Morning sickness
| Morning sickness | |
|---|---|
| Other names: Nausea and vomiting of pregnancy, nausea gravidarum, emesis gravidarum, pregnancy sickness | |
| Specialty | Obstetrics |
| Symptoms | Nausea, vomiting[1] |
| Complications | Wernicke encephalopathy, esophageal rupture[1] |
| Usual onset | 4th week of pregnancy[2] |
| Duration | Until 16th week of pregnancy[2] |
| Causes | Unknown[2] |
| Diagnostic method | Based on symptoms after other causes have been ruled out[3] |
| Differential diagnosis | Hyperemesis gravidarum[1] |
| Prevention | Prenatal vitamins[3] |
| Treatment | Doxylamine and pyridoxine[3][4] |
| Frequency | ~75% of pregnancies[4][5] |
Morning sickness, also called nausea and vomiting of pregnancy (NVP), is a symptom of pregnancy that involves nausea or vomiting.[1] Despite the name, nausea or vomiting can occur at any time during the day.[2] Typically the symptoms occur between the 4th and 16th week of pregnancy.[2] About 10% of women still have symptoms after the 20th week of pregnancy.[2] A severe form of the condition is known as hyperemesis gravidarum and results in weight loss.[1][6]
The cause of morning sickness is unknown but may relate to changing levels of the hormone human chorionic gonadotrophin.[2] Some have proposed that morning sickness may be useful from an evolutionary point of view.[1] Diagnosis should only occur after other possible causes have been ruled out.[3] Abdominal pain, fever, or headaches are typically not present in morning sickness.[1]
Taking prenatal vitamins before pregnancy may decrease the risk.[3] Specific treatment other than a bland diet may not be required for mild cases.[2][6][3] If treatment is used the combination of doxylamine and pyridoxine is recommended initially.[3][4] There is limited evidence that ginger may be useful.[3][7][8] For severe cases that have not improved with other measures methylprednisolone may be tried.[3] Tube feeding may be required in women who are losing weight.[3]
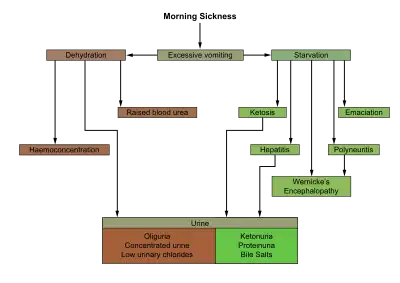
Morning sickness affects about 70–80% of all pregnant women to some extent.[4][5] About 60% of women experience vomiting.[2] Hyperemesis gravidarum occurs in about 1.6% of pregnancies.[1] Morning sickness can negatively affect quality of life, result in decreased ability to work while pregnant, and result in health-care expenses.[3] Generally, mild to moderate cases have no effect on the baby.[1] Most severe cases also have normal outcomes.[1] Some women choose to have an abortion due to the severity of symptoms.[1] Complications such as Wernicke encephalopathy or esophageal rupture may occur, but very rarely.[1]
Signs and symptoms
About 66% of women have both nausea and vomiting while 33% have just nausea.[1]
Cause
The cause of morning sickness is unknown but may relate to changing levels of the hormone human chorionic gonadotrophin.[2] Some have proposed that morning sickness may be useful from an evolutionary point of view, arguing that morning sickness may protect both the pregnant woman and the developing embryo just when the fetus is most vulnerable.[1] Diagnosis should only occur after other possible causes have been ruled out.[3] Abdominal pain, fever, or headaches are typically not present in morning sickness.[1]
Nausea and vomiting may also occur with molar pregnancy.[9]
Morning sickness is related to diets low in cereals and high in sugars, oilcrops, alcohol and meat.[10]
Pathophysiology
Hormone changes
- An increase in the circulating level of the hormone estrogen.[11] However, there is no consistent evidence of differences in estrogen levels and levels of bilirubin between women that experience sickness and those that do not.[12] Related to increased estrogen levels, a similar form of nausea is also seen in some women who use hormonal contraception or hormone replacement therapy.
- An increase in progesterone relaxes the muscles in the uterus, which prevents early childbirth, but may also relax the stomach and intestines, leading to excess stomach acids and gastroesophageal reflux disease (GERD).
- An increase in human chorionic gonadotropin. It is probably not the HCG itself that causes the nausea. More likely, it is the HCG stimulating the maternal ovaries to secrete estrogen, which in turn causes the nausea.[13]
Defense mechanism
Morning sickness may be an evolved trait that protects the baby against toxins ingested by the mother. Evidence in support of this theory includes:[14][15]
- Morning sickness is very common among pregnant women, which argues in favor of its being a functional adaptation and against the idea that it is a pathology.
- Fetal vulnerability to toxins peaks at around 3 months, which is also the time of peak susceptibility to morning sickness.
- There is a good correlation between toxin concentrations in foods, and the tastes and odors that cause revulsion.
Women who have no morning sickness are more likely to miscarry.[16] This may be because such women are more likely to ingest substances that are harmful to the fetus.[17]
In addition to protecting the fetus, morning sickness may also protect the mother. A pregnant woman's immune system is suppressed during pregnancy, presumably to reduce the chances of rejecting tissues of her own offspring.[18] Because of this, animal products containing parasites and harmful bacteria can be especially dangerous to pregnant women. There is evidence that morning sickness is often triggered by animal products including meat and fish.[19]
If morning sickness is a defense mechanism against the ingestion of toxins, the prescribing of anti-nausea medication to pregnant women may have the undesired side effect of causing birth defects or miscarriages by encouraging harmful dietary choices.[14]
Treatments
There is a lack of good evidence to support the use of any particular intervention for morning sickness.[20]
Medications
A number of antiemetics are effective and safe in pregnancy including: pyridoxine/doxylamine, antihistamines (such as diphenhydramine), metoclopramide, and phenothiazines (such as promethazine).[21][22] With respect to effectiveness it is unknown if one is superior to another.[21] In the United States and Canada, the doxylamine-pyridoxine combination (as Diclegis in US and Diclectin in Canada) is the only approved pregnancy category "A" prescription treatment for nausea and vomiting of pregnancy.[22]
Ondansetron may be beneficial, but there are some concerns regarding an association with cleft palate,[23] and there is little high quality data.[21] Metoclopramide is also used and relatively well tolerated.[24] Evidence for the use of corticosteroids is weak.[25]
Alternative medicine
Some studies support the use of ginger, but overall the evidence is limited and inconsistent.[3][7][20][26] Safety concerns have been raised regarding its anticoagulant properties.[27][28]
History
Thalidomide
Thalidomide was originally developed and prescribed as a cure for morning sickness in West Germany, but its use was discontinued when it was found to cause birth defects.[29] The United States Food and Drug Administration never approved thalidomide for use as a cure for morning sickness.[30]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 "Practice Bulletin No. 153: Nausea and Vomiting of Pregnancy". Obstetrics and Gynecology. 126 (3): e12–24. September 2015. doi:10.1097/AOG.0000000000001048. PMID 26287788.
- 1 2 3 4 5 6 7 8 9 10 Festin, M (3 June 2009). "Nausea and vomiting in early pregnancy". BMJ Clinical Evidence. 2009. PMC 2907767. PMID 21726485.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 "Practice Bulletin Summary No. 153: Nausea and Vomiting of Pregnancy". Obstetrics and Gynecology. 126 (3): 687–8. September 2015. doi:10.1097/01.aog.0000471177.80067.19. PMID 26287781.
- 1 2 3 4 Koren, G (December 2014). "Treating morning sickness in the United States--changes in prescribing are needed". American Journal of Obstetrics and Gynecology. 211 (6): 602–6. doi:10.1016/j.ajog.2014.08.017. PMID 25151184.
- 1 2 Einarson, Thomas R.; Piwko, Charles; Koren, Gideon (2013-01-01). "Prevalence of nausea and vomiting of pregnancy in the USA: a meta analysis". Journal of Population Therapeutics and Clinical Pharmacology. 20 (2): e163–170. ISSN 1710-6222. PMID 23863545.
- 1 2 "Pregnancy". Office on Women's Health. September 27, 2010. Archived from the original on 10 December 2015. Retrieved 5 December 2015.
- 1 2 Matthews, A; Haas, DM; O'Mathúna, DP; Dowswell, T (8 September 2015). "Interventions for nausea and vomiting in early pregnancy". The Cochrane Database of Systematic Reviews (9): CD007575. doi:10.1002/14651858.CD007575.pub4. PMC 4004939. PMID 26348534.

- ↑ Moe, Samantha (4 January 2016). "#153 Ginger for Nausea and Vomiting of Pregnancy: A queasy question". CFPCLearn. Archived from the original on 25 March 2023. Retrieved 16 June 2023.
- ↑ Verberg, MF; Gillott, DJ; Al-Fardan, N; Grudzinskas, JG (2005). "Hyperemesis gravidarum, a literature review". Human Reproduction Update. 11 (5): 527–39. doi:10.1093/humupd/dmi021. PMID 16006438.
- ↑ Pepper, GV; Craig Roberts, S (2006). "Rates of nausea and vomiting in pregnancy and dietary characteristics across populations". Proceedings of the Royal Society B. 273 (1601): 2675–2679. doi:10.1098/rspb.2006.3633. PMC 1635459. PMID 17002954.
- ↑ Lagiou, P; Tamimi, R; Mucci, LA; Trichopoulos, D; Adami, HO; Hsieh, CC (April 2003). "Nausea and vomiting in pregnancy in relation to prolactin, estrogens, and progesterone: a prospective study". Obstetrics and Gynecology. 101 (4): 639–44. doi:10.1016/s0029-7844(02)02730-8. PMID 12681864.
{{cite journal}}: CS1 maint: url-status (link) - ↑ Elizabeth Bauchner; Wendy Marquez. "Morning Sickness: Coping With The Worst". NY Metro Parents Magazine. Archived from the original on 2008-12-04. Retrieved 2008-07-06.
- ↑ Niebyl, Jennifer R. (2010). "Nausea and Vomiting in Pregnancy". New England Journal of Medicine. 363 (16): 1544–1550. doi:10.1056/NEJMcp1003896. PMID 20942670.
- 1 2 Nesse, Randolphe M; Williams, George C (1996). Why We Get Sick (1st ed.). New York: Vintage Books. p. 290.
- ↑ Pepper GV, Craig Roberts S (October 2006). "Rates of nausea and vomiting in pregnancy and dietary characteristics across populations". Proceedings of the Royal Society B. 273 (1601): 2675–2679. doi:10.1098/rspb.2006.3633. PMC 1635459. PMID 17002954.
- ↑ Chan, Ronna L.; Olshan, A. F.; Savitz, D. A.; Herring, A. H.; Daniels, J. L.; Peterson, H. B.; Martin, S. L.; et al. (Sep 22, 2010). "Severity and duration of nausea and vomiting symptoms in pregnancy and spontaneous abortion". Human Reproduction. 25 (11): 2907–12. doi:10.1093/humrep/deq260. PMC 3140259. PMID 20861299. Archived from the original on 2011-12-13.
- ↑ Sherman, Paul W.; Flaxman, Samuel M. (2002). "Nausea and vomiting of pregnancy in an evolutionary perspective". Am J Obstet Gynecol. 186 (5): S190–S197. CiteSeerX 10.1.1.611.7889. doi:10.1067/mob.2002.122593. PMID 12011885.
- ↑ Haig, David (October 1993). "Genetic conflicts in human pregnancy". Quarterly Review of Biology. 68 (4): 495–532. doi:10.1086/418300. PMID 8115596. Archived from the original on 2021-08-28. Retrieved 2018-09-18.
- ↑ Flaxman, Samuel M.; Sherman, Paul W. (June 2000). "Morning sickness: a mechanism for protecting mother and embryo". Quarterly Review of Biology. 75 (2): 113–148. doi:10.1086/393377. PMID 10858967.
- 1 2 Matthews, A; Haas, DM; O'Mathúna, DP; Dowswell, T (8 September 2015). "Interventions for nausea and vomiting in early pregnancy". The Cochrane Database of Systematic Reviews (9): CD007575. doi:10.1002/14651858.CD007575.pub4. PMC 4004939. PMID 26348534.
- 1 2 3 Jarvis, S; Nelson-Piercy, C (Jun 17, 2011). "Management of nausea and vomiting in pregnancy". BMJ (Clinical Research Ed.). 342: d3606. doi:10.1136/bmj.d3606. PMID 21685438. Archived from the original on August 28, 2021. Retrieved September 18, 2018.
- 1 2 Clark SM, Dutta E, Hankins GD (September 2014). "The outpatient management and special considerations of nausea and vomiting in pregnancy". Semin Perinatol. 38 (14): 496–502. doi:10.1053/j.semperi.2014.08.014. PMID 25267280.
- ↑ Koren, G (October 2012). "Motherisk update. Is ondansetron safe for use during pregnancy?". Canadian Family Physician. 58 (10): 1092–3. PMC 3470505. PMID 23064917.
- ↑ Tan, PC; Omar, SZ (April 2011). "Contemporary approaches to hyperemesis during pregnancy". Current Opinion in Obstetrics and Gynecology. 23 (2): 87–93. doi:10.1097/GCO.0b013e328342d208. PMID 21297474.
- ↑ Poon, SL (October 2011). "Towards evidence-based emergency medicine: Best BETs from the Manchester Royal Infirmary. BET 2: Steroid therapy in the treatment of intractable hyperemesis gravidarum". Emergency Medicine Journal. 28 (10): 898–900. doi:10.1136/emermed-2011-200636. PMID 21918097.
- ↑ Thomson, M.; Corbin, R.; Leung, L. (2014). "Effects of Ginger for Nausea and Vomiting in Early Pregnancy: A Meta-Analysis". The Journal of the American Board of Family Medicine. 27 (1): 115–122. doi:10.3122/jabfm.2014.01.130167. ISSN 1557-2625. PMID 24390893.
- ↑ Borrelli F, Capasso R, Aviello G, Pittler MH, Izzo AA (2005). "Effectiveness and safety of ginger in the treatment of pregnancy-induced nausea and vomiting". Obstetrics and Gynecology. 105 (4): 849–56. doi:10.1097/01.AOG.0000154890.47642.23. PMID 15802416.
- ↑ Tiran, Denise (Feb 2012). "Ginger to reduce nausea and vomiting during pregnancy: Evidence of effectiveness is not the same as proof of safety". Complementary Therapies in Clinical Practice. 18 (1): 22–25. doi:10.1016/j.ctcp.2011.08.007. ISSN 1744-3881. PMID 22196569.
- ↑ Cohen, Wayne R., ed. (2000). Cherry and Merkatz's complications of pregnancy (5th ed.). Lippincott Williams & Wilkins. p. 124. ISBN 9780683016734.
- ↑ Bren L (2001-02-28). "Frances Oldham Kelsey: FDA Medical Reviewer Leaves Her Mark on History". FDA Consumer. U.S. Food and Drug Administration. Archived from the original on 2011-06-29. Retrieved 2009-12-23.
External links
| Classification | |
|---|---|
| External resources |