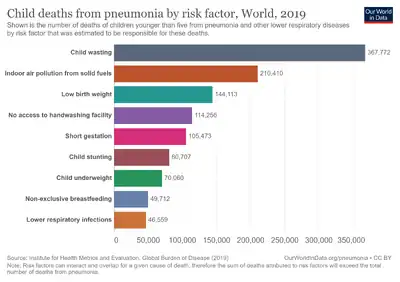
Low birth weight
| Low birth weight | |
|---|---|
 | |
| Low birth weight may be a result of preterm birth. | |
| Specialty | Neonatology |
Low birth weight (LBW) is defined by the World Health Organization as a birth weight of an infant of 2,499 g (5 lb 8.1 oz) or less, regardless of gestational age.[1] Infants born with LBW have added health risks which require close management, often in a neonatal intensive care unit (NICU). They are also at increased risk for long-term health conditions which require follow-up over time.
Classification
Birth weight may be classified as:[2]
- High birth weight (macrosomia): greater than 4,200 g (9 lb 4 oz)
- Normal weight (term delivery): 2,500–4,200 g (5 lb 8 oz–9 lb 4 oz)
- Low birth weight: less than 2,500 g (5 lb 8 oz)
- Very low birth weight: less than 1,500 g (3 lb 5 oz)
- Extremely low birth weight: less than 1,000 g (2 lb 3 oz)
Causes
LBW is either caused by preterm birth (that is, a low gestational age at birth, commonly defined as younger than 37 weeks of gestation) or the infant being small for gestational age (that is, a slow prenatal growth rate), or a combination of both.
In general, risk factors in the mother that may contribute to low birth weight include young ages, multiple pregnancies, previous LBW infants, poor nutrition, heart disease or hypertension, untreated celiac disease, substance use disorder, excessive alcohol use, and insufficient prenatal care. It can also be caused by prelabor rupture of membranes.[3] Environmental risk factors include smoking, lead exposure, and other types of air pollutions.[4][5][6]
Preterm birth
The mechanism of preterm birth is heterogeneous and poorly understood. It may be tied to one or more of the following processes: premature fetal endocrine activation, intrauterine inflammation, over-distension of the uterus, and endometrial bleeding. A prominent risk factor for preterm birth is prior history of preterm delivery. However, there is no reliable protocol for screening and prevention of preterm birth.[7]
Small for gestational age
Infants born small for gestational age may be constitutionally small, with no associated pathologic process. Others have intrauterine growth restriction (IUGR) due to any of various pathologic processes. Babies with chromosomal abnormalities or other congenital anomalies may manifest IUGR as part of their syndrome. Problems with the placenta can prevent it from providing adequate oxygen and nutrients to the fetus, resulting in growth restriction. Infections during pregnancy that affect the fetus, such as rubella, cytomegalovirus, toxoplasmosis, and syphilis, may also affect the baby's weight.
Environmental factors
Maternal tobacco smoking doubles risk of LBW for the infant.[8][9] More recently, passive maternal smoking has been examined for possible effects on birth weight, and has been shown to increase risk of LBW by 16%.[10]
Air pollutants
The combustion products of solid fuel in developing countries can cause many adverse health issues in people. Because a majority of pregnant women in developing countries, where rate of LBW is high, are heavily exposed to indoor air pollution, increased relative risk translates into substantial population attributable risk of 21% of LBW.[11]
Particulate matter, a component of ambient air pollution, is associated with increased risk of low birth weight.[12][13] Because particulate matter is composed of extremely small particles, even nonvisible levels can be inhaled and present harm to the fetus.[14] Particulate matter exposure can cause inflammation, oxidative stress, endocrine disruption, and impaired oxygen transport access to the placenta, all of which are mechanisms for heightening the risk of low birth weight.[15] To reduce exposure to particulate matter, pregnant women can monitor the EPA’s Air Quality Index and take personal precautionary measures such as reducing outdoor activity on low quality days, avoiding high-traffic roads/intersections, and/or wearing personal protective equipment (i.e., facial mask of industrial design). Indoor exposure to particulate matter can also be reduced through adequate ventilation, as well as use of clean heating and cooking methods.[16][17]
A correlation between maternal exposure to carbon monoxide (CO) and low birth weight has been reported that the effect on birth weight of increased ambient CO was as large as the effect of the mother smoking a pack of cigarettes per day during pregnancy.[18] It has been revealed that adverse reproductive effects (e.g., risk for LBW) were correlated with maternal exposure to CO emissions in Eastern Europe and North America.[19] Mercury is a known toxic heavy metal that can harm fetal growth and health, and there has been evidence showing that exposure to mercury (via consumption of large oily fish) during pregnancy may be related to higher risks of LBW in the offspring.[20]
Other exposures
Elevated blood lead levels in pregnant women, even those well below the US Centers for Disease Control and Prevention's 10 ug/dL "level of concern", can cause miscarriage, premature birth, and LBW in the offspring.[21] Exposure of pregnant women to airplane noise was found to be associated with low birth weight via adverse effects on fetal growth.[22] Prevalence of low birth weight in Japan is associated with radiation doses from the Fukushima accidents of March 2011.[23]
Periodontal health
Low birth weight, preterm birth and preeclampsia have been associated with maternal periodontal disease, though the strength of the observed associations is inconsistent and varies according to the population studied, the means of periodontal assessment and the periodontal disease classification employed.[24] The risk of low birth weight can be reduced with treatment of the periodontal disease. This therapy is safe during pregnancy and reduces the inflammatory burden, thus decreasing risk for preterm birth and low birth weight.[25]
Management
Temperature regulation


LBW newborns are at increased risk of hypothermia due to decreased brown fat stores. Plastic wraps, heated pads, and skin-to-skin contact decrease risk of hypothermia immediately after delivery. One or more of these interventions may be employed, though combinations incur risk of hyperthermia.[26] Warmed incubators in the NICU aid in thermoregulation for LBW infants.
Fluid and electrolyte balance
Frequent clinical monitoring of volume status and checking of serum electrolytes (up to three times daily) is appropriate to prevent dehydration, fluid overload, and electrolyte imbalance.[27] VLBW newborns have an increased body surface to weight ratio, increasing risk for insensible fluid losses and dehydration.[28] Humidified incubators and skin emollients can lessen insensible fluid loss in VLBW newborns.[27] However, fluid overloading is not benign; it is associated with increased risk of congestive heart failure, necrotizing enterocolitis, and mortality. A degree of fluid restriction mitigates these risks.[27]
VLBW newborns are at risk for electrolyte imbalances due to the relative immaturity of the nephrons in their kidneys. The kidneys are not equipped to handle large sodium loads. Therefore, if normal saline is given, the sodium level may become elevated, which may prompt the clinician to give more fluids. Sodium restriction has been shown to prevent fluid overload.[27] Potassium must also be monitored carefully, as immature aldosterone sensitivity and sodium-potassium pumping increases risk for hyperkalemia and cardiac arrhythmias.[27]
VLBW newborns are frequently found to have a persistently patent ductus arteriosus (PDA). If present, it is important to evaluate whether the PDA is causing increased circulatory volume, thus posing risk for heart failure. Signs of clinically significant PDA include widened pulse pressure and bounding pulses. In newborns with significant PDA, fluid restriction may avoid the need for surgical or medical therapy to close it.[27]
Approach to nutrition
As their gastrointestinal systems are typically unready for enteral feeds at the time of birth, VLBW infants require initial parenteral infusion of fluids, macronutrients, vitamins, and micronutrients.[28]
Energy needs
Decreased activity compared to normal weight newborns may decrease energy requirements, while comorbidities such as bronchopulmonary dysplasia may increase them. Daily weight gain can reveal whether a VLBW newborn is receiving adequate calories. Growth of 21 g/kg/day, mirroring in utero growth, is a target for VLBW and ELBW neonates.[28]
Enteral sources
Upon transitioning to enteral nutrition, human milk is preferable to formula initially in VLBW newborns because it speeds up development of the intestinal barrier and thereby reduces risk of necrotizing enterocolitis,[28] with an absolute risk reduction of 4%.[29] Donor human milk and maternal expressed breast milk are both associated with this benefit.[30] One drawback of human milk is the imprecision in its calorie content. The fat content in human milk varies greatly among women; therefore, the energy content of human milk cannot be known as precisely as formula.[28] Each time human milk is transferred between containers, some of the fat content may stick to the container, decreasing the energy content. Minimizing transfers of human milk between containers decreases the amount of energy loss.[28] Formula is associated with greater linear growth and weight gain than donor breast milk in LBW infants.[30]
Individual nutrient considerations
VLBW newborns are at increased risk for hypoglycemia due to decreased energy reserves and large brain mass to body mass ratio. Hypoglycemia may be prevented by intravenous infusion of glucose, amino acids, and lipids.[28] These patients are also at risk of hyperglycemia due to immature insulin secretion and sensitivity. However, insulin supplementation is not recommended due to the possible adverse effect of hypoglycemia, which is more dangerous.[28]
VLBW newborns have increased need for amino acids to mirror in utero nutrition. Daily protein intake above 3.0 g/kg is associated with improved weight gain for LBW infants.[31] ELBW newborns may require as much as 4 g/kg/day of protein.[28]
Due to the limited solubility of calcium and phosphorus in parenteral infusions, VLBW infants receiving parenteral nutrition will be somewhat deficient of these elements and will require clinical monitoring for osteopenia.[28]
Hematology
One Cochrane review showed administration of erythropoietin (EPO) decreases later need for blood transfusions, and also is associated with protection against necrotizing enterocolitis and intraventricular hemorrhage. EPO is safe and does not increase risk of mortality or retinopathy of prematurity.[32]
Prognosis
Perinatal outcomes

LBW is closely associated with fetal and perinatal mortality and morbidity, inhibited growth and cognitive development, and chronic diseases later in life. At the population level, the proportion of babies with a LBW is an indicator of a multifaceted public-health problem that includes long-term maternal malnutrition, ill health, hard work and poor health care in pregnancy. On an individual basis, LBW is an important predictor of newborn health and survival and is associated with higher risk of infant and childhood mortality.[33]
Low birth weight constitutes as sixty to eighty percent of the infant mortality rate in developing countries. Infant mortality due to low birth weight is usually directly causal, stemming from other medical complications such as preterm birth, PPROM,[34] poor maternal nutritional status, lack of prenatal care, maternal sickness during pregnancy, and an unhygienic home environment.[35]
Long term outcomes
Hyponatremia in the newborn period is associated with neurodevelopmental conditions such as spastic cerebral palsy and sensorineural hearing loss. Rapid correction of hyponatremia (faster than 0.4 mEq/L/hour) perinatally is also associated with neurodevelopmental adverse effects.[27] Among VLBW children, risk for cognitive impairment is increased with lower birth weight, male sex, nonwhite ethnicity, and lower parental education level. There is no clear association between brain injury in the neonatal period and later cognitive impairment.[36] Additionally, low birth weight has associations with cardiovascular diseases later in life, especially in cases of large increases in weight during childhood.[37][38][39][40]
Epidemiology
The World Health Organization (WHO) estimates the worldwide prevalence of low birth weight at 15% as of 2014, and varies by region: Sub-Saharan Africa, 13%; South Asia, 28%; East Asia and the Pacific, 6%; Latin America and the Caribbean, 9%.[41]
Aggregate prevalence of LBW in United Nations-designated Least Developed Countries[42] is 13%.[41]
The WHO has set a goal of reducing worldwide prevalence of LBW by 30% through public health interventions including improved prenatal care and women's education.[41]
In the United States, the Centers for Disease Control and Prevention (CDC) reports 313,752 LBW infants in 2018, for a prevalence of 8.28%.[43]
This is increased from an estimated 6.1% prevalence in 2011 by the Agency for Healthcare Research and Quality (AHRQ).[44]
The CDC reported prevalence of VLBW at 1.38% in 2018, similar to the 2011 AHRQ estimate.[44]
References
- ↑ P07 - Disorders related to short gestation and low birth weight Archived 2014-11-02 at the Wayback Machine in ICD-10
- ↑ "eMedicine - Extremely Low Birth Weight Infant: Article by KN Siva Subramanian, MD". Archived from the original on 2008-11-21. Retrieved 2007-11-28.
- ↑ Rizzo, Nicola; Simonazzi, Giuliana; Curti, Alessandra (2015-09-24). "Obstetrical risk factors of ELBW". Italian Journal of Pediatrics. 41 (Suppl 1): A35. doi:10.1186/1824-7288-41-S1-A35. ISSN 1824-7288. PMC 4595176.
- ↑ "Labor and delivery - Low Birth Weight". Umm.edu. 2008-10-22. Archived from the original on 2011-08-20. Retrieved 2011-01-05.
- ↑ Tersigni, C.; Castellani, R.; de Waure, C.; Fattorossi, A.; De Spirito, M.; Gasbarrini, A.; Scambia, G.; Di Simone, N. (2014). "Celiac disease and reproductive disorders: meta-analysis of epidemiologic associations and potential pathogenic mechanisms". Human Reproduction Update. 20 (4): 582–593. doi:10.1093/humupd/dmu007. ISSN 1355-4786. PMID 24619876.
- ↑ Saccone G, Berghella V, Sarno L, Maruotti GM, Cetin I, Greco L, Khashan AS, McCarthy F, Martinelli D, Fortunato F, Martinelli P (Oct 9, 2015). "Celiac disease and obstetric complications: a systematic review and metaanalysis". Am J Obstet Gynecol. 214 (2): 225–34. doi:10.1016/j.ajog.2015.09.080. PMID 26432464.
- ↑ Simhan HN, Caritis SN (2007). "Prevention of Preterm Delivery". New England Journal of Medicine. 357 (5): 477–487. doi:10.1056/NEJMra050435. PMID 17671256.
- ↑ Saygin Avsar, Tuba (2021). "Health outcomes of smoking during pregnancy and the postpartum period: an umbrella review". BMC Pregnancy and Childbirth. 21 (1): 43–49. doi:10.1186/s12884-021-03729-1. PMID 7995767. S2CID 232360282. Archived from the original on 2022-06-20. Retrieved 2022-08-19.
- ↑ Knopik, Valerie S. (2009). "Maternal smoking during pregnancy and child outcomes: real or spurious effect?". Developmental Neuropsychology. 34 (1): 1–36. doi:10.1080/87565640802564366. ISSN 1532-6942. PMC 3581055. PMID 19142764.
- ↑ Salmasi, Giselle; Grady, Rosheen; Jones, Jennifer; McDonald, Sarah D.; Knowledge Synthesis Group (2010). "Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses". Acta Obstetricia et Gynecologica Scandinavica. 89 (4): 423–441. doi:10.3109/00016340903505748. ISSN 1600-0412. PMID 20085532. S2CID 9206564.
- ↑ Pope, Daniel P.; Mishra, Vinod; Thompson, Lisa; Siddiqui, Amna Rehana; Rehfuess, Eva A.; Weber, Martin; Bruce, Nigel G. (2010). "Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries". Epidemiologic Reviews. 32: 70–81. doi:10.1093/epirev/mxq005. ISSN 1478-6729. PMID 20378629.
- ↑ EPA, OAR, US (2014-04-09). "Criteria Air Pollutants". www.epa.gov. Archived from the original on 2020-11-28. Retrieved 2017-03-31.
- ↑ Li, Xiangyu; Huang, Shuqiong; Jiao, Anqi; Yang, Xuhao; Yun, Junfeng; Wang, Yuxin; Xue, Xiaowei; Chu, Yuanyuan; Liu, Feifei; Liu, Yisi; Ren, Meng (Aug 2017). "Association between ambient fine particulate matter and preterm birth or term low birth weight: An updated systematic review and meta-analysis". Environmental Pollution. 227: 596–605. doi:10.1016/j.envpol.2017.03.055. ISSN 1873-6424. PMID 28457735. Archived from the original on 2022-07-03. Retrieved 2022-08-19.
- ↑ "CDC - Air Quality - Particle Pollution". www.cdc.gov. Archived from the original on 2017-04-01. Retrieved 2017-03-31.
- ↑ Erickson, Anders C.; Arbour, Laura (2014-11-26). "The Shared Pathoetiological Effects of Particulate Air Pollution and the Social Environment on Fetal-Placental Development". Journal of Environmental and Public Health. 2014: 901017. doi:10.1155/2014/901017. ISSN 1687-9805. PMC 4276595. PMID 25574176.
- ↑ "Particulate matter". EPA. 2009-05-19. Archived from the original on 2009-06-04.
- ↑ US EPA National Center for Environmental Assessment, Research Triangle Park NC, Environmental Media Assessment Group; Sacks, Jason. "2009 Final Report: Integrated Science Assessment for Particulate Matter". cfpub.epa.gov. Archived from the original on 2017-04-01. Retrieved 2017-03-31.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ↑ Lewtas, Joellen (Nov 2007). "Air pollution combustion emissions: characterization of causative agents and mechanisms associated with cancer, reproductive, and cardiovascular effects". Mutation Research. 636 (1–3): 95–133. doi:10.1016/j.mrrev.2007.08.003. ISSN 0027-5107. PMID 17951105. Archived from the original on 2022-04-23. Retrieved 2022-08-19.
- ↑ Townsend CL, Maynard RL (Oct 2002). "Effects on health of prolonged exposure to low concentrations of carbon monoxide". Occup Environ Med. 59 (10): 708–11. doi:10.1136/oem.59.10.708. PMC 1740215. PMID 12356933.
- ↑ Gochfeld M, Burger J (Aug 2005). "Good fish/bad fish: a composite benefit-risk by dose curve". Neurotoxicology. 26 (4): 511–20. doi:10.1016/j.neuro.2004.12.010. PMID 15979722.
- ↑ Cleveland, Lisa M.; Minter, Monica L.; Cobb, Kathleen A.; Scott, Anthony A.; German, Victor F. (Oct 2008). "Lead hazards for pregnant women and children: part 1: immigrants and the poor shoulder most of the burden of lead exposure in this country. Part 1 of a two-part article details how exposure happens, whom it affects, and the harm it can do". The American Journal of Nursing. 108 (10): 40–49, quiz 50. doi:10.1097/01.NAJ.0000337736.76730.66. ISSN 1538-7488. PMID 18827541. Archived from the original on 2022-07-25. Retrieved 2022-08-19.
- ↑ Kawada T (Feb 2004). "The effect of noise on the health of children". Journal of Nippon Medical School. 71 (1): 5–10. doi:10.1272/jnms.71.5. PMID 15129589.
- ↑ Scherb H, Hayashi K (July 2020). "Spatiotemporal association of low birth weight with Cs-137 deposition at the prefecture level in Japan after the Fukushima nuclear power plant accidents: an analytical-ecologic epidemiological study". Environmental Health. 19 (1): 82. doi:10.1186/s12940-020-00630-w. PMC 7346451. PMID 32646457.
- ↑ Sanz, M (April 2013). "Periodontitis and adverse pregnancy outcomes: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases". J Periodontol. 84 (4 suppl): S164–9. doi:10.1902/jop.2013.1340016. PMID 23631576.
- ↑ Shah, Monali (November 2013). "Effect of nonsurgical periodontal therapy during gestation period on adverse pregnancy outcome: a systematic review". J Matern Fetal Neonatal Med. 26 (17): 1691–5. doi:10.3109/14767058.2013.799662. PMID 23617740. S2CID 23564952.
- ↑ McCall, Emma M.; Alderdice, Fiona; Halliday, Henry L.; Vohra, Sunita; Johnston, Linda (12 Feb 2018). "Interventions to prevent hypothermia at birth in preterm and/or low birth weight infants". The Cochrane Database of Systematic Reviews. 2018 (2): CD004210. doi:10.1002/14651858.CD004210.pub5. ISSN 1469-493X. PMC 6491068. PMID 29431872.
- 1 2 3 4 5 6 7 Evidence-based handbook of neonatology. Oh, William. New Jersey: World Scientific. 2011. pp. 267–290. ISBN 978-981-4313-46-9. OCLC 775591575.
{{cite book}}: CS1 maint: others (link) - 1 2 3 4 5 6 7 8 9 10 Evidence-based handbook of neonatology. Oh, William. New Jersey: World Scientific. 2011. pp. 291–315. ISBN 978-981-4313-46-9. OCLC 775591575.
{{cite book}}: CS1 maint: others (link) - ↑ Miller, Jacqueline; Tonkin, Emma; Damarell, Raechel A.; McPhee, Andrew J.; Suganuma, Machiko; Suganuma, Hiroki; Middleton, Philippa F.; Makrides, Maria; Collins, Carmel T. (2018-05-31). "A Systematic Review and Meta-Analysis of Human Milk Feeding and Morbidity in Very Low Birth Weight Infants". Nutrients. 10 (6): 707. doi:10.3390/nu10060707. ISSN 2072-6643. PMC 6024377. PMID 29857555.
- 1 2 Quigley, Maria; Embleton, Nicholas D.; McGuire, William (July 19, 2019). "Formula versus donor breast milk for feeding preterm or low birth weight infants". The Cochrane Database of Systematic Reviews. 7: CD002971. doi:10.1002/14651858.CD002971.pub5. ISSN 1469-493X. PMC 6640412. PMID 31322731.
- ↑ Fenton, Tanis R.; Premji, Shahirose S.; Al-Wassia, Heidi; Sauve, Reg S. (2014-04-21). "Higher versus lower protein intake in formula-fed low birth weight infants". The Cochrane Database of Systematic Reviews (4): CD003959. doi:10.1002/14651858.CD003959.pub3. ISSN 1469-493X. PMC 7104240. PMID 24752987.
- ↑ Ohlsson, Arne; Aher, Sanjay M. (2020-02-11). "Early erythropoiesis-stimulating agents in preterm or low birth weight infants". The Cochrane Database of Systematic Reviews. 2: CD004863. doi:10.1002/14651858.CD004863.pub6. ISSN 1469-493X. PMC 7014351. PMID 32048730.
- ↑ Stevens-Simon C, Orleans M (Sep 1999). "Low-birthweight prevention programs: the enigma of failure". Birth. 26 (3): 184–91. doi:10.1046/j.1523-536x.1999.00184.x. PMID 10655819.
- ↑ Kalikkot Thekkeveedu, Renjithkumar; Guaman, Milenka Cuevas; Shivanna, Binoy (November 2017). "Bronchopulmonary dysplasia: A review of pathogenesis and pathophysiology". Respiratory Medicine. 132: 170–177. doi:10.1016/j.rmed.2017.10.014. ISSN 1532-3064. PMC 5729938. PMID 29229093.
- ↑ Andrews, K.M.; Brouillette, D.B; Brouillette, R.T. (2008). "Mortality, Infant". Encyclopedia of Infant and Early Childhood Development. pp. 343–359. doi:10.1016/B978-012370877-9.00084-0. ISBN 9780123708779.
- ↑ Linsell, Louise; Malouf, Reem; Morris, Joan; Kurinczuk, Jennifer J.; Marlow, Neil (Dec 2015). "Prognostic Factors for Poor Cognitive Development in Children Born Very Preterm or With Very Low Birth Weight: A Systematic Review". JAMA Pediatrics. 169 (12): 1162–1172. doi:10.1001/jamapediatrics.2015.2175. ISSN 2168-6211. PMC 5122448. PMID 26457641.
- ↑ Toemen L., De Jonge L.L., Gishti O., et al Longitudinal growth during fetal life and infancy and cardiovascular outcomes at school-age. J. Hypertens.. 2016;34(7):1396-1406. doi:10.1097/HJH.0000000000000947
- ↑ Barker DJ, Osmond C, Forsen TJ, Kajantie E, Eriksson JG. Trajectoriesof growth among children who have coronary events as adults.N Engl JMed2005; 353:1802–1809.
- ↑ Curhan GC, Willett WC, Rimm EB, Spiegelman D, Ascherio AL, Stamp-fer MJ. Birth weight and adult hypertension, diabetes mellitus, andobesity in US men.Circulation1996; 94:3246–3250
- ↑ Osmond C, Barker DJ, Winter PD, Fall CH, Simmonds SJ. Early growthand death from cardiovascular disease in women.BMJ1993; 307:1519–1524.
- 1 2 3 "Global nutrition targets 2025: low birth weight policy brief". www.who.int. Archived from the original on 2021-10-26. Retrieved 2020-11-04.
- ↑ "UNSD — Methodology: Standard country or area codes for statistical use (M49)". unstats.un.org. Archived from the original on 2017-08-30. Retrieved 2020-11-04.
- ↑ "FastStats - Birthweight and Gestation". www.cdc.gov. 2020-08-04. Archived from the original on 2020-11-12. Retrieved 2020-11-04.
- 1 2 Kowlessar N.M., Jiang H.J., and Steiner C. Hospital Stays for Newborns, 2011. HCUP Statistical Brief #163. October 2013. Agency for Healthcare Research and Quality, Rockville, MD. Archived 2022-08-18 at the Wayback Machine