Intravenous ascorbic acid
| Intravenous ascorbic acid | |
|---|---|
 Intravenous bag and drip chamber on a pole, used to administer ascorbic acid solution through peripheral IV line | |
| Other names | Vitamin C, Ascorbate, L-ascorbic acid |
| ICD-10-PCS | Z51.81 |
| ICD-9-CM | 267 |
| This article is part of a series on |
| Alternative medicine |
|---|
 |
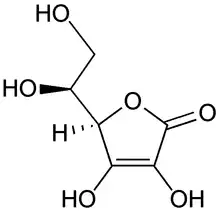
Intravenous Ascorbic Acid (also known as vitamin C or L-ascorbic acid), is a process that delivers soluble ascorbic acid directly into the bloodstream. It is not approved for use to treat any medical condition.[1]
The use of intravenous ascorbic acid as a proposed cancer treatment or co-treatment has been a controversial topic since the emergence of misleading data in the 1970s.[2]
Contraindications
High doses of ascorbic acid administered by intravenous infusion have been shown to increase the absorption of iron.[3] In individuals with hemochromatosis (a genetic disorder where the body takes up and stores too much iron), intravenous ascorbic acid is contraindicated as high dosages of ascorbic acid may result in iron overloading and therefore, lead to life-threatening complications such as heart disease, diabetes, or tissue damage.[4]
High dosages of ascorbic acid (such as those used in intravenous therapy) have been reported to cause some intestinal discomfort, diarrhoea, as well as increased gas and urination.[5]
Alternative medicine and unproven applications
Sepsis
The "Marik protocol", or "HAT" protocol, as devised by Paul E. Marik, proposed a combination of intravenous vitamin C, hydrocortisone, and thiamine as a treatment for preventing sepsis for people in intensive care. Marik's own initial research, published in 2017,[6] showed a dramatic evidence of benefit, leading to the protocol becoming popular among intensive care physicians,[7] especially after the protocol received attention on social media and National Public Radio, drawing criticism of science by press conference from the wider medical community.[8][9] Subsequent independent research failed to replicate Marik's positive results, indicating the possibility that they had been compromised by bias.[9][10] A systematic review of trials in 2021 found that the claimed benefits of the protocol could not be confirmed.[11]
Pharmacology
Mechanism of action
Ascorbic acid operates as an anti-oxidant and essential enzyme cofactor in the human body. In in vitro studies, the primary mechanism of high dosage intravenous ascorbic acid can be related to ascorbic acid's pro-oxidant activity, whereby hydrogen peroxide is formed.[12][13][14] In the extracellular fluid of cells, ascorbic acid dissociates into an ascorbate radical upon the reduction of transition metal ions, such as ferric or cupric cations.[12] These transition metal ions will then reduce dissolved oxygen into a superoxide radical- this will then react with hydrogen to form hydrogen peroxide.[13]
Furthermore, according to Fenton chemistry, these transition metal ions can be further oxidised by hydrogen peroxide to generate a highly reactive hydroxyl radical.[15] The formation of hydrogen peroxide and hydroxyl radicals is believed to induce cytotoxicity and apoptosis of cancer cells.[15] Although many in vitro studies have studied hydrogen peroxide generation by ascorbic acid, the pharmacological mechanism of intravenous ascorbic acid in vivo is still unclear.[15]
History
Pioneering research
Although the pharmacology of ascorbic acid had been studied since its discovery in the 1930s,[16] the method of administration and its medicinal potential to human patients was not investigated until the 1940s.[17] In 1949, American physician, Frederick Klenner, published his scientific report, “The Treatment of Poliomyelitis and Other Virus Diseases with ascorbic acid”,[18] which detailed the use of intravenous ascorbic acid to treat polio in children.[17] Although Klenner's attempts were unsuccessful, his research pioneered future studies investigating the medicinal role of intravenous ascorbic acid. Klenner's work was recognised by Linus Pauling in the foreword to the Clinical Guide: "Dr. Fred Klenner's early research reports provide much information on the use of high-dose ascorbic acid for the prevention and cure of many diseases, and these reports are still important."[19]
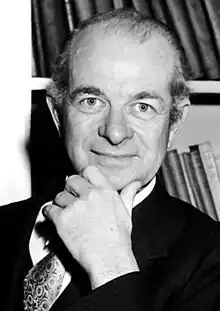
Linus Pauling
Nobel Prize winner and biochemist, Linus Pauling, was pivotal in the re-emergence of intravenous ascorbic acid research. Over the course of the 1970s, Pauling would begin a long-term collaboration with fellow physician, Ewan Cameron, on the medical potential of intravenous ascorbate acid as cancer therapy in terminally ill patients. In 1976, Pauling and Cameron co-authored a study whereby a group of 100 terminal cancer patients underwent supplementary ascorbic acid therapy (10g/day by intravenous infusion and oral thereafter) and the control group of 1,000 patients did not.[20] Their findings reported that the survival rate of the terminal cancer patients increased by four-fold, compared to the control group, stating that: "the treatment of ascorbate in amounts of 10g/day or more is of real value in extending the life of patients with advanced cancer."[20]
Subsequent studies by Pauling and Cameron hypothesised that ascorbic acid's role in enhanced collagen production would lead to the encapsulation of tumours and thus, protect normal tissue from metastasis.[21] Following these findings, Pauling became a strong advocate for vitamin megadosing and continued to investigate the medicinal potential of intravenous ascorbic acid across a range of illnesses, including: HIV transmission, the common cold, atherosclerosis, and angina pectoris.[22][23][24]
Medical controversy
The efficacy of intravenous ascorbic acid therapy came under scrutiny of the medical and science community, following the numerous high-profile studies authored by Linus Pauling in the 1970s.[14] The experimental design of Pauling and Cameron's 1976 publication, "Supplemental ascorbate in the supportive treatment of cancer",[20] had garnered considerable criticism as it was neither randomised nor placebo controlled. To test the validity of Pauling and Cameron's findings, the Mayo Clinic conducted three independent experiments in 1979, 1983 and 1985, whereby terminal cancer patients were given doses of oral ascorbic acid under randomised, double bind and placebo-controlled conditions.[25][26][27] All studies concluded that high doses of oral ascorbic acid were not effective against cancer.
The use of intravenous ascorbic acid in the treatment of cancer has been a contentious issue. There is no evidence to indicate that intravenous ascorbic acid therapy can cure cancer.[28][27] According to the U.S. Food and Drug Administration (FDA), high-dose vitamin C (such as intravenous ascorbic acid therapy) has not been approved as a treatment for cancer or any other medical condition.[1]
There many been multiple studies devoted to investigating the medicinal properties of ascorbic acid. The use of high-dosage intravenous ascorbic acid as a cancer treatment was first promoted by Linus Pauling and Ewan Cameron in the 1970s;[20][21] however, these findings were not reproduced using oral administration by subsequent Mayo Clinic studies in the 1980s.[25][26][27] In 2010, an academic review which detailed 33 years of ascorbic acid and cancer research stated: "we still do not know whether Vitamin C has any clinically significant anti-tumor activity. Nor do we know which histological types of cancers, if any, are susceptible to this agent. Finally, we don't know what the recommended dose of Vitamin C is, if there is indeed such a dose, that can produce an anti-tumor response".[29]
Research
The turn of the 21st century saw a renewed interest in the medical potential of intravenous ascorbic acid therapy. In the early 2010s, in vitro preclinical and clinical trials were undertaken to investigate the pharmacological mechanism of action of intravenous ascorbic acid therapy.[30][31] These findings demonstrated ascorbic acid's pro-oxidant capabilities to produce hydrogen peroxide and thus, proposed a possible pharmacological mechanism of action against cancer cells. Nonetheless, ascorbic acid's potential as an anti-tumour therapy is still dubious, as other pro-oxidant substances (such as menadione[32][33]) have been unsuccessful in the treatment of cancer patients.[34]
See also
References
- 1 2 "The Vitamin C Foundation - 514071 - 04/17/2017". U.S. Food and Drug Administration. 2019-04-23. Retrieved 2019-06-07.
- ↑ Nabzdyk CS, Bittner EA (October 2018). "Vitamin C in the critically ill - indications and controversies". World Journal of Critical Care Medicine. 7 (5): 52–61. doi:10.5492/wjccm.v7.i5.52. PMC 6201324. PMID 30370227.
- ↑ Jacob RA, Sotoudeh G (March 2002). "Vitamin C function and status in chronic disease". Nutrition in Clinical Care. 5 (2): 66–74. doi:10.1046/j.1523-5408.2002.00005.x. PMID 12134712.
- ↑ Institute of Medicine (US) Panel on Dietary Antioxidants Related Compounds (2000-04-11). Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. doi:10.17226/9810. ISBN 9780309069359. PMID 25077263.
- ↑ Ohno S, Ohno Y, Suzuki N, Soma G, Inoue M (March 2009). "High-dose vitamin C (ascorbic acid) therapy in the treatment of patients with advanced cancer". Anticancer Research. 29 (3): 809–15. PMID 19414313.
- ↑ Marik, Paul E.; Khangoora, Vikramjit; Rivera, Racquel; Hooper, Michael H.; Catravas, John (2017). "Hydrocortisone, Vitamin C, and Thiamine for the Treatment of Severe Sepsis and Septic Shock". Chest. Elsevier BV. 151 (6): 1229–1238. doi:10.1016/j.Chest.2016.11.036. ISSN 0012-3692. PMID 27940189. S2CID 3509326.
- ↑ "The Marik Protocol: Have We Found a "Cure" for Severe Sepsis and Septic Shock? - Emergency Medicine Blog". REBEL EM - Emergency Medicine Blog. 2017-04-07. Retrieved 2021-07-22.
- ↑ "Vitamin C Drug Cocktail for Sepsis". HealthManagement. July 9, 2019. Retrieved 2021-09-24.
{{cite web}}: CS1 maint: url-status (link) - 1 2 Rubin R (July 2019). "Wide Interest in a Vitamin C Drug Cocktail for Sepsis Despite Lagging Evidence". JAMA. 322 (4): 291–293. doi:10.1001/jama.2019.7936. PMID 31268477. S2CID 195788169.
- ↑ ""Ethically and morally unacceptable": Reaction to vitamin C for sepsis trial". Dietary supplements, Nutraceuticals, Functional foods, Health ingredients, Herbals. 2020-01-28. Retrieved 2021-07-22.
- ↑ Lee YR, Vo K, Varughese JT (May 2021). "Benefits of combination therapy of hydrocortisone, ascorbic acid and thiamine in sepsis and septic shock: A systematic review". Nutr Health: 2601060211018371. doi:10.1177/02601060211018371. PMID 34039089. S2CID 235215735.
- 1 2 Carr AC, Cook J (2018-08-23). "Intravenous Vitamin C for Cancer Therapy - Identifying the Current Gaps in Our Knowledge". Frontiers in Physiology. 9: 1182. doi:10.3389/fphys.2018.01182. PMC 6115501. PMID 30190680.
- 1 2 Vissers MC, Das AB (2018-07-03). "Potential Mechanisms of Action for Vitamin C in Cancer: Reviewing the Evidence". Frontiers in Physiology. 9: 809. doi:10.3389/fphys.2018.00809. PMC 6037948. PMID 30018566.
- 1 2 Verrax J, Calderon PB (December 2008). "The controversial place of vitamin C in cancer treatment". Biochemical Pharmacology. 76 (12): 1644–52. doi:10.1016/j.bcp.2008.09.024. PMID 18938145.
- 1 2 3 Fritz H, Flower G, Weeks L, Cooley K, Callachan M, McGowan J, et al. (July 2014). "Intravenous Vitamin C and Cancer: A Systematic Review". Integrative Cancer Therapies. 13 (4): 280–300. doi:10.1177/1534735414534463. PMID 24867961.
- ↑ Carpenter KJ (2012). "The discovery of vitamin C". Annals of Nutrition & Metabolism. 61 (3): 259–64. doi:10.1159/000343121. PMID 23183299. S2CID 37436503.
- 1 2 "Intravenous Vitamin C: The Historical Progression". PaulingBlog. 2017-10-18. Retrieved 2019-05-20.
- ↑ "The Treatment of Poliomyelitis and Other Virus Diseases with Vitamin C". www.seanet.com. Retrieved 2019-05-20.
- ↑ "Clinical Guide to the Use of Vitamin C". www.seanet.com. Retrieved 2019-05-20.
- 1 2 3 4 Cameron E, Pauling L (October 1976). "Supplemental ascorbate in the supportive treatment of cancer: Prolongation of survival times in terminal human cancer". Proceedings of the National Academy of Sciences of the United States of America. 73 (10): 3685–9. Bibcode:1976PNAS...73.3685C. doi:10.1073/pnas.73.10.3685. PMC 431183. PMID 1068480.
- 1 2 Mikirova N, Casciari J, Riordan N, Hunninghake R (August 2013). "Clinical experience with intravenous administration of ascorbic acid: achievable levels in blood for different states of inflammation and disease in cancer patients". Journal of Translational Medicine. 11: 191. doi:10.1186/1479-5876-11-191. PMC 3751545. PMID 23947403.
- ↑ Pauling L (January 1973). "Ascorbic acid and the common cold". Scottish Medical Journal. 18 (1): 1–2. doi:10.1177/003693307301800101. PMID 4577802. S2CID 28875346.
- ↑ Harakeh S, Jariwalla RJ, Pauling L (September 1990). "Suppression of human immunodeficiency virus replication by ascorbate in chronically and acutely infected cells". Proceedings of the National Academy of Sciences of the United States of America. 87 (18): 7245–9. Bibcode:1990PNAS...87.7245H. doi:10.1073/pnas.87.18.7245. PMC 54720. PMID 1698293.
- ↑ Rath M, Pauling L (August 1990). "Hypothesis: lipoprotein(a) is a surrogate for ascorbate". Proceedings of the National Academy of Sciences of the United States of America. 87 (16): 6204–7. Bibcode:1990PNAS...87.6204R. doi:10.1073/pnas.87.16.6204. PMC 54501. PMID 2143582.
- 1 2 Creagan ET, Moertel CG, O'Fallon JR, Schutt AJ, O'Connell MJ, Rubin J, Frytak S (September 1979). "Failure of high-dose vitamin C (ascorbic acid) therapy to benefit patients with advanced cancer. A controlled trial". The New England Journal of Medicine. 301 (13): 687–90. doi:10.1056/NEJM197909273011303. PMID 384241.
- 1 2 Tschetter L, Creagan E, O'Fallon J (1983). "A community-based study of vitamin C (ascorbic acid) in patients with advanced cancer". Proceedings of the American Society of Clinical Oncology. 2: 92.
- 1 2 3 Moertel CG, Fleming TR, Creagan ET, Rubin J, O'Connell MJ, Ames MM (January 1985). "High-dose vitamin C versus placebo in the treatment of patients with advanced cancer who have had no prior chemotherapy. A randomized double-blind comparison". The New England Journal of Medicine. 312 (3): 137–41. doi:10.1056/NEJM198501173120301. PMID 3880867.
- ↑ Klimant E, Wright H, Rubin D, Seely D, Markman M (April 2018). "Intravenous vitamin C in the supportive care of cancer patients: a review and rational approach". Current Oncology. 25 (2): 139–48. doi:10.3747/co.25.3790. PMC 5927785. PMID 29719430.
- ↑ Cabanillas F (September 2010). "Vitamin C and cancer: what can we conclude--1,609 patients and 33 years later?". Puerto Rico Health Sciences Journal. 29 (3): 215–7. PMID 20799507.
- ↑ Parrow NL, Leshin JA, Levine M (December 2013). "Parenteral ascorbate as a cancer therapeutic: a reassessment based on pharmacokinetics". Antioxidants & Redox Signaling. 19 (17): 2141–56. doi:10.1089/ars.2013.5372. PMC 3869468. PMID 23621620.
- ↑ Fritz H, Flower G, Weeks L, Cooley K, Callachan M, McGowan J, et al. (July 2014). "Intravenous Vitamin C and Cancer: A Systematic Review". Integrative Cancer Therapies. 13 (4): 280–300. doi:10.1177/1534735414534463. PMID 24867961.
- ↑ Tetef M, Margolin K, Ahn C, Akman S, Chow W, Leong L, et al. (1995). "Mitomycin C and menadione for the treatment of lung cancer: a phase II trial". Investigational New Drugs. 13 (2): 157–62. doi:10.1007/BF00872865. PMID 8617579. S2CID 10086469.
- ↑ Margolin KA, Akman SA, Leong LA, Morgan RJ, Somlo G, Raschko JW, et al. (1995). "Phase I study of mitomycin C and menadione in advanced solid tumors". Cancer Chemotherapy and Pharmacology. 36 (4): 293–8. doi:10.1007/BF00689046. PMID 7628048. S2CID 7283959.
- ↑ Borst P (December 2008). "Mega-dose vitamin C as therapy for human cancer?". Proceedings of the National Academy of Sciences of the United States of America. 105 (48): E95, author reply E96. Bibcode:2008PNAS..105E..95B. doi:10.1073/pnas.0809328105. PMC 2596258. PMID 19033231.