Escherichia coli O157:H7
| Escherichia coli O157:H7 | |
|---|---|
 | |
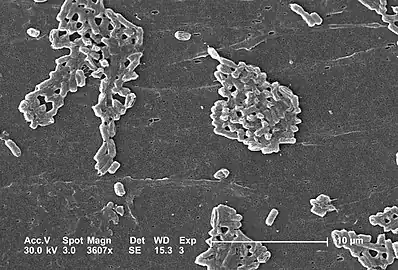
| Topographical images of colonies of E. coli O157:H7 strains (A) 43895OW (curli non-producing) and (B) 43895OR (curli producing) grown on agar for 48 h at 28°C. | |
| Specialty | Infectious disease |
| Symptoms | Severe, acute hemorrhagic diarrhea and abdominal cramps. |
| Duration | Illness resolves in 5 to 10 days |
| Causes | E. coli |
| Diagnostic method | Stool culture can detect the bacterium |
| Treatment | Fluid replacement and blood pressure support |
Escherichia coli O157:H7 is a serotype of the bacterial species Escherichia coli and is one of the Shiga-like toxin–producing types of E. coli. It is a cause of disease, typically foodborne illness, through consumption of contaminated and raw food, including raw milk and undercooked ground beef.[1][2] Infection with this type of pathogenic bacteria may lead to hemorrhagic diarrhea, and to kidney failure; these have been reported to cause the deaths of children younger than five years of age, and of elderly patients.[3]
Transmission is via the fecal–oral route, and most illness has been through distribution of contaminated raw leaf green vegetables, undercooked meat and raw milk.[4]
Signs and symptoms
E. coli O157:H7 infection often causes severe, acute hemorrhagic diarrhea (although nonhemorrhagic diarrhea is also possible) and abdominal cramps. Usually little or no fever is present, and the illness resolves in 5 to 10 days.[5] It can also sometimes be asymptomatic.[6]
In some people, particularly children under five years of age, persons whose immunologies are otherwise compromised, and the elderly, the infection can cause hemolytic uremic syndrome (HUS), in which the red blood cells are destroyed and the kidneys fail, about 10% of infections lead to this complication. HUS is one of the principal cause of acute kidney failure in children, and most cases of HUS are caused by E. coli O157:H7.[3][7]
Bacteriology
 Escherichia coli is a Gram-negative bacterium that normally colonizes the digestive tract of most warm-blooded animals.One strain of E. coli, O157:H7, causes an estimated 73,000 cases of infection, and 61 deaths in the United States each year
Escherichia coli is a Gram-negative bacterium that normally colonizes the digestive tract of most warm-blooded animals.One strain of E. coli, O157:H7, causes an estimated 73,000 cases of infection, and 61 deaths in the United States each year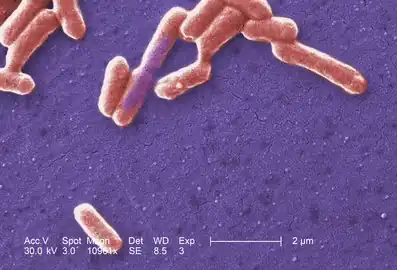 Escherichia coli O157-H7 CDC
Escherichia coli O157-H7 CDC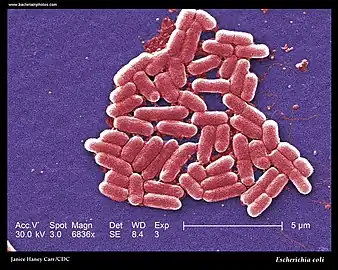 SEM -Escherichia coli (strain O157:H7).
SEM -Escherichia coli (strain O157:H7). E. coli O157:H7
E. coli O157:H7
Escherichia coli is a Gram-negative, facultative anaerobic, rod-shaped, coliform bacterium of the genus Escherichia that is commonly found in the lower intestine of warm-blooded organisms.[8][9] Most E. coli strains are harmless, but some serotypes can cause serious food poisoning in their hosts, and are occasionally responsible for food contamination incidents that prompt product recalls.[10][11]
Like the other strains of the species, O157:H7 is gram-negative and oxidase-negative. Unlike many other strains, it does not ferment sorbitol, which provides a basis for clinical laboratory differentiation of the strain. Strains of E. coli that express Shiga and Shiga-like toxins gained that ability via infection with a prophage containing the structural gene coding for the toxin, and nonproducing strains may become infected and produce shiga-like toxins after incubation with shiga toxin positive strains. The prophage responsible seems to have infected the strain's ancestors fairly recently, as viral particles have been observed to replicate in the host if it is stressed in some way (e.g. antibiotics).[12][13]
All clinical isolates of E. coli O157:H7 possess the plasmid pO157.[14] The periplasmic catalase is encoded on pO157 and may enhance the virulence of the bacterium by providing additional oxidative protection when infecting the host.[15] E. coli O157:H7 non-hemorrhagic strains are converted to hemorrhagic strains by lysogenic conversion after bacteriophage infection of non-hemorrhagic cells.[16][17]
Natural habitat
While it is relatively uncommon, the E. coli serotype O157:H7 can naturally be found in the intestinal contents of some cattle, goats.[18]The digestive tract of cattle lack the Shiga toxin receptor globotriaosylceramide, and thus, these can be asymptomatic carriers of the bacterium.[19] The prevalence of E. coli O157:H7 in North American feedlot cattle herds ranges from 0 to 60%.[20] Some cattle may also be so-called “super-shedders” of the bacterium. Super-shedders may be defined as cattle exhibiting rectoanal junction colonization and excreting >103 to 4 CFU g−1 feces. Super-shedders have been found to constitute a small proportion of the cattle in a feedlot (<10%) but they may account for >90% of all E. coli O157:H7 excreted.[21]
Mechanism
Some strains of E. coli, like O157:H7, can produce Shiga toxin . The Shiga toxin causes inflammatory responses in target cells of the gut, leaving behind lesions which result in the bloody diarrhea that is a symptom of a Shiga toxin-producing E. coli infection. This toxin further causes premature destruction of the red blood cells, which then clog the body's filtering system, the kidneys, in some rare cases causing hemolytic-uremic syndrome , which may lead to kidney failure and even death. In addition, this strain causes the buildup of fluid, leading to edema around the lungs, legs, and arms. This increase in fluid buildup especially around the lungs impedes the functioning of the heart, causing an increase in blood pressure.[22][23]
Transmission
Infection with E. coli O157:H7 can come from ingestion of contaminated food or water, or oral contact with contaminated surfaces. Examples of this can be undercooked ground beef but also leafy vegetables and raw milk. Fields often get contaminated with the bacterium through irrigation processes or contaminated water naturally entering the soil.[24] It is highly virulent, with a low infectious dose: an inoculation of fewer than 10 to 100 CFU of E. coli O157:H7 is sufficient to cause infection, compared to over one-million CFU for other pathogenic E. coli strains.[25]
Diagnosis

A stool culture can detect the bacterium, although it is not a routine test and so must be specifically requested. The sample is cultured on sorbitol-MacConkey (SMAC) agar, or the variant cefixime potassium tellurite sorbitol-MacConkey agar (CT-SMAC)[26]
On SMAC agar, O157:H7 colonies appear clear due to their inability to ferment sorbitol, while the colonies of the usual sorbitol-fermenting serotypes of E. coli appear red. Sorbitol nonfermenting colonies are tested for the somatic O157 antigen before being confirmed as E. coli O157:H7.[27]
Like all cultures, diagnosis is time-consuming with this method; swifter diagnosis is possible using quick E. coli DNA extraction method[27] plus PCR techniques.
Prevention
Proper hand washing after using the lavatory or changing a diaper, especially among children or those with diarrhea, reduces the risk of transmission. Anyone with a diarrheal illness should avoid swimming in public pools or lakes, sharing baths with others, and preparing food for others and even avoiding raw milk.[28]
Surveillance
E. coli O157:H7 infection is a nationally reportable disease in the US, Great Britain, and Germany. It is also reportable in most states of Australia including Queensland.[29]
Treatment
While fluid replacement and blood pressure support may be necessary to prevent death from dehydration, most patients recover without treatment in 5–10 days. There is no evidence that antibiotics improve the course of disease, and treatment with antibiotics may precipitate hemolytic uremic syndrome.[30]
The antibiotics are thought to trigger prophage induction, and the prophages released by the dying bacteria infect other susceptible bacteria, converting them into toxin-producing forms. Antidiarrheal agents, such as loperamide , should also be avoided as they may prolong the duration of the infection.[31][3]
Certain novel treatment strategies, such as the use of anti-induction strategies to prevent toxin production[32] and the use of anti-Shiga toxin antibodies,[33] have also been proposed.
Epidemiology
The pathogen results in an estimated 2,100 hospitalizations annually in the United States. The illness is often misdiagnosed; therefore, expensive and invasive diagnostic procedures may be performed. Patients who develop HUS often require prolonged hospitalization, dialysis, and long-term followup.[34]
Outbreaks
United States and Canada

- The 1993 Jack in the Box E. coli outbreak occurred when the Escherichia coli O157:H7 bacterium (originating from contaminated beef patties) killed four children and infected 732 people across four states.[35][36][37] The outbreak involved 73 Jack in the Box restaurants in California, Idaho, Washington, and Nevada, and has been described as "far and away the most infamous food poison outbreak in contemporary history."[38][39]
- The U.S.D.A. banned the sale of ground beef contaminated with the O157:H7 strain in 1994.[40]
- The 1996 Odwalla E. coli outbreak began on October 7, 1996, when American food company Odwalla produced a batch of unpasteurized apple juice using blemished fruit contaminated with the E. coli bacterium, which ultimately killed a 16-month-old girl and sickened 70 people in California, Colorado, Washington state, and British Columbia, of whom 25 were hospitalized and 14 developed the hemolytic uremic syndrome.[41]On October 30, 1996, health officials from the state of Washington informed Odwalla that they had found a link between an outbreak of the Escherichia coli O157:H7 bacterium and a batch of Odwalla's fresh apple juice produced on October 7. This was confirmed on November 5, and may have resulted from using rotten fruit; one account tells of fruit being used that was highly decayed.[42]
- The Walkerton E. coli outbreak was the result of a contamination of the drinking water supply of Walkerton, Ontario, Canada, with E. coli O157:H7 and Campylobacter jejuni bacteria. The water supply was contaminated as a result of improper water treatment following heavy rainfall in late April and early May 2000, that had drawn bacteria from the manure of nearby cattle used to fertilize crops into the shallow aquifer of a nearby well. The first reported case was on May 17. The contamination caused gastroenteritis and sickened more than 2,000 people and resulted in six deaths.[43][44]
.jpg.webp)
- Six states in the U.S. between July 26, 2022, and August 17, 2022, had 109 individuals with infection from the E. coli O157:H7 strain, after eating at Wendy's restaurant. [45][46]
- The outbreak was officially over, according to the CDC on October 4, 2022.[46]
See also
References
- ↑ Gally DL, Stevens MP (January 2017). "Microbe Profile: Escherichia coli O157:H7 - notorious relative of the microbiologist's workhorse" (PDF). Microbiology. 163 (1): 1–3. doi:10.1099/mic.0.000387. PMID 28218576. Archived (PDF) from the original on 2020-10-31. Retrieved 2022-10-10.
- ↑ Karch H, Tarr PI, Bielaszewska M (October 2005). "Enterohaemorrhagic Escherichia coli in human medicine". International Journal of Medical Microbiology. 295 (6–7): 405–18. doi:10.1016/j.ijmm.2005.06.009. PMID 16238016.
- 1 2 3 Ameer, Muhammad Atif; Wasey, Abdul; Salen, Philip (2022). "Escherichia Coli (E Coli 0157 H7)". StatPearls. StatPearls Publishing. Archived from the original on 11 October 2022. Retrieved 20 October 2022.
- ↑ "Reports of Selected E. coli Outbreak Investigations". CDC.gov. 2019-11-22. Archived from the original on 2022-09-24. Retrieved 2022-10-10.
- ↑ Ciccarelli S, Stolfi I, Caramia G (October 2013). "Management strategies in the treatment of neonatal and pediatric gastroenteritis". Infection and Drug Resistance. 6: 133–61. doi:10.2147/IDR.S12718. PMC 3815002. PMID 24194646.
- ↑ Roos V, Ulett GC, Schembri MA, Klemm P (January 2006). "The asymptomatic bacteriuria Escherichia coli strain 83972 outcompetes uropathogenic E. coli strains in human urine". Infection and Immunity. 74 (1): 615–24. doi:10.1128/IAI.74.1.615-624.2006. PMC 1346649. PMID 16369018.
- ↑ Rodrigo, Luis (30 September 2020). E. Coli Infections: Importance of Early Diagnosis and Efficient Treatment. BoD – Books on Demand. p. 3. ISBN 978-1-83962-523-7. Archived from the original on 25 October 2022. Retrieved 25 October 2022.
- ↑ Tenaillon O, Skurnik D, Picard B, Denamur E (March 2010). "The population genetics of commensal Escherichia coli". Nature Reviews. Microbiology. 8 (3): 207–17. doi:10.1038/nrmicro2298. PMID 20157339. S2CID 5490303.
- ↑ Singleton P (1999). Bacteria in Biology, Biotechnology and Medicine (5th ed.). Wiley. pp. 444–54. ISBN 978-0-471-98880-9.
- ↑ "Escherichia coli". CDC National Center for Emerging and Zoonotic Infectious Diseases. Archived from the original on 25 September 2012. Retrieved 2 October 2012.
- ↑ Vogt RL, Dippold L (2005). "Escherichia coli O157:H7 outbreak associated with consumption of ground beef, June–July 2002". Public Health Reports. 120 (2): 174–78. doi:10.1177/003335490512000211. PMC 1497708. PMID 15842119.
- ↑ O'Brien AD, Newland JW, Miller SF, Holmes RK, Smith HW, Formal SB (November 1984). "Shiga-like toxin-converting phages from Escherichia coli strains that cause hemorrhagic colitis or infantile diarrhea". Science. 226 (4675): 694–96. Bibcode:1984Sci...226..694O. doi:10.1126/science.6387911. PMID 6387911.
- ↑ Strockbine NA, Marques LR, Newland JW, Smith HW, Holmes RK, O'Brien AD (July 1986). "Two toxin-converting phages from Escherichia coli O157:H7 strain 933 encode antigenically distinct toxins with similar biologic activities". Infection and Immunity. 53 (1): 135–40. doi:10.1128/IAI.53.1.135-140.1986. PMC 260087. PMID 3522426.
- ↑ Lim JY, Yoon J, Hovde CJ (January 2010). "A brief overview of Escherichia coli O157:H7 and its plasmid O157". Journal of Microbiology and Biotechnology. 20 (1): 5–14. doi:10.4014/jmb.0908.08007. PMC 3645889. PMID 20134227.
- ↑ Brunder W, Schmidt H, Karch H (November 1996). "KatP, a novel catalase-peroxidase encoded by the large plasmid of enterohaemorrhagic Escherichia coli O157:H7". Microbiology. 142 ( Pt 11) (11): 3305–15. doi:10.1099/13500872-142-11-3305. PMID 8969527.
- ↑ Kushwaha, Dr A. K. (26 July 2020). Textbook of Microbiology. Dr. A.K KUSHWAHA. p. 171. Archived from the original on 24 October 2022. Retrieved 24 October 2022.
- ↑ Liu, Dongyou (8 April 2014). Manual of Security Sensitive Microbes and Toxins. CRC Press. p. 520. ISBN 978-1-4665-5398-9. Archived from the original on 24 October 2022. Retrieved 24 October 2022.
- ↑ Lim, Ji Youn; Yoon, Jang W.; Hovde, Carolyn J. (2010). "A Brief Overview of Escherichia coli O157:H7 and Its Plasmid O157". Journal of microbiology and biotechnology. 20 (1): 5–14. ISSN 1017-7825. Archived from the original on 23 October 2022. Retrieved 23 October 2022.
- ↑ Pruimboom-Brees IM, Morgan TW, Ackermann MR, Nystrom ED, Samuel JE, Cornick NA, Moon HW (September 2000). "Cattle lack vascular receptors for Escherichia coli O157:H7 Shiga toxins". Proceedings of the National Academy of Sciences of the United States of America. 97 (19): 10325–29. Bibcode:2000PNAS...9710325P. doi:10.1073/pnas.190329997. PMC 27023. PMID 10973498.
- ↑ Jeon SJ, Elzo M, DiLorenzo N, Lamb GC, Jeong KC (2013). "Evaluation of animal genetic and physiological factors that affect the prevalence of Escherichia coli O157 in cattle". PLOS ONE. 8 (2): e55728. Bibcode:2013PLoSO...855728J. doi:10.1371/journal.pone.0055728. PMC 3566006. PMID 23405204.
- ↑ Chase-Topping M, Gally D, Low C, Matthews L, Woolhouse M (December 2008). "Super-shedding and the link between human infection and livestock carriage of Escherichia coli O157". Nature Reviews. Microbiology. 6 (12): 904–12. doi:10.1038/nrmicro2029. PMC 5844465. PMID 19008890.
- ↑ "Hemolytic uremic syndrome (HUS)". Mayo Clinic. Archived from the original on 2014-01-02. Retrieved 2022-10-26.
- ↑ "CDC Features - E. coli Infection and Food Safety". web.archive.org. 1 February 2014. Archived from the original on 1 February 2014. Retrieved 26 October 2022.
{{cite web}}: CS1 maint: bot: original URL status unknown (link) - ↑ Scutti, Susan. "Why deadly E. coli loves leafy greens". CNN. Archived from the original on 2018-05-13. Retrieved 2018-09-20.
- ↑ J.D. Greig, E.C.D. Todd, C. Bartleson, and B. Michaels. March 25, 2010. "Infective Doses and Pathen Carriage Archived 2010-10-16 at the Wayback Machine", pp. 19–20, USDA 2010 Food Safety Education Conference.
- ↑ "MACCONKEY SORBITOL AGAR (CT-SMAC)" (PDF). Archived from the original (PDF) on 2011-07-16. Retrieved 2010-12-11.
- 1 2 "Quick E. coli DNA extraction filter paper card". Archived from the original on 2014-07-17. Retrieved 2014-07-11.
- ↑ "Viruses, Bacteria, and Parasites in the Digestive Tract - Health Encyclopedia - University of Rochester Medical Center". www.urmc.rochester.edu. Archived from the original on 2022-10-19. Retrieved 2020-01-17.
- ↑ "Journal". Archived from the original on 2020-09-08. Retrieved 2022-10-10.
- ↑ Walterspiel JN, Ashkenazi S, Morrow AL, Cleary TG (1992). "Effect of subinhibitory concentrations of antibiotics on extracellular Shiga-like toxin I". Infection. 20 (1): 25–29. doi:10.1007/BF01704889. PMID 1563808. S2CID 39513818.
- ↑ "Investigation of Outbreak of Human Infections Caused by E. coli O157:H7 | E. coli CDC". www.cdc.gov. Archived from the original on 17 October 2021. Retrieved 21 October 2022.
- ↑ Keen EC (December 2012). "Paradigms of pathogenesis: targeting the mobile genetic elements of disease". Frontiers in Cellular and Infection Microbiology. 2: 161. doi:10.3389/fcimb.2012.00161. PMC 3522046. PMID 23248780.
- ↑ Tzipori S, Sheoran A, Akiyoshi D, Donohue-Rolfe A, Trachtman H (October 2004). "Antibody therapy in the management of shiga toxin-induced hemolytic uremic syndrome". Clinical Microbiology Reviews. 17 (4): 926–41, table of contents. doi:10.1128/CMR.17.4.926-941.2004. PMC 523565. PMID 15489355.
- ↑ Berkenpas, E.; Millard, P.; Pereira da Cunha, M. (2005-12-13). "Detection of Escherichia coli O157:H7 with langasite pure shear horizontal surface acoustic wave sensors". Biosensors and Bioelectronics. 21 (12): 2255–2262. doi:10.1016/j.bios.2005.11.005. PMID 16356708.
- ↑ Schlosser 2001, p. 198.
- ↑ Nestle 2010, p. 73.
- ↑ "Other big E.coli outbreaks". South Wales Echo. Cardiff. March 11, 2008. p. 9. ProQuest document ID 342321106.
- ↑ Denn, Rebekah (May 13, 2011). "Poisoned author Jeff Benedict examines the current state of food safety in the US". The Christian Science Monitor. Boston, MA. Archived from the original on October 20, 2022. Retrieved July 8, 2013.
- ↑ Golan et al. 2004, p. 10.
- ↑ "Ban on E. Coli in Ground Beef Is to Extend to 6 More Strains". The New York Times. September 12, 2011. Archived from the original on 2013-04-26. Retrieved 2011-10-08.
After the U.S.D.A. banned the O157 form of E. coli from ground beef in 1994, the meat industry sued to block the move, but the agency prevailed in court.
- ↑ Cody SH, Glynn MK, Farrar JA, Cairns KL, Griffin PM, Kobayashi J, Fyfe M, Hoffman R, King AS, Lewis JH, Swaminathan B, Bryant RG, Vugia DJ (February 2, 1999). "An outbreak of Escherichia coli O157:H7 infection from unpasteurized commercial apple juice". Ann Intern Med. 130 (3): 202-9. PMID 10049198. Archived from the original on 5 March 2022. Retrieved 8 March 2022.
- ↑ Drew, Christopher; Belluck, Pam (January 4, 1998). "Deadly Bacteria a New Threat To Fruit and Produce in U.S." The New York Times. New York. Archived from the original on December 25, 2015. Retrieved April 13, 2015.
- ↑ Ali, S. Harris (June 2004). "A socio-ecological autopsy of the E. coli O157:H7 outbreak in Walkerton, Ontario, Canada". Social Science & Medicine (1982). 58 (12): 2601–2612. doi:10.1016/j.socscimed.2003.09.013. ISSN 0277-9536. Archived from the original on 31 August 2021. Retrieved 20 October 2022.
- ↑ Salvadori, Marina I.; Sontrop, Jessica M.; Garg, Amit X.; Moist, Louise M.; Suri, Rita S.; Clark, William F. (February 2009). "Factors that led to the Walkerton tragedy". Kidney International. Supplement (112): S33–34. doi:10.1038/ki.2008.616. ISSN 0098-6577. Archived from the original on 13 April 2022. Retrieved 20 October 2022.
- ↑ "The E. Coli Outbreak Linked To Wendy's Has Officially Ended". MSN. Archived from the original on 20 October 2022. Retrieved 20 October 2022.
- 1 2 "Investigation Details | E. coli Outbreak with Unknown Food Source | CDC". www.cdc.gov. 4 October 2022. Archived from the original on 19 October 2022. Retrieved 20 October 2022.
External links
| Classification |
|---|
- E. coli: Protecting yourself and your family from a sometimes deadly bacterium
- Escherichia coli O157:H7 genomes and related information at PATRIC, a Bioinformatics Resource Center funded by NIAID Archived 2021-08-26 at the Wayback Machine
- For more information about reducing your risk of foodborne illness, visit the US Department of Agriculture's Food Safety and Inspection Service Archived 2002-04-16 at the Wayback Machine website or the [Archived 2022-10-08 at the Wayback Machine The Partnership for Food Safety Education | Fight BAC! Partnership for Food Safety Education
- Cooking Ground Beef Safely Archived 2022-10-08 at the Wayback Machine