloculated fluid collection in the left gluteus minimus muscle found to be a staph aureus pyomyositis in a 12-year-old healthy boy.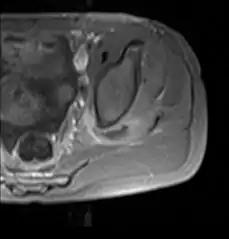 Axial T1 weighted fat suppressed post IV gadolinium contrast enhanced MRI image showing a mutliloculated bacterial abscess in the left gluteal muscle which grew Staphylococcus aureus (methicillin sensitive) thought to be due to tropical pyomyositis.
Axial T1 weighted fat suppressed post IV gadolinium contrast enhanced MRI image showing a mutliloculated bacterial abscess in the left gluteal muscle which grew Staphylococcus aureus (methicillin sensitive) thought to be due to tropical pyomyositis.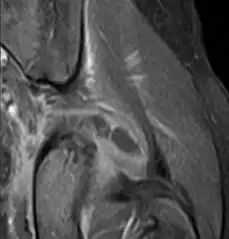 Coronal fat suppressed post contrast image showing a multiloculated bacterial abscess in the left gluteus minimus muscle due to tropical pyomyositis.
Coronal fat suppressed post contrast image showing a multiloculated bacterial abscess in the left gluteus minimus muscle due to tropical pyomyositis.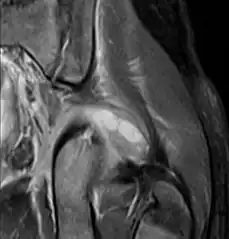 Coronal T2 weighted fat suppressed image showing a multiloculated fluid collection in the left gluteal musculature due to tropical pyomositis in a 12-year-old boy.
Coronal T2 weighted fat suppressed image showing a multiloculated fluid collection in the left gluteal musculature due to tropical pyomositis in a 12-year-old boy.
Treatment
The abscesses within the muscle must be drained surgically (not all patient require surgery if there is no abscess). Antibiotics are given for a minimum of three weeks to clear the infection.[2]
Epidemiology
Pyomyositis is most often caused by the bacterium Staphylococcus aureus.[3] The infection can affect any skeletal muscle, but most often infects the large muscle groups such as the quadriceps or gluteal muscles.[2][4][5]
Pyomyositis is mainly a disease of children and was first described by Scriba in 1885. Most patients are aged 2 to 5 years, but infection may occur in any age group.[6][7] Infection often follows minor trauma and is more common in the tropics, where it accounts for 4% of all hospital admissions. In temperate countries such as the US, pyomyositis was a rare condition (accounting for 1 in 3000 pediatric admissions), but has become more common since the appearance of the USA300 strain of MRSA.[2][4][5]
Gonococcal pyomyositis is a rare infection caused by Neisseria gonorrhoeae.[8]
References
- 1 2 "Pyomyositis - National Organization for Rare Disorders". rarediseases.org. 16 June 2022. Archived from the original on 5 February 2023. Retrieved 5 February 2023.
- 1 2 3 Pannaraj PS, Hulten KG, Gonzalez BE, Mason EO Jr, Kaplan SL (2006). "Clin Infect Dis". Clinical Infectious Diseases. 43 (8): 953–60. doi:10.1086/507637. PMID 16983604.
- ↑ Chauhan S, Jain S, Varma S, Chauhan SS (2004). "Tropical pyomyositis (myositis tropicans): current perspective". Postgrad Med J. 80 (943): 267–70. doi:10.1136/pgmj.2003.009274. PMC 1743005. PMID 15138315. Archived from the original on 2019-12-11. Retrieved 2022-08-14.
- 1 2 Ovadia D, Ezra E, Ben-Sira L, et al. (2007). "Primary pyomyositis in children: a retrospective analysis of 11 cases". J Pediatr Orthop B. 16 (2): 153–159. doi:10.1097/BPB.0b013e3280140548. PMID 17273045.
- 1 2 Mitsionis GI, Manoudis GN, Lykissas MG, et al. (2009). "Pyomyositis in children: early diagnosis and treatment". J Pediatr Surg. 44 (11): 2173–178. doi:10.1016/j.jpedsurg.2009.02.053. PMID 19944229.
- ↑ Small LN, Ross JJ (2005). "Tropical and temperate pyomyositis". Infect Dis Clin North Am. 19 (4): 981–989. doi:10.1016/j.idc.2005.08.003. PMID 16297743.
- ↑ Taksande A, Vilhekar K, Gupta S (2009). "Primary pyomyositis in a child". Int J Infect Dis. 13 (4): e149–e151. doi:10.1016/j.ijid.2008.08.013. PMID 19013093.
- ↑ Jensen M (2021). "Neisseria gonorrhoeae pyomyositis complicated by compartment syndrome: A rare manifestation of disseminated gonococcal infection". IDCases. 23: e00985. doi:10.1016/j.idcr.2020.e00985. PMC 7695882. PMID 33294370.
- Maravelas R, Melgar TA, Vos D, Lima N, Sadarangani S (2020). "Pyomyositis in the United States 2002-2014". J Infect. 80(5):497-503. doi:10.1016/j.jinf.2020.02.005. PMID 32147332.
External links
| Classification | |
|---|---|
| External resources |
|