Hibernoma
| Hibernoma | |
|---|---|
 | |
| CT scan: right-sided retroperitoneal hibernoma | |
| Symptoms | Small, slow-growing, painless, mobile lump just under skin[1] |
| Usual onset | Young adult[1] |
| Causes | Association with multiple endocrine neoplasiatype 1[1] |
| Prognosis | Good, generally do not recur[1] |
| Frequency | Rare, <% of benign and 1% of all adipocytic tumours[1] |
A hibernoma is a non-cancerous soft tissue tumor of brown fat, that present as a small, slow-growing, painless, mobile lump just under skin typically in a young adult.[1]
The term was originally used by the French anatomist Louis Gery in 1914.[2][3]
Signs and symptoms
Affected people present with a slow-growing, painless, solitary mass, usually of the subcutaneous tissues. It is much less frequently noted in the intramuscular tissue. It is not uncommon for symptoms to be present for years. Benign neoplasm with brown fat is noted.[4][5]
Diagnosis
Imaging findings
In general, imaging studies show a well-defined, heterogeneous mass, usually showing a mass which is hypointense to subcutaneous fat on magnetic resonance T1-weight images. Serpentine, thin, low signal bands (septations or vessels) are often seen throughout the tumor.
Pathology findings
From a macroscopic perspective, there is a well-defined, encapsulated or circumscribed mass, showing a soft, yellow tan to deep brown mass. The size ranges from 1 to 27 cm, although the mean is about 10 cm.[4]

The tumors histologically resemble brown fat. There are four histologic types recognized, but one is the most frequently seen (typical). There is a background of rich vascularity.
- Lobular type: Variable degrees of differentiation of uniform, round to oval cells with granular eosinophilic cells with prominent borders, alternating with coarsely multivacuolated fat cells (pale cells). There are usually small centrally placed nuclei without pleomorphism. The cells have large cytoplasmic lipid droplets interspersed throughout.[4][5]
- Myxoid variant: Loose, basophilic matrix, with thick fibrous septa, and foamy histiocytes
- Lipoma-like variant: Univacuolated lipocytes, with only isolated hibernoma cells
- Spindle cell variant: Spindle cell lipoma combined with hibernoma
Histochemistry
Oil Red O-positive droplets of cytoplasmic lipid can be seen in most cases
Immunohistochemistry
The neoplastic cells are S100 protein positive (approximately 80%), and show membrane and vacuole CD31 immunoreactivity. Uncoupling protein 1 (UCP1), a unique brown fat mitochondrial protein, is also positive.
Cytogenetics
There are structural rearrangements of 11q13-21, which are considered most characteristic. This alteration can be detected by metaphase fluorescent in situ hybridization (FISH). MEN1 gene (11q13.1) is most frequently deleted, while GARP gene (11q13.5) may also be involved.
Cytology
The fine needle aspiration smears show small, round, brown fat-like cells, with uniform, small cytoplasmic vacuoles and regular, small, round nuclei. There is usually a rich vascular background of branching capillaries. It is not uncommon to also have mature fat cells.
Differential diagnoses
It is important to separate hiberoma from adult rhabdomyoma, a granular cell tumor and a true liposarcoma.
Classification
This lesion has been called a fetal lipoma, lipoma of embryonic fat or a lipoma of immature fat.[4]
Management
Complete surgical excision is the treatment of choice, associated with an excellent long term clinical outcome.
Epidemiology
The tumor is rare, affecting adults in the 4th decade most commonly. Patients are usually younger than those who present with a lipoma. There is a slight male predominance. Hibernoma are most commonly identified in the subcutaneous and muscle tissue of the head and neck region (shoulders, neck, scapular), followed by thigh, back, chest, abdomen, and arms. In rare cases hibernoma may arise in bone tissue, however it is an incidental finding.[6]
Additional images
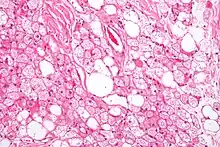 Hibernoma (intermediate magnification).
Hibernoma (intermediate magnification).
See also
References
- 1 2 3 4 5 6 WHO Classification of Tumours Editorial Board, ed. (2020). "1. Soft tissue tumours: hibernoma". Soft Tissue and Bone Tumours: WHO Classification of Tumours. Vol. 3 (5th ed.). Lyon (France): International Agency for Research on Cancer. pp. 31–33. ISBN 978-92-832-4503-2.
- ↑ "On the ultrastructure of hibernoma". Cancer. November 1975.
- ↑ Lexicon Orthopaedic Etymology. CRC Press. 1999. p. 147. ISBN 9789057025976. Archived from the original on 2021-04-13. Retrieved 2021-05-22.
- 1 2 3 4 Furlong, M. A.; Fanburg-Smith, J. C.; Miettinen, M. (2001). "The morphologic spectrum of hibernoma: A clinicopathologic study of 170 cases" (PDF). The American Journal of Surgical Pathology. 25 (6): 809–814. doi:10.1097/00000478-200106000-00014. PMID 11395560. Archived (PDF) from the original on 2019-09-06. Retrieved 2021-05-22.
- 1 2 Paul, M. A.; Koomen, A. R.; Blok, P. (1989). "Hibernoma, a brown fat tumour". The Netherlands Journal of Surgery. 41 (4): 85–87. PMID 2674772.
- ↑ Jerman, Anze (2015). "Intraosseous hibernoma: case report and tumour characterization". BJR Case Reports. British Institute of Radiology. 1 (3): 20150204. doi:10.1259/bjrcr.20150204. PMC 6180828. PMID 30363629.
Further reading
Lester D. R. Thompson; Bruce M. Wenig (2011). Diagnostic Pathology: Head and Neck: Published by Amirsys. Hagerstown, MD: Lippincott Williams & Wilkins. pp. 8:42–43. ISBN 978-1-931884-61-7.
External links
| Classification |
|---|