Chest tube
| Chest tube | |
|---|---|
| Other names: Intercostal drain, chest drain, thoracic catheter, tube thoracostomy, intercostal catheter, Bülau drain | |
 | |
| The free end of the chest tube is usually attached to an underwater seal, below the level of the chest. This allows the air or fluid to escape, but prevents anything returning to the chest. | |
| Specialty | Emergency medicine, general surgery |
| Indications | Pneumothorax, pleural effusion[1] |
| Steps | 1) Place person on back with hand behind their head[2] 2) Clean and inject local anesthetic into the area[2] 3) Make a 2 cm incision at the 5th intercostal space anterior axillary line[2] 4) Use Kelly forceps to dissect one intercostal space up and into the pleural cavity[2] 5) Replace the forceps with a finger to guide in the chest tube[2] 6) Suture, apply gauze, and tape the tube in place[2] 7) Attach the tube to the drainage system[2] |
| Success | Confirmed by chest X-ray, bubbles in drainage system[2] |
| Complications | Subcutaneous emphysema, blockage of the tube, bleeding, infection, reexpansion pulmonary edema, lung or diaphragm injury[1] |
A chest tube is a flexible plastic tube that is inserted through the chest wall into the pleural space.[1] It is used to remove air (pneumothorax), fluid (pleural effusion, hemothorax), or pus (empyema).[1] In those with a tension pneumothorax, a needle thoracostomy may be carried out first.[1]
The person is generally placed on their back, possibly with the head of the bed raised, and their hand behind their head.[2] After the area is cleaned with chlorhexidine and injected with local anesthetic, a 2 cm horizontal incision is make at the 4th or 5th intercostal space anterior axillary line.[2] Kelly forceps are than used to dissect one intercostal space up and into the pleura.[2] A finger may be placed in the hole to help guide in the chest tube.[2] The tube is aimed superiorly for air and inferiorly for fluid.[2] The tube is than sutured, gauze applied, and taped.[2] It is than connected to a drainage system.[2]
In a pneumothorax bubbles will be seen in the drainage system.[2] A chest X-ray is than carried out to confirm placement.[2] Antibiotics are often given to prevent infection.[3] The tube may be removed once air leakage has stopped for more than 12 to 24 hours or the amount of fluid out is under 200 ml per 24 hours.[2] Removal should occur when the person has taken and is holding a maximal breath.[2] Another chest X-rays is done after 12 to 24 hours.[2] Complications may include subcutaneous emphysema, blockage of the tube, bleeding, infection, reexpansion pulmonary edema, and lung or diaphragm injury.[1]
A chest tube was first used by Hippocrates around 400 BC to drain an empyema using a metal tube.[4][5] The addition of water seals came about in 1873.[6] Chest tubes became widely used in the 1920s, for post-pneumonic empyema as a result of the 1918 influenza pandemic.[6] Modern tubes sizes vary from 6 to 40 French (Fr) and are made from either silicone or polyvinyl chloride.[6] They generally have a number of holes at one end and a stripe along the side that appears bright on X-rays.[7]
Medical uses
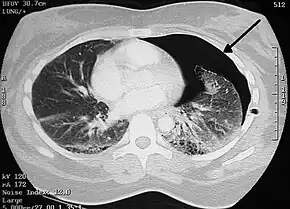
- Pneumothorax: accumulation of air or gas in the pleural space
- Pleural effusion: accumulation of fluid in the pleural space
- Chylothorax: a collection of lymphatic fluid in the pleural space
- Empyema: a pyogenic infection of the pleural space
- Hemothorax: accumulation of blood in the pleural space
- Hydrothorax: accumulation of serous fluid in the pleural space
Tube size
In adults a tube size of 24 to 32 Fr may be used for an open technique.[8][9] Smaller tubes of 8 to 14 Fr may be used for catheter thoracostomy.[8]
Technique
When chest tubes are placed for either blunt or penetrating trauma, antibiotics decrease the risks of infectious complications.[10][3] Typically cephazolin is used as a single dose or for up to 2 days.[3] If more than 1500ml of blood initially comes out in the setting of trauma, or more than 200 cc/hr for 4 hours, a thoracotomy is indicated.[7]
Tube thoracostomy

The free end of the tube is usually attached to an underwater seal, below the level of the chest. This allows the air or fluid to escape from the pleural space, and prevents anything returning to the chest. Alternatively, the tube can be attached to a flutter valve. This allows patients with pneumothorax to remain more mobile.
British Thoracic Society recommends the tube is inserted in an area described as the "safe zone", a region bordered by: the lateral border of pectoralis major, a horizontal line inferior to the axilla, the anterior border of latissimus dorsi and a horizontal line superior to the nipple.[11] More specifically, the tube is inserted into the 5th intercostal space slightly anterior to the mid axillary line.[12]
Chest tubes are usually inserted under local anesthesia. The skin in the area of insertion is first cleansed with antiseptic solution, before sterile drapes are placed around the area. The local anesthetic is injected into the skin and down to the muscle, and after the area is numb a small incision is made in the skin and a passage made through the skin and muscle into the chest. The tube is placed through this passage. If necessary, patients may be given additional analgesics for the procedure. Once the tube is in place it is sutured to the skin to prevent it falling out and a dressing applied to the area. Once the drain is in place, a chest radiograph will be taken to check the location of the drain. The tube stays in for as long as there is air or fluid to be removed, or risk of air gathering.
Chest tubes can also be placed using a trocar, which is a pointed metallic bar used to guide the tube through the chest wall. This method is less popular due to an increased risk of iatrogenic lung injury. Placement using the Seldinger technique, in which a blunt guidewire is passed through a needle (over which the chest tube is then inserted) has been described.
Protocols to maintain chest tube patency by preventing chest tube clogging are necessary.
Postoperative drainage
The placement technique for postoperative drainage (e.g. cardiac surgery) differs from the technique used for emergency situations. At the completion of open cardiac procedures, chest tubes are placed through separate stab incisions, typically near the inferior aspect of the sternotomy incision. In some instances multiple drains may be used to evacuate the mediastinal, pericardial, and pleural spaces. The drainage holes are placed inside the patient and the chest tube is passed out through the incision. Once the tube is in place, it is sutured to the skin to prevent movement. The chest tube is then connected to the drainage canister using additional tubing and connectors and connected to a suction source, typically regulated to -20 cm of water.[13]
Dressings
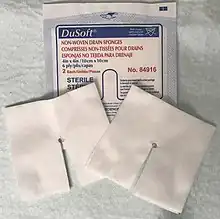
After suturing, dressings are applied to cover the wound. First, a y-slit compress is used around the tube. Second, a compress (10 x 10 cm) is placed on top and finally an adhesive plaster is added in a way that tension is avoided. A bridle rein is recommended to fix the tube to the skin. This tape bridge will prevent the tube from moving backwards and the possibility to cause clogging. It also prevents pain as it reduces tension on the fixation stitch. Alternatively, a large adhesive plaster that functions like a tape bridge may be used.[14]
Tube management
Chest tubes should be kept free of dependent loops, kinks, and obstructions which may prevent drainage.[15] In general, chest tubes are not clamped except during insertion, removal, or when diagnosing air leaks.
Manual manipulation, often called milking, stripping, fan folding, or tapping, of chest tubes is commonly performed to clear chest tube obstructions. No conclusive evidence has demonstrated that any of these techniques are more effective than the others, and no method has shown to improve chest tube drainage.[16] Furthermore, chest tube manipulation has proved to increase negative pressure, which may be detrimental, and painful to the patient.[16] For these reasons, many hospitals do not allow these types of manual tube manipulations.[17]
One option is active chest tube clearance without breaking the sterile field. The 2019 ERAS Guidelines for Perioperative Care recommends active clearance of chest tubes to prevent retained blood and other complications.[18] This was given an IB-NR rating, meaning, it should routinely be performed. Makeshift efforts such as open chest tube clearing that involves breaking the sterile environment separating the chest tube from the drainage canister tubing to suction it out should not be performed (Class III, A).[19]
Complications
Relative contraindications to chest tube placement include a diaphragmatic hernia, as well as hepatic hydrothorax.[20] Additional relative contraindications include scarring in the pleural space (adhesions). It appears that a chest tube can still be safely placed in those with a coagulopathy.[21]
Insertion complications may include hemorrhage, infection, and reexpansion pulmonary edema. While it was previously believed that one should drain no more than 1.5 liters of fluid, the concerns appears unfounded, and draining all fluid present is generally reasonable.[1] Injury to the liver, spleen or diaphragm is possible if the tube is placed inferior to the pleural cavity. Injuries to the thoracic aorta and heart can also occur.[22]
The most common complication of a chest tube is chest tube clogging.[17] Another common complication after thoracic surgery that occurs in 30–50% is air leaks. If a chest tube clogs when there is an airleak the patient will develop a pneumothorax.[23] Here, digital chest drainage systems can provide real time information as they monitor intra-pleural pressure and air leak flow, constantly.[24]
Subcutaneous emphysema indicates backpressure created by undrained air, often caused by a clogged chest tube or insufficient negative pressure.[25] If a patient has subcutaneous emphysema, it is likely their chest tube is not draining and consideration should be given if it should be unclogged or another tube should be placed so that the air leaking from the lung can be adequately drained.
Device
Characteristics

Chest tubes are commonly made from clear plastics like PVC and soft silicone. Chest tubes are made in a range of sizes measured by their external diameter from 6 Fr to 40 Fr. Chest tubes, like most catheters, are measured in French catheter scale. For adults, 20 Fr to 40 Fr (6.7 to 13.3mm external diameter) are commonly used, and 6 Fr to 26 Fr for children. Conventional chest tubes feature multiple drainage fenestrations in the section of the tube which resides inside the patient, as well as distance markers along the length of the tube, and a radiopaque stripe which outlines the first drainage hole.[22] Chest tubes are also provided in right angle, trocar, flared, and tapered configurations for different drainage needs. As well, some chest tubes are coated with heparin to help prevent thrombus formation, though the effect of this is disputed.[27]
Chest tube have an end hole (proximal, toward the patient) and a series of side holes. The number of side holes is generally 6 on most chest tubes. The length of tube that has side holes is the effective drainage length (EDL). In chest tubes designed for pediatric heart surgery, the EDL is shorter, generally by only having 4 side holes.[28]
Channel style chest drains, also called Blake drains, are so-called silastic drains made of silicone and feature open flutes that reside inside the patient. Drainage is thought to be achieved by capillary action, allowing the fluids to travel through the open grooves into a closed cross section, which contains the fluid and allows it to be suctioned through the tube.[13] Though these chest tubes are more expensive than conventional ones, they are theoretically less painful.[29]
Chest drainage system
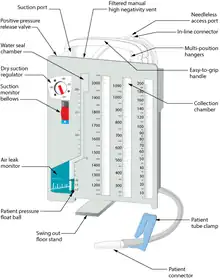

A chest drainage system is typically used to collect chest drainage (air, blood, effusions). Most commonly, drainage systems use three chambers which are based on the three-bottle system. The first chamber allows fluid that is drained from the chest to be collected. The second chamber functions as a "water seal", which acts as a one way valve allowing gas to escape, but not reenter the chest. Air bubbling through the water seal chamber is usual when the patient coughs or exhales but may indicate, if continual, a pleural or system leak that should be evaluated critically. It can also indicate a leak of air from the lung. The third chamber is the suction control chamber. The height of the water in this chamber regulates the negative pressure applied to the system. A gentle bubbling through the water column minimizes evaporation of the fluid and indicates that the suction is being regulated to the height of the water column. In this way, increased wall suction does not increase the negative pressure of the system. Newer drainage systems eliminate the water seal using a mechanical check-valve, and some also use a mechanical regulator to regulate the suction pressure. Systems which employ both these are dubbed "dry" systems, whereas systems that retain the water seal but use a mechanical regulator are called "wet-dry" systems. Systems which use a water seal and water column regulator are called "wet" systems. Dry systems are advantageous as tip-overs of wet systems can spill and mix with blood, mandating the replacement of the system. Even newer systems are smaller and more ambulatory so the patient can be sent home for drainage if indicated.[22]
More recently digital or electronic chest drainage systems have been introduced. An onboard motor is used as vacuum source along with an integrated suction control canister and water seal. These systems monitor the patient and will alert if the measured data are out of range. Due to the digital control of the negative pressure, the system is able to objectively quantify the presence of a pleural or system leak. Digital drainage systems allow clinicians to mobilize patients early, even for those on continuous suction, which is difficult to accomplish with the traditional water-seal system under suction.[23][30] Recently published clinical data indicates, that application of such systems can also lead to a reduction in complications.[31][32]
References
- 1 2 3 4 5 6 7 "How To Do Tube and Catheter Thoracostomy - Pulmonary Disorders". Merck Manuals Professional Edition. Archived from the original on 14 August 2022. Retrieved 9 August 2022.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Dev SP, Nascimiento B, Simone C, Chien V (October 2007). "Videos in clinical medicine. Chest-tube insertion". The New England Journal of Medicine. 357 (15): e15. doi:10.1056/NEJMvcm071974. PMID 17928590. S2CID 73173434.
- 1 2 3 Freeman, JJ; Asfaw, SH; Vatsaas, CJ; Yorkgitis, BK; Haines, KL; Burns, JB; Kim, D; Loomis, EA; Kerwin, AJ; McDonald, A; Agarwal S, Jr; Fox, N; Haut, ER; Crandall, ML; Como, JJ; Kasotakis, G (2022). "Antibiotic prophylaxis for tube thoracostomy placement in trauma: a practice management guideline from the Eastern Association for the Surgery of Trauma". Trauma surgery & acute care open. 7 (1): e000886. doi:10.1136/tsaco-2022-000886. PMID 36312819.
- ↑ M, Sriram Bhat (30 November 2017). SRB's Surgical Operations: Text & Atlas. JP Medical Ltd. p. 203. ISBN 978-93-5270-211-4. Archived from the original on 14 August 2022. Retrieved 10 August 2022.
- ↑ Hippocrates (1847). Genuine Works of Hippocrates. Sydenham Society.
- 1 2 3 Wahidi, Momen M.; Ost, David E. (5 July 2022). Practical Guide to Interventional Pulmonology. Elsevier Health Sciences. p. 165. ISBN 978-0-323-70955-2. Archived from the original on 14 August 2022. Retrieved 10 August 2022.
- 1 2 Ravi, C; McKnight, CL (January 2022). "Chest Tube". PMID 29083704.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 "Chest tube sizing in children and adults". www.uptodate.com. Archived from the original on 8 December 2022. Retrieved 8 December 2022.
- ↑ "ATLS 10th edition offers new insights into managing trauma patients". The Bulletin. 1 June 2018. Archived from the original on 8 December 2022. Retrieved 8 December 2022.
- ↑ Ayoub, F; Quirke, M; Frith, D (2019). "Use of prophylactic antibiotic in preventing complications for blunt and penetrating chest trauma requiring chest drain insertion: a systematic review and meta-analysis". Trauma surgery & acute care open. 4 (1): e000246. doi:10.1136/tsaco-2018-000246. PMID 30899791.
- ↑ Laws D, Neville E, Duffy J (May 2003). "BTS guidelines for the insertion of a chest drain". Thorax. 58 Suppl 2 (90002): ii53-9. doi:10.1136/thorax.58.suppl_2.ii53. PMC 1766017. PMID 12728150.
- ↑ "Ventilatory management". University of Pretoria. Archived from the original on 2009-06-17. Retrieved 2009-09-16.
- 1 2 Obney JA, Barnes MJ, Lisagor PG, Cohen DJ (September 2000). "A method for mediastinal drainage after cardiac procedures using small silastic drains". The Annals of Thoracic Surgery. 70 (3): 1109–10. doi:10.1016/s0003-4975(00)01800-2. PMID 11016389. Archived from the original on 2020-07-27. Retrieved 2019-07-05.
- ↑ Kiefer T (2017). Chest Drains in Daily Clinical Practice. Springer. pp. 102–103. ISBN 9783319323398.
- ↑ Schmelz JO, Johnson D, Norton JM, Andrews M, Gordon PA (September 1999). "Effects of position of chest drainage tube on volume drained and pressure". American Journal of Critical Care. 8 (5): 319–23. doi:10.4037/ajcc1999.8.5.319. PMID 10467469.
- 1 2 Wallen M, Morrison A, Gillies D, O'Riordan E, Bridge C, Stoddart F (October 2004). "Mediastinal chest drain clearance for cardiac surgery". The Cochrane Database of Systematic Reviews (4): CD003042. doi:10.1002/14651858.CD003042.pub2. PMID 15495040.
- 1 2 Shalli S, Saeed D, Fukamachi K, Gillinov AM, Cohn WE, Perrault LP, Boyle EM (2009). "Chest tube selection in cardiac and thoracic surgery: a survey of chest tube-related complications and their management". Journal of Cardiac Surgery. 24 (5): 503–9. doi:10.1111/j.1540-8191.2009.00905.x. PMID 19740284. S2CID 23273268.
- ↑ Engelman DT, Ben Ali W, Williams JB, Perrault LP, Reddy VS, Arora RC, et al. (May 2019). "Guidelines for Perioperative Care in Cardiac Surgery: Enhanced Recovery After Surgery Society Recommendations". JAMA Surgery. 154 (8): 755–766. doi:10.1001/jamasurg.2019.1153. PMID 31054241.
- ↑ Halejian BA, Badach MJ, Trilles F (December 1988). "Maintaining chest tube patency". Surgery, Gynecology & Obstetrics. 167 (6): 521. PMID 3187876.
- ↑ Runyon BA, Greenblatt M, Ming RH (July 1986). "Hepatic hydrothorax is a relative contraindication to chest tube insertion". The American Journal of Gastroenterology. 81 (7): 566–7. PMID 3717119.
- ↑ Fong, C; Chang Tan, CW; Yan Tan, DK; See, KC (24 April 2021). "Safety of Thoracentesis and Tube Thoracostomy in Patients With Uncorrected Coagulopathy: A Systematic Review and Meta-analysis". Chest. doi:10.1016/j.chest.2021.04.036. PMID 33905681.
- 1 2 3 Miller KS, Sahn SA (February 1987). "Chest tubes. Indications, technique, management and complications". Chest. 91 (2): 258–64. doi:10.1378/chest.91.2.258. PMID 3542404.
- 1 2 Brunelli A, Cassivi SD, Salati M, Fibla J, Pompili C, Halgren LA, Wigle DA, Di Nunzio L (April 2011). "Digital measurements of air leak flow and intrapleural pressures in the immediate postoperative period predict risk of prolonged air leak after pulmonary lobectomy". European Journal of Cardio-Thoracic Surgery. 39 (4): 584–8. doi:10.1016/j.ejcts.2010.07.025. PMID 20801054.
- ↑ "Compact Digital Thoracic Drain Systems for the Management of Thoracic Surgical Patients: A Review of the Clinical Effectiveness, Safety, and Cost-Effectiveness". Canadian Agency for Drugs and Technologies in Health. October 1, 2014. Archived from the original on May 13, 2019. Retrieved May 13, 2019.
- ↑ Papiris SA, Roussos C (2004). "Pleural disease in the intensive care unit". In Bouros D (ed.). Pleural Disease (Lung Biology in Health and Disease). Florida: Bendy Jean Baptiste. pp. 771–777. ISBN 978-0-8247-4027-6. Archived from the original on 2021-10-26. Retrieved 2008-05-16.
- ↑ "Chest Tube and Fuhrman Catheter Insertion". University of Bullfalo, The State University of New York. Archived from the original on 2010-04-08. Retrieved 2009-07-19.
- ↑ Kumar P, McKee D, Grant M, Pepper J (April 1997). "Phosphatidylcholine coated chest drains: are they better than conventional drains after open heart surgery?". European Journal of Cardio-Thoracic Surgery. 11 (4): 769–73. doi:10.1016/s1010-7940(96)01145-1. PMID 9151051.
- ↑ "PleuraFlow for Pediatric CT Surgery Clears Chest Tubes of Clots |". 2016-08-02. Archived from the original on 2016-11-04. Retrieved 2016-11-03.
- ↑ Frankel TL, Hill PC, Stamou SC, Lowery RC, Pfister AJ, Jain A, Corso PJ (July 2003). "Silastic drains vs conventional chest tubes after coronary artery bypass". Chest. 124 (1): 108–13. doi:10.1378/chest.124.1.108. PMID 12853511.
- ↑ Bertolaccini L, Rizzardi G, Filice MJ, Terzi A (May 2011). "'Six sigma approach' - an objective strategy in digital assessment of postoperative air leaks: a prospective randomised study". European Journal of Cardio-Thoracic Surgery. 39 (5): e128-32. doi:10.1016/j.ejcts.2010.12.027. PMID 21316980.
- ↑ Leo F, Duranti L, Girelli L, Furia S, Billè A, Garofalo G, et al. (October 2013). "Does external pleural suction reduce prolonged air leak after lung resection? Results from the AirINTrial after 500 randomized cases". The Annals of Thoracic Surgery. 96 (4): 1234–1239. doi:10.1016/j.athoracsur.2013.04.079. PMID 23866802.
- ↑ Miller DL, Helms GA, Mayfield WR (September 2016). "Digital Drainage System Reduces Hospitalization After Video-Assisted Thoracoscopic Surgery Lung Resection". The Annals of Thoracic Surgery. 102 (3): 955–961. doi:10.1016/j.athoracsur.2016.03.089. PMID 27234573.
External links
- Merck Manual Archived 2022-08-14 at the Wayback Machine
- WikEM Archived 2021-07-28 at the Wayback Machine
| Classification |
|---|
