Blue nevus
| Blue nevus | |
|---|---|
| Other names: Dendritic blue nevus, common blue nevus, dermal denf=dritic melanocytotic nevus, nevus of Jadassohn, Tièche nevus, Jadassohn-Tièche nevus[1] | |
.jpg.webp) | |
| Blue nevus | |
| Specialty | Dermatology |
| Symptoms | Single well-defined blue-black bump[1] |
| Complications | Rarely malignant transformation[2] |
| Types | Dendritic, cellular[1] |
| Causes | Unclear[2] |
| Diagnostic method | Visualisation, dermoscopy[3] |
| Differential diagnosis | Dermatofibroma, melanoma[2][4] |
| Treatment | Monitoring, excision[2] |
| Prognosis | Good[2] |
| Frequency | Female>male[5] |
A blue nevus is a type of coloured mole, typically a single well-defined blue-black bump.[1]
The blue colour is caused by the pigment being deep in the skin.[3]
Diagnosis is by visualisation and dermoscopy.[3] A biopsy is sometimes performed, or the whole lesion surgically removed.[2] The outcome is generally good but there is a small chance of cancerous transformation.[2] Differential diagnosis includes dermatofibroma and melanoma.[2]
Blue nevi are more common in females than males.[5] It was first studied in 1906 by Tièche, a student of Josef Jadassohn.[6]
Classification
Blue nevi may be divided into the following types:[7]: 701
- A patch blue nevus (also known as an "acquired dermal melanocytosis", and "dermal melanocyte hamartoma") is a cutaneous condition characterized by a diffusely gray-blue area that may have superimposed darker macules.[8]
- A blue nevus of Jadassohn–Tièche (also known as a "common blue nevus", and "nevus ceruleus") is a cutaneous condition characterized by a steel-blue papule or nodule.[7]: 701
- A cellular blue nevus is a cutaneous condition characterized by large, firm, blue or blue-black nodules.[7]: 701
- An epithelioid blue nevus is a cutaneous condition most commonly seen in patients with the Carney complex.[7]: 701
- A deep penetrating nevus is a type of benign melanocytic skin tumor characterized, as its name suggests, by penetration into the deep dermis and/or subcutis. Smudged chromatic is a typical finding. In some cases mitotic figures or atypical melanocytic cytology are seen, potentially mimicking a malignant melanoma. Evaluation by an expert skin pathologist is advisable in some cases to help differentiate from invasive melanoma.[7]: 701
- An amelanotic blue nevus (also known as a "hypomelanotic blue nevus") is a cutaneous condition characterized by mild atypia and pleomorphism.[7]: 701
- A malignant blue nevus is a cutaneous condition characterized by a sheet-like growth pattern, mitoses, necrosis, and cellular atypia.[8][7]: 701
Signs and symptoms
It is typically a single well-defined blue-black bump.[5]
.jpg.webp) Blue nevus
Blue nevus.jpg.webp) Blue naevus
Blue naevus.jpg.webp) Blue naevus
Blue naevus
Diagnosis
Diagnosis is by visualisation and dermoscopy.[3] A biopsy is sometimes performed.[2]
Dermoscopy
.jpg.webp) Blue naevus
Blue naevus Blue nevus and dermoscopy
Blue nevus and dermoscopy.jpg.webp)
Histopathology
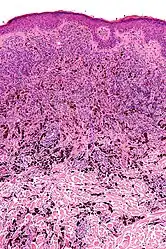 Micrograph of a blue nevus showing the characteristic pigmented melanocytes between bundles of collagen. H&E stain.
Micrograph of a blue nevus showing the characteristic pigmented melanocytes between bundles of collagen. H&E stain.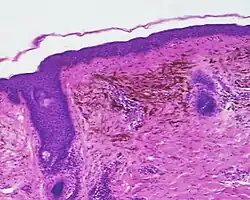 Blue nevus
Blue nevus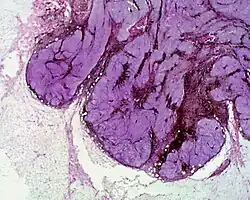 Cellular blue nevus
Cellular blue nevus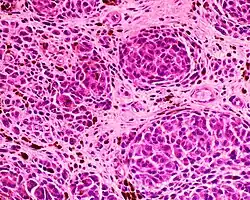 Epithelioid blue nevus
Epithelioid blue nevus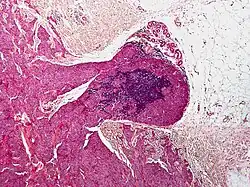 Malignant blue nevus
Malignant blue nevus
Epidemiology

Blue nevi are more common in females than males.[5]
History
It was first studied in 1906 by Tièche, a student of Josef Jadassohn.[6]
See also
References
- 1 2 3 4 DE, Elder; D, Massi; RA, Scolyer; R, Willemze (2018). "2. Melanocytic tumours: Blue nevus and cellular blue naevus". WHO Classification of Skin Tumours. Vol. 11 (4th ed.). Lyon (France): World Health Organization. pp. 126–129. ISBN 978-92-832-2440-2. Archived from the original on 2022-07-11. Retrieved 2022-08-20.
- 1 2 3 4 5 6 7 8 9 Austad, Steve S.; Athalye, Leela (2021). "Blue Nevus". StatPearls. StatPearls Publishing. Archived from the original on 2021-10-13. Retrieved 2021-10-12.
- 1 2 3 4 "Blue naevus". dermnetnz.org. Archived from the original on 13 August 2021. Retrieved 12 October 2021.
- ↑ Blue+Nevi at the US National Library of Medicine Medical Subject Headings (MeSH)
- 1 2 3 4 Johnstone, Ronald B. (2017). "32. Lentigines and melanomas". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. p. 545. ISBN 978-0-7020-6830-0. Archived from the original on 2021-05-25. Retrieved 2021-09-25.
- 1 2 Sreeremya, S. (17 April 2018). "Blue Nevus". International Journal of Molecular Biotechnology. 4 (1): 1–4. doi:10.37628/ijmb.v4i1.255. Archived from the original on 13 October 2021. Retrieved 12 October 2021.
- 1 2 3 4 5 6 7 James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- 1 2 Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. p. 1722. ISBN 978-1-4160-2999-1.
External links
| Classification |
|---|