Epidemiology of autism
The epidemiology of autism is the study of the incidence and distribution of autism spectrum disorders (ASD). A 2012 review of global prevalence estimates of autism spectrum disorders found a median of 62 cases per 10,000 people.[1] In contrast, a 2016 review of global prevalence estimates of autism spectrum disorders found a median of 18.5 cases per 10,000 people.[2] However there is a lack of evidence from low- and middle-income countries.[1]
ASD averages a 4.3:1 male-to-female ratio in diagnosis, not accounting for ASD in gender diverse populations, which overlap disproportionately with ASD populations.[3] The number of children known to have autism has increased dramatically since the 1980s, at least partly due to changes in diagnostic practice; it is unclear whether prevalence has actually increased;[4] and as-yet-unidentified environmental risk factors cannot be ruled out.[5] In 2020, the Centers for Disease Control’s Autism and Developmental Disabilities Monitoring (ADDM) Network reported that approximately 1 in 54 children in the United States (1 in 34 boys, and 1 in 144 girls) is diagnosed with an autism spectrum disorder (ASD), based on data collected in 2016.[6] This estimate is a 10% increase from the 1 in 59 rate in 2014, 105% increase from the 1 in 110 rate in 2006 and 176% increase from the 1 in 150 rate in 2000.[6] Diagnostic criteria of ASD has changed significantly since the 1980s; for example, U.S. special-education autism classification was introduced in 1994.[4]
Autism is a complex neurodevelopmental disorder. Many causes have been proposed, but its theory of causation is still questionable and ultimately unknown.[4][7] The possibility of autism is associated with several prenatal factors, including advanced paternal age and diabetes in the mother during pregnancy.[8] ASD is associated with several intellectual or emotional gifts, which has led to a variety of hypotheses from within evolutionary psychiatry that autistic traits have played a beneficial role over human evolutionary history.[9][10] Some individuals perceive it to be connected to genetic disorders[11] and with epilepsy.[12] Autism is believed to be largely inherited, although the genetics of autism are complex, and it is unclear which genes are responsible.[13] Little evidence exists to support associations with specific environmental exposures.[4]
In rare cases, autism is strongly associated with agents that cause birth defects.[14] Other proposed causes, such as childhood vaccines, are controversial. The vaccine hypothesis has been extensively investigated and shown to be false,[15] lacking any scientific evidence.[5] Andrew Wakefield published a small study in 1998 in the United Kingdom suggesting a causal link between autism and the trivalent MMR vaccine. After data included in the report was shown to be deliberately falsified, the paper was retracted, and Wakefield was struck off the medical register in the United Kingdom.[16][17][18]
It is problematic to compare autism rates over the last three decades, as the diagnostic criteria for autism have changed with each revision of the Diagnostic and Statistical Manual (DSM), which outlines which symptoms meet the criteria for an ASD diagnosis. In 1983, the DSM did not recognize PDD-NOS or Asperger’s syndrome, and the criteria for autistic disorder (AD) were more restrictive. The previous edition of the DSM, DSM-IV, included autistic disorder, childhood disintegrative disorder, PDD-NOS, and Asperger’s syndrome. Due to inconsistencies in diagnosis and how much is still being learnt about autism, the most recent DSM (DSM-5) only has one diagnosis, autism spectrum disorder (ASD), which encompasses each of the previous four disorders. According to the new diagnostic criteria for ASD, one must have both struggles in social communication and interaction and restricted repetitive behaviors, interests and activities (RRBs).
ASD diagnoses continue to be over four times more common among boys (1 in 34) than among girls (1 in 154), and they are reported in all racial, ethnic and socioeconomic groups. Studies have been conducted in several continents (Asia, Europe and North America) that report a prevalence rate of approximately 1 to 2 percent.[6] A 2011 study reported a 2.6 percent prevalence of autism in South Korea.[19]
Frequency
Although incidence rates measure autism prevalence directly, most epidemiological studies report other frequency measures, typically point or period prevalence, or sometimes cumulative incidence. Attention is focused mostly on whether prevalence is increasing with time.[4]
Incidence and prevalence
Epidemiology defines several measures of the frequency of occurrence of a disease or condition:[20]
- The incidence rate of a condition is the rate at which new cases occurred per person-year, for example, "2 new cases per 1,000 person-years".
- The cumulative incidence is the proportion of a population that became new cases within a specified time period, for example, "1.5 per 1,000 people became new cases during 2006".
- The point prevalence of a condition is the proportion of a population that had the condition at a single point in time, for example, "10 cases per 1,000 people at the start of 2006".
- The period prevalence is the proportion that had the condition at any time within a stated period, for example, "15 per 1,000 people had cases during 2006".
When studying how conditions are caused, incidence rates are the most appropriate measure of condition frequency as they assess probability directly. However, incidence can be difficult to measure with rarer conditions such as autism.[20] In autism epidemiology, point or period prevalence is more useful than incidence, as the condition starts long before it is diagnosed, bearing in mind genetic elements it is inherent from conception, and the gap between initiation and diagnosis is influenced by many factors unrelated to chance. Research focuses mostly on whether point or period prevalence is increasing with time; cumulative incidence is sometimes used in studies of birth cohorts.[4]
Estimation methods
The three basic approaches used to estimate prevalence differ in cost and in quality of results. The simplest and cheapest method is to count known autism cases from sources such as schools and clinics, and divide by the population. This approach is likely to underestimate prevalence because it does not count children who have not been diagnosed yet, and it is likely to generate skewed statistics because some children have better access to treatment.[21]
The second method improves on the first by having investigators examine student or patient records looking for probable cases, to catch cases that have not been identified yet. The third method, which is arguably the best, screens a large sample of an entire community to identify possible cases, and then evaluates each possible case in more detail with standard diagnostic procedures. This last method typically produces the most reliable, and the highest, prevalence estimates.[21]
Frequency estimates
Estimates of the prevalence of autism vary widely depending on diagnostic criteria, age of children screened, and geographical location.[22] Most recent reviews tend to estimate a prevalence of 1–2 per 1,000 for autism and close to 6 per 1,000 for ASD;[4] PDD-NOS is the vast majority of ASD, Asperger syndrome is about 0.3 per 1,000 and the atypical forms childhood disintegrative disorder and Rett syndrome are much rarer.[23]
A 2006 study of nearly 57,000 British nine- and ten-year-olds reported a prevalence of 3.89 per 1,000 for autism and 11.61 per 1,000 for ASD; these higher figures could be associated with broadening diagnostic criteria.[24] Studies based on more detailed information, such as direct observation rather than examination of medical records, identify higher prevalence; this suggests that published figures may underestimate ASD's true prevalence.[25] A 2009 study of the children in Cambridgeshire, England used different methods to measure prevalence, and estimated that 40% of ASD cases go undiagnosed, with the two least-biased estimates of true prevalence being 11.3 and 15.7 per 1,000.[26]
A 2009 U.S. study based on 2006 data estimated the prevalence of ASD in eight-year-old children to be 9.0 per 1,000 (approximate range 8.6–9.3).[27] A 2009 report based on the 2007 Adult Psychiatric Morbidity Survey by the National Health Service determined that the prevalence of ASD in adults was approximately 1% of the population, with a higher prevalence in males and no significant variation between age groups;[28] these results suggest that prevalence of ASD among adults is similar to that in children and rates of autism are not increasing.[29]
Changes with time
Attention has been focused on whether the prevalence of autism is increasing with time. Earlier prevalence estimates were lower, centering at about 0.5 per 1,000 for autism during the 1960s and 1970s and about 1 per 1,000 in the 1980s, as opposed to today's 18–19 per 1000.[4][6]
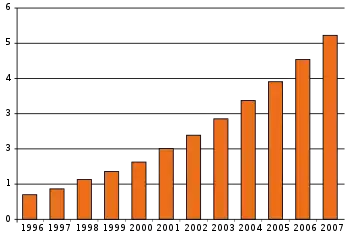
The number of reported cases of autism increased dramatically in the 1990s and early 2000s, prompting investigations into several potential reasons:[31]
- More children may have autism; that is, the true frequency of autism may have increased.
- There may be more complete pickup of autism (case finding), as a result of increased awareness and funding. For example, attempts to sue vaccine companies may have increased case-reporting.
- The diagnosis may be applied more broadly than before, as a result of the changing definition of the disorder, particularly changes in DSM-III-R and DSM-IV.
- An editorial error in the description of the PDD-NOS category of Autism Spectrum Disorders in the DSM-IV, in 1994, inappropriately broadened the PDD-NOS construct. The error was corrected in the DSM-IV-TR, in 2000, reversing the PDD-NOS construct back to the more restrictive diagnostic criteria requirements from the DSM-III-R.[32]
- Successively earlier diagnosis in each succeeding cohort of children, including recognition in nursery (preschool), may have affected apparent prevalence but not incidence.
- A review of the "rising autism" figures compared to other disabilities in schools shows a corresponding drop in findings of mental retardation.[33]
The reported increase is largely attributable to changes in diagnostic practices, referral patterns, availability of services, age at diagnosis, and public awareness.[4][5][30] A widely cited 2002 pilot study concluded that the observed increase in autism in California cannot be explained by changes in diagnostic criteria,[34] but a 2006 analysis found that special education data poorly measured prevalence because so many cases were undiagnosed, and that the 1994–2003 U.S. increase was associated with declines in other diagnostic categories, indicating that diagnostic substitution had occurred.[33]
A 2007 study that modeled autism incidence found that broadened diagnostic criteria, diagnosis at a younger age, and improved efficiency of case ascertainment, can produce an increase in the frequency of autism ranging up to 29-fold depending on the frequency measure, suggesting that methodological factors may explain the observed increases in autism over time.[35] A small 2008 study found that a significant number (40%) of people diagnosed with pragmatic language impairment as children in previous decades would now be given a diagnosis as autism.[36] A study of all Danish children born in 1994–99 found that children born later were more likely to be diagnosed at a younger age, supporting the argument that apparent increases in autism prevalence were at least partly due to decreases in the age of diagnosis.[37]
A 2009 study of California data found that the reported incidence of autism rose 7- to 8-fold from the early 1990s to 2007, and that changes in diagnostic criteria, inclusion of milder cases, and earlier age of diagnosis probably explain only a 4.25-fold increase; the study did not quantify the effects of wider awareness of autism, increased funding, and expanding support options resulting in parents' greater motivation to seek services.[38] Another 2009 California study found that the reported increases are unlikely to be explained by changes in how qualifying condition codes for autism were recorded.[39]
Several environmental factors have been proposed to support the hypothesis that the actual frequency of autism has increased. These include certain foods, infectious disease, pesticides. There is overwhelming scientific evidence against the MMR hypothesis and no convincing evidence for the thiomersal (or Thimerosal) hypothesis, so these types of risk factors have to be ruled out.[5] Although it is unknown whether autism's frequency has increased, any such increase would suggest directing more attention and funding toward addressing environmental factors instead of continuing to focus on genetics.[40]
Geographical frequency
Africa
The prevalence of autism in Africa is unknown.[41]
The Americas
The prevalence of autism in the Americas overall is unknown.
Canada
The rate of autism diagnoses in Canada was 1 in 450 in 2003. However, preliminary results of an epidemiological study conducted at Montreal Children's Hospital in the 200–2004 school year found a prevalence rate of 0.68% (or 1 per 147).[42]
A 2001 review of the medical research conducted by the Public Health Agency of Canada concluded that there was no link between MMR vaccine and either inflammatory bowel disease or autism.[43] The review noted, "An increase in cases of autism was noted by year of birth from 1979 to 1992; however, no incremental increase in cases was observed after the introduction of MMR vaccination."[43] After the introduction of MMR, "A time trend analysis found no correlation between prevalence of MMR vaccination and the incidence of autism in each birth cohort from 1988 to 1993."[43]
United States
CDC's most recent estimate is that 1 out of every 59 children, or 16.8 per 1,000, have some form of ASD as of 2014.[6] The number of diagnosed cases of autism grew dramatically in the U.S. in the 1990s and early 2000s. For the 2006 surveillance year, identified ASD cases were an estimated 9.0 per 1000 children aged 8 years (95% confidence interval [CI] = 8.6–9.3).[27] These numbers measure what is sometimes called "administrative prevalence", that is, the number of known cases per unit of population, as opposed to the true number of cases.[33] This prevalence estimate rose 57% (95% CI 27%–95%) from 2002 to 2006.[27]
The National Health Interview Survey (NHIS) for 2014–2016 studied 30,502 US children and adolescents and found the weighted prevalence of ASD was 2.47% (24.7 per 1,000); 3.63% in boys and 1.25% in girls. Across the 3-year reporting period, the prevalence was 2.24% in 2014, 2.41% in 2015, and 2.76% in 2016.[44]
The number of new cases of autism spectrum disorder (ASD) in Caucasian boys is roughly 50% higher than found in Hispanic children, and approximately 30% more likely to occur than in Non-Hispanic white children in the United States.[4][45]
A further study in 2006 concluded that the apparent rise in administrative prevalence was the result of diagnostic substitution, mostly for findings of mental retardation and learning disabilities.[33] "Many of the children now being counted in the autism category would probably have been counted in the mental retardation or learning disabilities categories if they were being labeled 10 years ago instead of today," said researcher Paul Shattuck of the Waisman Center at the University of Wisconsin–Madison, in a statement.[46]
A population-based study in Olmsted County, Minnesota county found that the cumulative incidence of autism grew eightfold from the 1980–83 period to the 1995–97 period. The increase occurred after the introduction of broader, more-precise diagnostic criteria, increased service availability, and increased awareness of autism.[47] During the same period, the reported number of autism cases grew 22-fold in the same location, suggesting that counts reported by clinics or schools provide misleading estimates of the true incidence of autism.[48]
Venezuela
A 2008 study in Venezuela reported a prevalence of 1.1 per 1,000 for autism and 1.7 per 1,000 for ASD.[49]
Asia
A journal reports that the median prevalence of ASD among 2–6-year-old children who are reported in China from 2000 upwards was 10.3/10,000.[50]
Hong Kong
A 2008 Hong Kong study reported an ASD incidence rate similar to those reported in Australia and North America, and lower than Europeans. It also reported a prevalence of 1.68 per 1,000 for children under 15 years.[51]
Japan
A 2005 study of a part of Yokohama with a stable population of about 300,000 reported a cumulative incidence to age 7 years of 48 cases of ASD per 10,000 children in 1989, and 86 in 1990. After the vaccination rate of the triple MMR vaccine dropped to near zero and was replaced with MR and M vaccine, the incidence rate grew to 97 and 161 cases per 10,000 children born in 1993 and 1994, respectively, indicating that the combined MMR vaccine did not cause autism.[52] A 2004 Japanese autism association reported that about 360.000 people have typical Kanner-type autism.
Middle East
Israel
A 2009 study reported that the annual incidence rate of Israeli children with a diagnosis of ASD receiving disability benefits rose from zero in 1982–1984 to 190 per million in 2004. It was not known whether these figures reflected true increases or other factors such as changes in diagnostic measures.[53]
Saudi Arabia
Studies of autism frequency have been particularly rare in the Middle East. One rough estimate is that the prevalence of autism in Saudi Arabia is 18 per 10,000, slightly higher than the 13 per 10,000 reported in developed countries.[54](compared to 168 per 10,000 in the USA)
Europe
Denmark
In 1992, thiomersal-containing vaccines were removed in Denmark. A study at Aarhus University indicated that during the chemical's usage period (up through 1990), there was no trend toward an increase in the incidence of autism. Between 1991 and 2000 the incidence increased, including among children born after the discontinuation of thimerosal.[55]
France
France made autism the national focus for the year 2012 and the Health Ministry now evaluates the rate of autism to be 67 per 10,000 (1 out of 150).[56]
Eric Fombonne made some studies in the years 1992 and 1997. He found a prevalence of 16 per 10,000 for the global pervasive developmental disorder (PDD).[57][58] The INSERM found a prevalence of 27 per 10,000 for the ASD and a prevalence of 9 per 10,000 for the early infantile autism in 2003.[59] Those figures are considered as underrated as the WHO gives figures between 30 and 60 per 10,000.[60] The French Minister of Health gives a prevalence of 4.9 per 10,000 on its website but it counts only early infantile autism.[61]
Germany
A 2008 study in Germany found that inpatient admission rates for children with ASD increased 30% from 2000 to 2005, with the largest rise between 2000 and 2001 and a decline between 2001 and 2003. Inpatient rates for all mental disorders also rose for ages up to 15 years, so that the ratio of ASD to all admissions rose from 1.3% to 1.4%.[62]
Norway
A 2009 study in Norway reported prevalence rates for ASD ranging from 0.21% to 0.87%, depending on assessment method and assumptions about non-response, suggesting that methodological factors explain large variances in prevalence rates in different studies.[63]
United Kingdom
The incidence and changes in incidence with time are unclear in the United Kingdom.[64] The reported autism incidence in the UK rose starting before the first introduction of the MMR vaccine in 1989.[65] However, a perceived link between the two arising from the results of a fraudulent scientific study has caused considerable controversy, despite being subsequently disproved.[66] A 2004 study found that the reported incidence of pervasive developmental disorders in a general practice research database in England and Wales grew steadily during 1988–2001 from 0.11 to 2.98 per 10,000 person-years, and concluded that much of this increase may be due to changes in diagnostic practice.[67]
Genetics
As late as the mid-1970s there was little evidence of a genetic role in autism; evidence from genetic epidemiology studies now suggests that it is one of the most heritable of all psychiatric conditions.[68] The first studies of twins estimated heritability to be more than 90%; in other words, that genetics explains more than 90% of autism cases.[13] When only one identical twin is autistic, the other often has learning or social disabilities. For adult siblings, the risk of having one or more features of the broader autism phenotype might be as high as 30%,[69] much higher than the risk in controls.[70] About 10–15% of autism cases have an identifiable Mendelian (single-gene) condition, chromosome abnormality, or other genetic syndrome,[69] and ASD is associated with several genetic disorders.[11]
Since heritability is less than 100% and symptoms vary markedly among identical twins with autism, environmental factors are most likely a significant cause as well. If some of the risk is due to gene-environment interaction the 90% heritability estimate may be too high;[4] new twin data and models with structural genetic variation are needed.[71]
Genetic linkage analysis has been inconclusive; many association analyses have had inadequate power.[71] Studies have examined more than 100 candidate genes; many genes must be examined because more than a third of genes are expressed in the brain and there are few clues on which are relevant to autism.[4]
Causing factors
Several studies found a strong association between the use of acetaminophen (e.g., Tylenol, Paracetamol) and autism [72][73] Autism is also associated with several prenatal factors, including advanced age in either parent, diabetes, bleeding and use of psychiatric drugs in the mother during pregnancy.[8] Autism was found to be indirectly linked to prepregnancy obesity and low weight mothers.[74] It is not known whether mutations that arise spontaneously in autism and other neuropsychiatric disorders come mainly from the mother or the father, or whether the mutations are associated with parental age.[75] However, recent studies have identified advancing paternal age as a significant indicator for ASD.[76] Increased chance of autism has also been linked to rapid "catch-up" growth for children born to mothers who had unhealthy weight at conception.[74]
A large 2008 population study of Swedish parents of children with autism found that the parents were more likely to have been hospitalized for a mental disorder, that schizophrenia was more common among the mothers and fathers, and that depression and personality disorders were more common among the mothers.[77]
It is not known how many siblings of autistic individuals are themselves autistic. Several studies based on clinical samples have given quite different estimates, and these clinical samples differ in important ways from samples taken from the general community.[78]
Autism has also been shown to cluster in urban neighborhoods of high socioeconomic status. One study from California found a three to fourfold increased risk of autism in a small 30 by 40 km region centered on West Hollywood, Los Angeles.[79]
Gender differences
Boys have a higher chance of being diagnosed with autism than girls. The ASD sex ratio averages 4.3:1 and is greatly modified by cognitive impairment: it may be close to 2:1 with mental retardation and more than 5.5:1 without. Recent studies have found no association with socioeconomic status, and have reported inconsistent results about associations with race or ethnicity.[4]
RORA deficiency may explain some of the difference in frequency between males and females. RORA protein levels are higher in the brains of typically developing females compared to typically developing males, providing females with a buffer against RORA deficiency. This is known as the Female protective effect. RORA deficiency has previously been proposed as one factor that may make males more vulnerable to autism.[80]
There is a statistically notable overlap between ASD populations and gender diverse populations.[81]
Comorbid conditions
Autism is associated with several other conditions:
- Genetic disorders. About 10–15% of autism cases have an identifiable Mendelian (single-gene) condition, chromosome abnormality, or other genetic syndrome,[69] and ASD is associated with several genetic disorders.[11]
- Intellectual disability. The fraction of autistic individuals who also meet criteria for intellectual disability has been reported as anywhere from 25% to 70%, a wide variation illustrating the difficulty of assessing autistic intelligence.[82]
- Anxiety disorders are common among children with ASD, although there are no firm data.[83] Symptoms include generalized anxiety and separation anxiety,[84] and are likely affected by age, level of cognitive functioning, degree of social impairment, and ASD-specific difficulties. Many anxiety disorders, such as social phobia, are not commonly diagnosed in people with ASD because such symptoms are better explained by ASD itself, and it is often difficult to tell whether symptoms such as compulsive checking are part of ASD or a co-occurring anxiety problem. The prevalence of anxiety disorders in children with ASD has been reported to be anywhere between 11% and 84%.[83]
- Epilepsy, with variations in risk of epilepsy due to age, cognitive level, and type of language disorder; 5–38% of children with autism have comorbid epilepsy, and only 16% of these have remission in adulthood.[12]
- Several metabolic defects, such as phenylketonuria, are associated with autistic symptoms.[85]
- Minor physical anomalies are significantly increased in the autistic population.[86]
- Preempted diagnoses. Although the DSM-IV rules out concurrent diagnosis of many other conditions along with autism, the full criteria for ADHD, Tourette syndrome, and other of these conditions are often present and these comorbid diagnoses are increasingly accepted.[87] A 2008 study found that nearly 70% of children with ASD had at least one psychiatric disorder, including nearly 30% with social anxiety disorder and similar proportions with ADHD and oppositional defiant disorder.[88] Childhood-onset schizophrenia, a rare and severe form, is another preempted diagnosis whose symptoms are often present along with the symptoms of autism.[89]
References
- 1 2 Elsabbagh M, Divan G, Koh YJ, Kim YS, Kauchali S, Marcín C, et al. (June 2012). "Global prevalence of autism and other pervasive developmental disorders". Autism Research. 5 (3): 160–79. doi:10.1002/aur.239. PMC 3763210. PMID 22495912.
- ↑ Maenner M, Shaw K, Baio J, Washington A, Patrick M, DiRienzo M, et al. (June 2016). "Prevalance of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016". Centers for Disease Control and Prevention. 5 (3): 160–79. doi:10.1002/aur.239. PMC 3763210. PMID 22495912.
- ↑ "Largest study to date confirms overlap between autism and gender diversity". Spectrum | Autism Research News. 2020-09-14. Retrieved 2021-08-02.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Newschaffer CJ, Croen LA, Daniels J, Giarelli E, Grether JK, Levy SE, et al. (2007). "The epidemiology of autism spectrum disorders". Annual Review of Public Health. 28: 235–58. doi:10.1146/annurev.publhealth.28.021406.144007. PMID 17367287.
- 1 2 3 4 Rutter M (January 2005). "Incidence of autism spectrum disorders: changes over time and their meaning". Acta Paediatrica. 94 (1): 2–15. doi:10.1111/j.1651-2227.2005.tb01779.x. PMID 15858952. S2CID 79259285.
- 1 2 3 4 5 CDC (2020-03-27). "Data and Statistics on Autism Spectrum Disorder | CDC". Centers for Disease Control and Prevention. Retrieved 2021-06-19.
- ↑ Trottier G, Srivastava L, Walker CD (March 1999). "Etiology of infantile autism: a review of recent advances in genetic and neurobiological research". Journal of Psychiatry & Neuroscience. 24 (2): 103–15. PMC 1188990. PMID 10212552.
- 1 2 Gardener H, Spiegelman D, Buka SL (July 2009). "Prenatal risk factors for autism: comprehensive meta-analysis". The British Journal of Psychiatry. 195 (1): 7–14. doi:10.1192/bjp.bp.108.051672. PMC 3712619. PMID 19567888.
- ↑ Baron-Cohen S (10 November 2020). The pattern seekers : how autism drives human invention. ISBN 978-1-5416-4713-8. OCLC 1204602315.
- ↑ Crespi BJ (2016-06-30). "Autism As a Disorder of High Intelligence". Frontiers in Neuroscience. 10: 300. doi:10.3389/fnins.2016.00300. PMC 4927579. PMID 27445671.
- 1 2 3 Zafeiriou DI, Ververi A, Vargiami E (June 2007). "Childhood autism and associated comorbidities". Brain & Development. 29 (5): 257–72. doi:10.1016/j.braindev.2006.09.003. PMID 17084999. S2CID 16386209.
- 1 2 Levisohn PM (2007). "The autism-epilepsy connection". Epilepsia. 48 Suppl 9 (Suppl 9): 33–5. doi:10.1111/j.1528-1167.2007.01399.x. PMID 18047599. S2CID 25651749.
- 1 2 Freitag CM (January 2007). "The genetics of autistic disorders and its clinical relevance: a review of the literature". Molecular Psychiatry. 12 (1): 2–22. doi:10.1038/sj.mp.4001896. PMID 17033636. S2CID 205678822.
- ↑ Arndt TL, Stodgell CJ, Rodier PM (2005). "The teratology of autism". International Journal of Developmental Neuroscience. 23 (2–3): 189–99. doi:10.1016/j.ijdevneu.2004.11.001. PMID 15749245. S2CID 17797266.
- ↑ Taylor LE, Swerdfeger AL, Eslick GD (June 2014). "Vaccines are not associated with autism: an evidence-based meta-analysis of case-control and cohort studies". Vaccine. 32 (29): 3623–9. doi:10.1016/j.vaccine.2014.04.085. PMID 24814559.
- ↑ Godlee F, Smith J, Marcovitch H (January 2011). "Wakefield's article linking MMR vaccine and autism was fraudulent". BMJ. 342: c7452. doi:10.1136/bmj.c7452. PMID 21209060. S2CID 43640126.
- ↑ Wakefield AJ, Murch SH, Anthony A, Linnell J, Casson DM, Malik M, et al. (February 1998). "Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children". Lancet. 351 (9103): 637–41. doi:10.1016/s0140-6736(97)11096-0. PMID 9500320. S2CID 439791.
- ↑ Boseley S (18 July 2018). "How disgraced anti-vaxxer Andrew Wakefield was embraced by Trump's America". The Guardian.
- ↑ Kim YS, Leventhal BL, Koh YJ, Fombonne E, Laska E, Lim EC, et al. (September 2011). "Prevalence of autism spectrum disorders in a total population sample". The American Journal of Psychiatry. 168 (9): 904–12. doi:10.1176/appi.ajp.2011.10101532. PMID 21558103.
- 1 2 Coggon D, Rose G, Barker DJ (1997). "Quantifying diseases in populations". Epidemiology for the Uninitiated (4th ed.). BMJ. ISBN 0-7279-1102-3.
- 1 2 Scahill L, Bearss K (February 2009). "The rise in autism and the mercury myth". Journal of Child and Adolescent Psychiatric Nursing. 22 (1): 51–3. doi:10.1111/j.1744-6171.2008.00152.x. PMID 19200293.
- ↑ Williams JG, Higgins JP, Brayne CE (January 2006). "Systematic review of prevalence studies of autism spectrum disorders" (PDF). Archives of Disease in Childhood. 91 (1): 8–15. doi:10.1136/adc.2004.062083. PMC 2083083. PMID 15863467. Archived from the original (PDF) on 2009-04-18.
- ↑ Fombonne E (2005). "Epidemiology of autistic disorder and other pervasive developmental disorders". The Journal of Clinical Psychiatry. 66 (Suppl 10): 3–8. PMID 16401144.
- ↑ Baird G, Simonoff E, Pickles A, Chandler S, Loucas T, Meldrum D, Charman T (July 2006). "Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP)". Lancet. 368 (9531): 210–5. doi:10.1016/S0140-6736(06)69041-7. PMID 16844490. S2CID 23532364.
- ↑ Caronna EB, Milunsky JM, Tager-Flusberg H (June 2008). "Autism spectrum disorders: clinical and research frontiers". Archives of Disease in Childhood. 93 (6): 518–23. doi:10.1136/adc.2006.115337. PMID 18305076. S2CID 18761374.
- ↑ Baron-Cohen S, Scott FJ, Allison C, Williams J, Bolton P, Matthews FE, Brayne C (June 2009). "Prevalence of autism-spectrum conditions: UK school-based population study". The British Journal of Psychiatry. 194 (6): 500–9. doi:10.1192/bjp.bp.108.059345. PMID 19478287. S2CID 6928284.
- 1 2 3 "Prevalence of autism spectrum disorders - Autism and Developmental Disabilities Monitoring Network, United States, 2006". Morbidity and Mortality Weekly Report. Surveillance Summaries. 58 (10): 1–20. December 2009. PMID 20023608.
- ↑ Brugha T, McManus S, Meltzer H, et al. (2009). Autism Spectrum Disorders in adults living in households throughout England: Report from the Adult Psychiatric Morbidity Survey 2007 (PDF) (Report). NHS Information Centre for health and social care. Archived from the original (PDF) on 2011-01-03. Retrieved 2010-02-16.
- ↑ Boseley S (2009-09-22). "Autism just as common in adults, so MMR jab is off the hook". Guardian.
- 1 2 Prevalence and changes in diagnostic practice:
- Fombonne E (January 2003). "The prevalence of autism". JAMA. 289 (1): 87–9. doi:10.1001/jama.289.1.87. PMID 12503982.
- Wing L, Potter D (2002). "The epidemiology of autistic spectrum disorders: is the prevalence rising?". Mental Retardation and Developmental Disabilities Research Reviews. 8 (3): 151–61. doi:10.1002/mrdd.10029. PMID 12216059.
- ↑ Wing L, Potter D (1999). "Notes on the prevalence of autism spectrum disorders". National Autistic Society. Retrieved 2007-12-10.
- ↑ "Clarification of the definition of Pervasive Developmental Disorder Not Otherwise Specified".
- 1 2 3 4 Shattuck PT (April 2006). "The contribution of diagnostic substitution to the growing administrative prevalence of autism in US special education". Pediatrics. 117 (4): 1028–37. doi:10.1542/peds.2005-1516. PMID 16585296. S2CID 26733990. Lay summary (2006-04-03).
{{cite journal}}: Cite uses deprecated parameter|lay-url=(help) - ↑ Byrd RS, Sage AC, Keyzer J, et al. (2002). "Report to the legislature on the principal findings of the epidemiology of autism in California: a comprehensive pilot study" (PDF). M.I.N.D. Institute. Archived from the original (PDF) on 2008-04-14.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Wazana A, Bresnahan M, Kline J (June 2007). "The autism epidemic: fact or artifact?". Journal of the American Academy of Child and Adolescent Psychiatry. 46 (6): 721–730. doi:10.1097/chi.0b013e31804a7f3b. PMID 17513984.
- ↑ Bishop DV, Whitehouse AJ, Watt HJ, Line EA (May 2008). "Autism and diagnostic substitution: evidence from a study of adults with a history of developmental language disorder". Developmental Medicine and Child Neurology. 50 (5): 341–5. doi:10.1111/j.1469-8749.2008.02057.x. PMID 18384386. S2CID 22025445.
- ↑ Parner ET, Schendel DE, Thorsen P (December 2008). "Autism prevalence trends over time in Denmark: changes in prevalence and age at diagnosis". Archives of Pediatrics & Adolescent Medicine. 162 (12): 1150–6. doi:10.1001/archpedi.162.12.1150. PMID 19047542.
- ↑ Hertz-Picciotto I, Delwiche L (January 2009). "The rise in autism and the role of age at diagnosis". Epidemiology. 20 (1): 84–90. doi:10.1097/EDE.0b013e3181902d15. PMC 4113600. PMID 19234401. Lay summary – WebMD (2009-01-08).
{{cite journal}}: Cite uses deprecated parameter|lay-url=(help) - ↑ Grether JK, Rosen NJ, Smith KS, Croen LA (October 2009). "Investigation of shifts in autism reporting in the California Department of Developmental Services". Journal of Autism and Developmental Disorders. 39 (10): 1412–9. doi:10.1007/s10803-009-0754-z. PMID 19479197. S2CID 7502270.
- ↑ Szpir M (July 2006). "Tracing the origins of autism: a spectrum of new studies". Environmental Health Perspectives. 114 (7): A412-8. doi:10.1289/ehp.114-a412. PMC 1513312. PMID 16835042. Archived from the original on 2008-07-08.
- ↑ Mankoski RE, Collins M, Ndosi NK, Mgalla EH, Sarwatt VV, Folstein SE (November 2006). "Etiologies of autism in a case-series from Tanzania". Journal of Autism and Developmental Disorders. 36 (8): 1039–51. doi:10.1007/s10803-006-0143-9. PMID 16897390. S2CID 22993074.
- ↑ Childhood Autism in Canada: Some issues relating to behavioural intervention by Sonya Norris, Science and Technology Division; Jean-Rodrigue Paré, Political and Social Affairs Division; Sheena Starky, Economics Division, 2006.
- 1 2 3 Public Health Agency of Canada, Canada Communicable Disease Report, "Does Measles-Mumps-Rubella (MMR) Vaccination cause Inflammatory Bowel Disease and Autism?"
- ↑ Xu G, Strathearn L, Liu B, Bao W (January 2018). "Prevalence of Autism Spectrum Disorder Among US Children and Adolescents, 2014-2016". JAMA. 319 (1): 81–82. doi:10.1001/jama.2017.17812. PMC 5833544. PMID 29297068.
- ↑ "ASD Data and Statistics". CDC.gov. Archived from the original on 2014-04-18. Retrieved 5 Apr 2014.
- ↑ Rise in Autism Rate Misleading, study says CBC news quoting Paul Shattuck, 2006
- ↑ Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ (January 2005). "The incidence of autism in Olmsted County, Minnesota, 1976-1997: results from a population-based study". Archives of Pediatrics & Adolescent Medicine. 159 (1): 37–44. doi:10.1001/archpedi.159.1.37. PMID 15630056.
- ↑ Barbaresi WJ, Colligan RC, Weaver AL, Katusic SK (March 2009). "The incidence of clinically diagnosed versus research-identified autism in Olmsted County, Minnesota, 1976-1997: results from a retrospective, population-based study". Journal of Autism and Developmental Disorders. 39 (3): 464–70. doi:10.1007/s10803-008-0645-8. PMC 2859841. PMID 18791815.
- ↑ Montiel-Nava C, Peña JA (March 2008). "Epidemiological findings of pervasive developmental disorders in a Venezuelan study". Autism. 12 (2): 191–202. doi:10.1177/1362361307086663. PMID 18308767. S2CID 11235638.
- ↑ Sun X, Allison C (April 2010). "A review of the prevalence of Autism Spectrum Disorder in Asia". Research in Autism Spectrum Disorders. 4 (2): 156–167. doi:10.1016/j.rasd.2009.10.003.
- ↑ Wong VC, Hui SL (January 2008). "Epidemiological study of autism spectrum disorder in China". Journal of Child Neurology. 23 (1): 67–72. doi:10.1177/0883073807308702. PMID 18160559. S2CID 29590911.
- ↑ Honda H, Shimizu Y, Rutter M (June 2005). "No effect of MMR withdrawal on the incidence of autism: a total population study". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 46 (6): 572–9. doi:10.1111/j.1469-7610.2005.01425.x. PMID 15877763. Lay summary – Bandolier (2005).
{{cite journal}}: Cite uses deprecated parameter|lay-url=(help) - ↑ Senecky Y, Chodick G, Diamond G, Lobel D, Drachman R, Inbar D (January 2009). "Time trends in reported autistic spectrum disorders in Israel, 1972-2004" (PDF). The Israel Medical Association Journal. 11 (1): 30–3. PMID 19344009. Archived from the original (PDF) on 2011-07-16.
- ↑ Al-Salehi SM, Al-Hifthy EH, Ghaziuddin M (June 2009). "Autism in Saudi Arabia: presentation, clinical correlates and comorbidity". Transcultural Psychiatry. 46 (2): 340–7. doi:10.1177/1363461509105823. PMID 19541755. S2CID 26992006.
- ↑ Madsen KM, Lauritsen MB, Pedersen CB, Thorsen P, Plesner AM, Andersen PH, Mortensen PB (September 2003). "Thimerosal and the occurrence of autism: negative ecological evidence from Danish population-based data". Pediatrics. 112 (3 Pt 1): 604–6. doi:10.1542/peds.112.3.604. PMID 12949291.
- ↑ "Autisme Grande Cause". Archived from the original on 4 April 2012.
- ↑ Fombonne E, du Mazaubrun C (August 1992). "Prevalence of infantile autism in four French regions". Social Psychiatry and Psychiatric Epidemiology. 27 (4): 203–10. doi:10.1007/bf00789007. PMID 1411750. S2CID 20081218.
- ↑ Fombonne E, Du Mazaubrun C, Cans C, Grandjean H (November 1997). "Autism and associated medical disorders in a French epidemiological survey". Journal of the American Academy of Child and Adolescent Psychiatry. 36 (11): 1561–9. doi:10.1016/S0890-8567(09)66566-7. PMID 9394941.
- ↑ Expertise collective. Troubles mentaux. Dépistage et prévention chez l'enfant et chez l'adolescent. Inserm, 2003, 8
- ↑ "Plan autisme 2008–2010: Construire une nouvelle étape de la politique des troubles envahissants du développement (TED) et en particulier de l'autisme" [Autism Plan 2008-2010: Building a new stage in the policy of pervasive developmental disorders (PDD) and in particular autism] (PDF) (in French). Republic of France. Archived from the original (PDF) on 2010-03-27.
- ↑ Jean-François Chossy, La situation des autistes en France, besoins et perspectives, rapport remis au Premier ministre, La Documentation française : Paris, Septembre 2003.
- ↑ Bölte S, Poustka F, Holtmann M (May 2008). "Trends in autism spectrum disorder referrals". Epidemiology. 19 (3): 519–20. doi:10.1097/EDE.0b013e31816a9e13. PMID 18414094.
- ↑ Posserud M, Lundervold AJ, Lie SA, Gillberg C (March 2010). "The prevalence of autism spectrum disorders: impact of diagnostic instrument and non-response bias". Social Psychiatry and Psychiatric Epidemiology. 45 (3): 319–27. doi:10.1007/s00127-009-0087-4. PMID 19551326. S2CID 24751946.
- ↑ "Incidence of autism". National Autistic Society. 2004. Retrieved 2007-12-10.
- ↑ Kaye JA, del Mar Melero-Montes M, Jick H (February 2001). "Mumps, measles, and rubella vaccine and the incidence of autism recorded by general practitioners: a time trend analysis". BMJ. 322 (7284): 460–3. doi:10.1136/bmj.322.7284.460. PMC 26561. PMID 11222420.
- ↑ Deer B (8 February 2009). "MMR doctor Andrew Wakefield fixed data on autism". The Sunday Times. London. Archived from the original on February 27, 2014. Retrieved 2009-02-09.
- ↑ Smeeth L, Cook C, Fombonne PE, Heavey L, Rodrigues LC, Smith PG, Hall AJ (November 2004). "Rate of first recorded diagnosis of autism and other pervasive developmental disorders in United Kingdom general practice, 1988 to 2001". BMC Medicine. 2: 39. doi:10.1186/1741-7015-2-39. PMC 533883. PMID 15535890.
- ↑ Szatmari P, Jones MB (2007). "Genetic epidemiology of autism spectrum disorders". In Volkmar FR (ed.). Autism and Pervasive Developmental Disorders (2nd ed.). Cambridge University Press. pp. 157–178. ISBN 978-0-521-54957-8.
- 1 2 3 Folstein SE, Rosen-Sheidley B (December 2001). "Genetics of autism: complex aetiology for a heterogeneous disorder". Nature Reviews. Genetics. 2 (12): 943–55. doi:10.1038/35103559. PMID 11733747. S2CID 9331084.
- ↑ Bolton P, Macdonald H, Pickles A, Rios P, Goode S, Crowson M, et al. (July 1994). "A case-control family history study of autism". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 35 (5): 877–900. doi:10.1111/j.1469-7610.1994.tb02300.x. PMID 7962246.
- 1 2 Sykes NH, Lamb JA (September 2007). "Autism: the quest for the genes". Expert Reviews in Molecular Medicine. 9 (24): 1–15. doi:10.1017/S1462399407000452. PMID 17764594. S2CID 45880191.
- ↑ Parker W, Hornik CD, Bilbo S, Holzknecht ZE, Gentry L, Rao R, et al. (April 2017). "The role of oxidative stress, inflammation and acetaminophen exposure from birth to early childhood in the induction of autism". The Journal of International Medical Research. 45 (2): 407–438. doi:10.1177/0300060517693423. PMC 5536672. PMID 28415925.
- ↑ Seneff S, Davidson RM, Liu J (7 November 2012). "Empirical Data Confirm Autism Symptoms Related to Aluminum and Acetaminophen Exposure". Entropy. 14 (11): 2227–2253. Bibcode:2012Entrp..14.2227S. doi:10.3390/e14112227.
- 1 2 Moss BG, Chugani DC (2014). "Increased risk of very low birth weight, rapid postnatal growth, and autism in underweight and obese mothers". American Journal of Health Promotion. 28 (3): 181–8. doi:10.4278/ajhp.120705-QUAN-325. PMID 23875984. S2CID 25497329.
- ↑ Schubert C (November 2008). "Male biological clock possibly linked to autism, other disorders". Nature Medicine. 14 (11): 1170. doi:10.1038/nm1108-1170a. PMID 18989289. S2CID 6695070.
- ↑ Geschwind DH (February 2009). "Advances in autism". Annual Review of Medicine. 60 (1): 367–80. doi:10.1146/annurev.med.60.053107.121225. PMC 3645857. PMID 19630577.
- ↑ Daniels JL, Forssen U, Hultman CM, Cnattingius S, Savitz DA, Feychting M, Sparen P (May 2008). "Parental psychiatric disorders associated with autism spectrum disorders in the offspring". Pediatrics. 121 (5): e1357-62. doi:10.1542/peds.2007-2296. PMID 18450879. S2CID 7493945. Lay summary – UNC News (2008-05-05).
{{cite journal}}: Cite uses deprecated parameter|lay-url=(help) - ↑ Rogers SJ (June 2009). "What are infant siblings teaching us about autism in infancy?". Autism Research. 2 (3): 125–37. doi:10.1002/aur.81. PMC 2791538. PMID 19582867.
- ↑ Mazumdar S, King M, Liu KY, Zerubavel N, Bearman P (May 2010). "The spatial structure of autism in California, 1993-2001". Health & Place. 16 (3): 539–46. doi:10.1016/j.healthplace.2009.12.014. PMC 2835822. PMID 20097113.
- ↑ Hu VW, Sarachana T, Sherrard RM, Kocher KM (2015). "Investigation of sex differences in the expression of RORA and its transcriptional targets in the brain as a potential contributor to the sex bias in autism". Molecular Autism. 6: 7. doi:10.1186/2040-2392-6-7. PMC 4459681. PMID 26056561.
- ↑ "Largest study to date confirms overlap between autism and gender diversity". Spectrum | Autism Research News. 2020-09-14. Retrieved 2021-08-02.
- ↑ Dawson M, Mottron L, Gernsbacher MA (2008). "Learning in autism" (PDF). In Byrne JH, Roediger III HL (eds.). Learning and Memory: A Comprehensive Reference. Vol. 2. Academic Press. pp. 759–72. doi:10.1016/B978-012370509-9.00152-2. ISBN 978-0-12-370504-4. Archived from the original (PDF) on 2012-03-03.
- 1 2 White SW, Oswald D, Ollendick T, Scahill L (April 2009). "Anxiety in children and adolescents with autism spectrum disorders". Clinical Psychology Review. 29 (3): 216–29. doi:10.1016/j.cpr.2009.01.003. PMC 2692135. PMID 19223098.
- ↑ MacNeil BM, Lopes VA, Minnes PM (2009). "Anxiety in children and adolescents with Autism Spectrum Disorders". Res Autism Spectr Disord. 3 (1): 1–21. doi:10.1016/j.rasd.2008.06.001.
- ↑ Manzi B, Loizzo AL, Giana G, Curatolo P (March 2008). "Autism and metabolic diseases". Journal of Child Neurology. 23 (3): 307–14. doi:10.1177/0883073807308698. PMID 18079313. S2CID 30809774.
- ↑ Ozgen HM, Hop JW, Hox JJ, Beemer FA, van Engeland H (March 2010). "Minor physical anomalies in autism: a meta-analysis". Molecular Psychiatry. 15 (3): 300–7. doi:10.1038/mp.2008.75. PMID 18626481. S2CID 26087399.
- ↑ Steyaert JG, De la Marche W (October 2008). "What's new in autism?". European Journal of Pediatrics. 167 (10): 1091–101. doi:10.1007/s00431-008-0764-4. PMID 18597114. S2CID 11831418.
- ↑ Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G (August 2008). "Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample". Journal of the American Academy of Child and Adolescent Psychiatry. 47 (8): 921–9. doi:10.1097/CHI.0b013e318179964f. PMID 18645422. S2CID 205551553.
- ↑ Rapoport J, Chavez A, Greenstein D, Addington A, Gogtay N (January 2009). "Autism spectrum disorders and childhood-onset schizophrenia: clinical and biological contributions to a relation revisited". Journal of the American Academy of Child and Adolescent Psychiatry. 48 (1): 10–8. doi:10.1097/CHI.0b013e31818b1c63. PMC 2664646. PMID 19218893.