Caudal anaesthesia
| Caudal anaesthesia | |
|---|---|
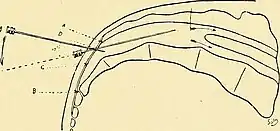 Canal block showing needle puncture over sacral area with the patient in the lateral position |
Caudal anaesthesia (or caudal anesthesia) is a form of neuraxial regional anaesthesia conducted by accessing the epidural space via the sacral hiatus. It is typically used in paediatrics to provide peri- and post-operative analgesia for surgeries below the umbilicus. In adults it is used for chronic low back pain management.[1]
It can be used as an alternative to general anaesthesia or as adjunct to it.[2]
Indications
Caudal anaesthesia is a relatively low-risk technique[3] commonly used, either on its own or in combination with sedation or general anaesthesia.[2][4]
Caudal anesthesia may be favored for sub-umbilical region surgeries in the pediatric population, such as inguinal hernia repair, circumcision, hypospadias repair, anal atresia, or to immobilise newborns with hip dysplasia. Success rate is limited when used for mid-abdominal interventions such as umbilical hernia repair. This is due to the unpredictable cephalad spread of the local anesthetics.[5]
It may also be used in patients with lumbar spinal stenosis, lumbar spinal radiculopathy, postlaminectomy pain, or nonspecific chronic low back pain that fail conservative treatment.[6][7]
List of indications:[5]
- Obstetrics and general surgery below the umbilicus
- Acute and chronic pain refractory to conservative management
- Patients with previous lumbar spine surgery
- Patients who are "anticoagulated" or have coagulopathy
Contraindications
Contraindications to caudal anesthesia include patient or guardian refusal, localized infection over the sacral area, severe coagulopathy and elevated intracranial pressure. It should also be avoided in case of allergies to local anesthetics to be used for the procedure.[4]
Risks and complications
Serious complications are infrequent. When they occur, they are similar those encountered with lumbar epidural block. Some of the risks associated with caudal anesthesia include:
- Needle misplacement leading to subdural, intravascular, intraosseous or antesacral injection with rectum perforation
- Infection, such as epidural abscess, meningitis or sacral osteomyelitis
- Low blood pressure
- Injury to the nerve roots
- Epidural hematoma
- Local anesthetic toxicity, more frequently following caudal anesthesia than it does following lumbar or thoracic blocks.[5]
The most common complications of the anatomic technique for caudal block include: needle misplacement, subarachnoid puncture, and intrathecal or intravascular injections.[1]
Technique
A caudal block may be performed by using anatomic landmarks to guide needle insertion. However, greatest accuracy is obtained by performing caudal blocks using imaging guidance, such as ultrasound or fluoroscopy.[4] Common local anesthetic drugs for caudal blockade are bupivacaine and ropivacaine. Opioids, ketamine or opioids are common drug added as they prolong the postoperative analgesia while minimizing the motor block.[8]
History
Caudal anesthesia was first described independently in 1901 by Fernand Cathelin and Jean-Athanase Sicard. It predates the lumbar epidural approach which was described by Fidel Pagés Miravé in 1921. However, the high failure rate found in caudal anesthesia (5–10%) limited its popularity until the 1940s when it resurfaced in obstetrics anaesthesia.[9][5] The first publication to describe caudal anaesthesia in children was published by Meredith Campbell in 1933.[10]
See also
References
- 1 2 Dernek B, Aydoğmuş S, Ulusoy İ, Duymuş TM, Ersoy S, Kesiktaş FN, et al. (2022). "Caudal epidural steroid injection for chronic low back pain: A prospective analysis of 107 patients". Journal of Back and Musculoskeletal Rehabilitation. 35 (1): 135–139. doi:10.3233/BMR-200262. PMID 34151825. S2CID 235492058.
- 1 2 Wiegele M, Marhofer P, Lönnqvist PA (April 2019). "Caudal epidural blocks in paediatric patients: a review and practical considerations". British Journal of Anaesthesia. 122 (4): 509–517. doi:10.1016/j.bja.2018.11.030. PMC 6435837. PMID 30857607.
- ↑ Ivani G, Suresh S, Ecoffey C, Bosenberg A, Lonnqvist PA, Krane E, et al. (2015). "The European Society of Regional Anaesthesia and Pain Therapy and the American Society of Regional Anesthesia and Pain Medicine Joint Committee Practice Advisory on Controversial Topics in Pediatric Regional Anesthesia". Regional Anesthesia and Pain Medicine. 40 (5): 526–532. doi:10.1097/AAP.0000000000000280. PMID 26192549. S2CID 205430620.
- 1 2 3 Sanghvi C, Dua A (September 2022). "Caudal Anesthesia.". StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. PMID 31869157.
- 1 2 3 4 Candido KD, Winnie AP (2007). "Chapter 15. caudal anesthesia.". In Hadzic A (ed.). NYSORA Textbook of Regional Anesthesia and Acute Pain Management. McGraw Hill. ISBN 978-0-07-144906-9.
- ↑ Kao SC, Lin CS (2017). "Caudal Epidural Block: An Updated Review of Anatomy and Techniques". BioMed Research International. 2017: 9217145. doi:10.1155/2017/9217145. PMC 5346404. PMID 28337460.
- ↑ Lin Z, Fang Y, Yan L, Lin Y, Liu M, Zhang B, et al. (August 2021). "General versus general anaesthesia combined with caudal block in laparoscopic-assisted Soave pull-through of Hirschsprung disease: a retrospective study". BMC Anesthesiology. 21 (1): 209. doi:10.1186/s12871-021-01431-5. PMC 8404309. PMID 34461833.
- ↑ Disma N, Frawley G, Mameli L, Pistorio A, Alberighi OD, Montobbio G, Tuo P (February 2011). "Effect of epidural clonidine on minimum local anesthetic concentration (ED50) of levobupivacaine for caudal block in children". Pediatric Anesthesia. 21 (2): 128–135. doi:10.1111/j.1460-9592.2010.03478.x. PMID 21159021. S2CID 25897059.
- ↑ Waurick K, Waurick R (July 2015). "[History and Technique of Epidural Anaesthesia]" [History and Technique of Epidural Anaesthesia]. Anasthesiologie, Intensivmedizin, Notfallmedizin, Schmerztherapie (in German). 50 (7–8): 476–82, quiz 483. doi:10.1055/s-0041-100845. PMID 26230893.
- ↑ Pandya C, Mehta K, Patel K, Panchasara K (2014). "Pediatric regional anesthesia- A comparison between pediatric spinal and caudal anesthesia". NHL Journal of Medical Sciences. 3 (1): 72–76.