Superficial spreading melanoma
| Superficial spreading melanoma | |
|---|---|
| Other names: Superficially spreading melanoma[1] | |
.jpg.webp) | |
| Superficial spreading melanoma, Breslow 0.4 mm, nonpolarised dermoscopy view | |
| Specialty | Dermatology |
| Symptoms | Irregularly edged dark spot[2] |
| Causes | Sun exposure[2] |
| Frequency | Two-thirds of cases in light skin, less common in dark skin[2] |
Superficial spreading melanoma (SSM) is a type of skin cancer that typically starts as an irregularly edged dark spot typically on sun-exposed part of the body.[2][3] The colour may be variable with dark, light and reddish shades; occasionally no color at all.[2] It typically grows in diameter before spreading to deeper tissue, forming a bump or becoming an ulcer.[2] Itching, bleeding and crust formation may occur in some.[2] The backs and shoulders of males and legs of women are particularly prone.[2]
It is a type of melanocytic tumor occurring in intermittently sun-exposed skin.[2] The cause is associated with repeated sunburns in childhood, intermittent exposure to sun during life, and sun bed use.[2]
Two-thirds of cases occur in light skin, and it less common in dark skin.[2]
Signs and symptoms
Often, this disease evolves from a precursor lesion, usually a dysplastic nevus. Otherwise it arises in previously normal skin. A prolonged radial growth phase, where the lesion remains thin, may eventually be followed by a vertical growth phase where the lesion becomes thick and nodular. As the risk of spread varies with the thickness, early SSM is more frequently cured than late nodular melanoma. The average age at diagnosis is in the fifth decade, and it tends to occur on sun-exposed skin, especially on the backs of males and lower limbs of females.
.jpg.webp) Superficial spreading melanoma, Breslow 0.7mm, arising within a melanoma in situ, nonpolarised dermoscopy view
Superficial spreading melanoma, Breslow 0.7mm, arising within a melanoma in situ, nonpolarised dermoscopy view.jpg.webp) Superficial spreading melanoma, Breslow 0.25 mm, polarised dermoscopy view
Superficial spreading melanoma, Breslow 0.25 mm, polarised dermoscopy view.jpg.webp) Superficial spreading melanoma, Breslow 0.5 mm, nonpolarised dermoscopy view
Superficial spreading melanoma, Breslow 0.5 mm, nonpolarised dermoscopy view
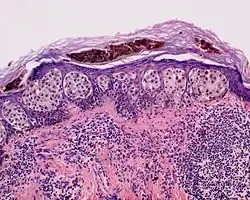
Histopathology
The microscopic hallmarks are:
- Large melanocytic cells with nest formation along the dermo-epidermal junction.
- Invasion of the upper epidermis in a pagetoid fashion (discohesive single cell growth).
- The pattern of rete ridges is often effaced.
- Invasion of the dermis by atypical, pleomorphic melanocytes
- Absence of the 'maturation' typical of naevus cells
- Mitoses
Treatment
Treatment is by excisional biopsy, wide local excision and possibly sentinel node biopsy. Spread of disease to local lymph nodes or distant sites (typically brain, bone, skin and lung) marks a decidedly poor prognosis.
Epidemiology
Two-thirds of cases occur in light skin, and it less common in dark skin.[2]
See also
References
- ↑ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- 1 2 3 4 5 6 7 8 9 10 11 12 DE, Elder; D, Massi; RA, Scolyer; R, Willemze (2018). "2. Melanocytic tumours". WHO Classification of Skin Tumours. Vol. 11 (4th ed.). Lyon (France): World Health Organization. pp. 76–77. ISBN 978-92-832-2440-2. Archived from the original on 2022-07-11. Retrieved 2023-07-01.
- ↑ "Superficial spreading melanoma | DermNet". dermnetnz.org. Archived from the original on 1 July 2023. Retrieved 29 June 2023.
External links
| Classification |
|---|