Hemoptysis
| Hemoptysis | |
|---|---|
| Other names: Haemoptysis, coughing up of blood | |
 | |
| Frequently hemoptysis bronchitis is indicated. Lower left: Inflammation of the bronchus can bring about bloody mucus. | |
| Pronunciation |
|
| Specialty | Pulmonology |
| Complications | Lack of oxygen[1] |
| Causes | Common: Acute bronchitis, pneumonia, tuberculosis, bronchiectasis, asthma, COPD, cancer[2] Less common: Pulmonary embolism, lung abscess, foreign body, heart failure, lupus, Wegener granulomatosis, mitral valve stenosis, blood clotting problems[2] |
| Diagnostic method | Medical imaging (chest X ray, CT scan), bronchoscopy[2] |
| Differential diagnosis | Gastrointestinal bleed, nose bleed, Serratia marcescens infection[2] |
| Treatment | Bleeding lung down, intubating the good lung, angiography for embolization, bronchoscopy, surgery[1] |
| Frequency | 0.1% of patient visits[2] |
Hemoptysis is the coughing up of blood or blood-stained mucus from the lungs or airway.[2] Hemoptysis is considered life threatening if abnormal vitals are present and massive if bleeding is more than 100 mL (3.5 imp fl oz; 3.4 US fl oz) to 600 mL (21 imp fl oz; 20 US fl oz) in 24 hours.[2] Large amounts of bleeding can result in a lack of oxygen.[1]
The most common cause in adults is acute bronchitis, pneumonia, tuberculosis, bronchiectasis, asthma, COPD, and cancer.[2] Less common causes include pulmonary embolism, lung abscess, foreign body, heart failure, lupus, Wegener granulomatosis, mitral valve stenosis, and blood clotting problems.[2] Bleeding that may look like hemoptysis but is not include a gastrointestinal bleed, nose bleed, and Serratia marcescens infection.[2]
Diagnosis generally includes a chest X-ray with a CT scan and bronchoscopy if significant bleeding or other concerns are present.[2] Treatment begins with resuscitation if needed.[2] In large volume bleeding the affected side should be placed down.[1] Other treatments may include intubating just the good lung, angiography for embolization, bronchoscopy, and surgery.[1] Hemoptysis makes up about one in every 1,000 patient visits.[2]
Cause
The most common causes for hemoptysis in adults are chest infections such as bronchitis or pneumonia.[1] In children, hemoptysis is commonly caused by the presence of a foreign body in the airway. Other common causes include lung cancers and tuberculosis. Less common causes include aspergilloma, bronchiectasis, coccidioidomycosis, pulmonary embolism, pneumonic plague, and cystic fibrosis. Rarer causes include hereditary hemorrhagic telangiectasia (HHT or Rendu-Osler-Weber syndrome), Goodpasture's syndrome, and granulomatosis with polyangiitis. A rare cause of hemoptysis in women is endometriosis, which leads to intermittent hemoptysis coinciding with menstrual periods.[3] Hemoptysis may be exacerbated or even caused by overtreatment with anticoagulant drugs such as warfarin.
Blood-laced mucus from the sinus or nose area can sometimes be misidentified as symptomatic of hemoptysis (such secretions can be a sign of nasal or sinus cancer, but also a sinus infection). Extensive non-respiratory injury can also cause one to cough up blood. Cardiac causes like heart failure and mitral stenosis should be ruled out.
Bright-red, foamy blood more often comes from the respiratory tract, whereas dark-red, coffee-colored blood generally comes from the gastrointestinal tract. Sometimes hemoptysis may be rust-colored.
- Lung cancer, including both non-small cell lung carcinoma and small cell lung carcinoma.[4][5]
- Sarcoidosis[6]
- Aspergilloma[7]
- Tuberculosis[8]
- Histoplasmosis[9]
- Pneumonia
- Pulmonary edema
- Foreign body aspiration and aspiration pneumonia
- Goodpasture's syndrome[10]
- Microscopic polyangiitis
- Granulomatosis with polyangiitis[11]
- Eosinophilic granulomatosis with polyangiitis
- Bronchitis[12]
- Bronchiectasis[12]
- Pulmonary embolism[13]
- Anticoagulant use[13]
- Trauma[13]
- Lung abscess[13]
- Mitral stenosis
- Tropical eosinophilia
- Bleeding disorders
- Hughes-Stovin syndrome and other variants of Behçet's disease
- Pulmonary arteriovenous malformations
Diagnosis
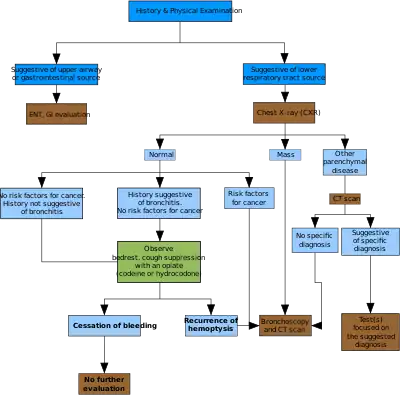
- Past history, history of present illness, family history
- history of tuberculosis, bronchiectasis, chronic bronchitis, mitral stenosis, etc.
- history of cigarette smoking, occupational diseases by exposure to silica dust, etc.
- Blood
- duration, frequency, amount
- Amounts of blood: large amounts of blood, or is there blood-streaked sputum
- Probable source of bleeding: Is the blood coughed up, or vomited?
- Bloody sputum
- color, characters: blood-streaked, fresh blood, frothy pink, bloody gelatinous.
- Accompanying symptoms
- fever, chest pain, coughing, purulent sputum, mucocutaneous bleeding, jaundice.
- Imaging examination
- chest X-ray, CT scan and 3D reconstruction images or CT virtual bronchoscopy, bronchial angiography.
- Laboratory tests
- blood test: WBC
- Sputum: cells and bacterial examinations, sputum culture
- Bronchial fiber endoscopy[14]
Treatment
Treatment depends on the underlying cause. Treatments include iced saline, and topical vasoconstrictors such as adrenalin or vasopressin. Tranexamic acid was proved to improve in-hospital mortality.[15] Selective bronchial intubation can be used to collapse the lung that is bleeding. Also, endobronchial tamponade can be used. Laser photocoagulation can be used to stop bleeding during bronchoscopy. Angiography of bronchial arteries can be performed to locate the bleeding, and it can often be embolized.[16] Bronchial artery embolization (BAE) is the first line treatment nowadays.[17][18][19][20][21] Surgical option is usually the last resort and can involve removal of a lung lobe or removal of the entire lung. Cough suppressants can increase the risk of choking.[1]
References
- 1 2 3 4 5 6 7 Sabatine, Marc S. (2014). Pocket medicine (Fifth ed.). [S.l.]: Aspen Publishers, Inc. p. 2-7. ISBN 978-1451193787.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Earwood, JS; Thompson, TD (15 February 2015). "Hemoptysis: evaluation and management". American family physician. 91 (4): 243–9. PMID 25955625.
- ↑ Rousset P, Rousset-Jablonski C, Alifano M, Mansuet-Lupo A, Buy JN, Revel MP (March 2014). "Thoracic endometriosis syndrome: CT and MRI features". Clinical Radiology. 69 (3): 323–30. doi:10.1016/j.crad.2013.10.014. PMID 24331768.
- ↑ "Google Health – Google". Archived from the original on 2020-05-30. Retrieved 2010-02-05.
- ↑ "Google Health – Google". Archived from the original on 2020-05-30. Retrieved 2010-02-05.
- ↑ "Sarcoidosis Signs & Symptoms – Sarcoidosis – HealthCommunities.com". Archived from the original on 2009-02-21. Retrieved 2010-02-05.
- ↑ MedlinePlus Encyclopedia: Pulmonary aspergilloma
- ↑ "Google Health – Google". Archived from the original on 2020-12-18. Retrieved 2010-02-05.
- ↑ "Histoplasmosis Symptoms – Diseases and Conditions – Mayo Clinic". Archived from the original on 2013-05-31. Retrieved 2010-02-05.
- ↑ Pediatric Goodpasture Syndrome at eMedicine
- ↑ "Granulomatosis with Polyangiitis". www.mayoclinic.org. Mayo Foundation for Medical Education and Research. Archived from the original on 22 December 2017. Retrieved 3 March 2018.
- 1 2 "Hemoptysis Causes – Hemoptysis – HealthCommunities.com". Archived from the original on 2009-01-23. Retrieved 2010-02-05.
- 1 2 3 4 "Other Causes of Hemoptysis – Hemoptysis – HealthCommunities.com". Archived from the original on 2009-06-08. Retrieved 2010-02-05.
- ↑ Richard F.LeBlond (2004). Diagnostics. US: McGraw-Hill Companies, Inc. ISBN 978-0-07-140923-0.
- ↑ Kinoshita, Takahiro; Ohbe, Hiroyuki; Matsui, Hiroki; Fushimi, Kiyohide; Ogura, Hiroshi; Yasunaga, Hideo (December 2019). "Effect of tranexamic acid on mortality in patients with haemoptysis: a nationwide study". Critical Care. 23 (1): 347. doi:10.1186/s13054-019-2620-5. ISSN 1364-8535. PMC 6836388. PMID 31694697.
- ↑ Uppsala Academic Hospital > Guidelines for treatment of acute lung diseases. August 2004. Authors: Christer Hanson, Carl-Axel Karlsson, Mary Kämpe, Kristina Lamberg, Eva Lindberg, Lavinia Machado Boman, Gunnemar Stålenheim
- ↑ Woo S, Yoon CJ, Chung JW, Kang SG, Jae HJ, Kim HC, et al. (November 2013). "Bronchial artery embolization to control hemoptysis: comparison of N-butyl-2-cyanoacrylate and polyvinyl alcohol particles". Radiology. 269 (2): 594–602. doi:10.1148/radiol.13130046. PMID 23801773.
- ↑ Ishikawa H, Hara M, Ryuge M, Takafuji J, Youmoto M, Akira M, et al. (February 2017). "Efficacy and safety of super selective bronchial artery coil embolisation for haemoptysis: a single-centre retrospective observational study". BMJ Open. 7 (2): e014805. doi:10.1136/bmjopen-2016-014805. PMC 5318547. PMID 28213604.
- ↑ Ryuge M, Hara M, Hiroe T, Omachi N, Minomo S, Kitaguchi K, et al. (February 2019). "Mechanisms of recurrent haemoptysis after super-selective bronchial artery coil embolisation: a single-centre retrospective observational study". European Radiology. 29 (2): 707–715. doi:10.1007/s00330-018-5637-2. PMC 6302874. PMID 30054792.
- ↑ Panda, Ananya; Bhalla, Ashu Seith; Goyal, Ankur (2017-07-07). "Bronchial artery embolization in hemoptysis: a systematic review". Diagnostic and Interventional Radiology. 23 (4): 307–317. doi:10.5152/dir.2017.16454. PMC 5508955. PMID 28703105.
- ↑ Olsen, Kathryn M.; Manouchehr-pour, Shawdi; Donnelly, Edwin F.; Henry, Travis S.; Berry, Mark F.; Boiselle, Phillip M.; Colletti, Patrick M.; Harrison, Nicholas E.; Kuzniewski, Christopher T.; Laroia, Archana T.; Maldonado, Fabien (May 2020). "ACR Appropriateness Criteria® Hemoptysis". Journal of the American College of Radiology. 17 (5): S148–S159. doi:10.1016/j.jacr.2020.01.043. PMID 32370959.
External links
| Classification | |
|---|---|
| External resources |
- Corey, Ralph (1990). Hemoptysis. Clinical Methods: The History, Physical, and Laboratory Examinations. Butterworths. ISBN 9780409900774. PMID 21250201. Archived from the original on 4 March 2020. Retrieved 26 June 2018.