Proteinuria
| Proteinuria | |
|---|---|
| Other names: Protein in the urine | |
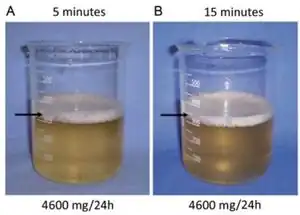 | |
| Foamy and cloudy urine due to high protein including albumin[1] | |
| Pronunciation |
|
| Specialty | Nephrology |
| Symptoms | Foamy urine, leg swelling[2] |
| Complications | Heart disease, blood clots, muscle loss[2] |
| Types | Transient, persistent[2] |
| Causes | Transient: Urinary tract infections, fever, exercise, pregnancy, prolonged standing[2] Persistent: Glomerulonephritis, certain medications, diabetes, heart failure, high blood pressure, myeloma[2] |
| Diagnostic method | Urine protein creatinine ratio (UPCR) > 45 to 50 mg/mmol[2] |
| Differential diagnosis | Dehydrated[2] |
| Treatment | Depends on the underlying cause[2] |
| Medication | ACE inhibitors, ARBs[2] |
| Frequency | Relatively common (adults)[3][2] |
Proteinuria is the presence of excess proteins in the urine.[2] This can result in the urine being foamy.[2] Complications can include leg swelling, heart disease, blood clots, and muscle loss.[2] It can be divided into transient and persistent.[2]
Transient causes include urinary tract infections, fever, exercise, pregnancy, and being on ones feet for a prolonged period of time.[2] Ongoing protein loss in the urine is a sign of kidney damage; with the amount of protein loss linked to the severity of disease.[2] This may include glomerulonephritis, certain medications, diabetes, heart failure, high blood pressure, and myeloma.[2]
Normally urine contains less than 15 mg/mmol or 150 mg/24 hr of protein.[2][4] Proteinuria is defined as a urine protein creatinine ratio (UPCR) of more than 45 to 50 mg/mmol (400 mg/g to 440 mg/g) or a urine albumin creatinine ratio (UACR) of greater than 30 mg/mmol.[2] Further investigation; however, is not generally required unless blood is present or the UPCR is greater than 100 mg/mmol.[2] Severe proteinurina (>350 mg/mmol or 3.5 g/24 hr) is defined as nephrotic syndrome.[2] The test may be falsely positive in those who are dehydrated.[2]
Proteinuria is relatively common in adults, occurring in about 20% of people.[2][3] Of those with a positive urine dipstick, less than 2% have a serious cause.[2] In Japan, people are routine screened for the condition.[2]
Signs and symptoms
Proteinuria often doesn't cause any symptoms and it may be discovered incidentally.
Foamy urine is considered a cardinal sign of proteinuria, but only a third of people with foamy urine have proteinuria as the underlying cause.[5] It may also be caused by bilirubin in the urine (bilirubinuria),[6] retrograde ejaculation, pneumaturia (air bubbles in the urine) due to a fistula,[7] or drugs such as pyridium.[6]
Causes
There are three main mechanisms to cause proteinuria:
- Due to disease in the glomerulus
- Because of increased quantity of proteins in serum (overflow proteinuria)
- Due to low reabsorption at proximal tubule (Fanconi syndrome)
Proteinuria can also be caused by certain biological agents, such as bevacizumab (Avastin) used in cancer treatment. Excessive fluid intake (drinking in excess of 4 litres of water per day) is another cause.[8][9]
Proteinuria may be a sign of renal (kidney) damage. Since serum proteins are readily reabsorbed from urine, the presence of excess protein indicates either an insufficiency of absorption or impaired filtration. People with diabetes may have damaged nephrons and develop proteinuria. The most common cause of proteinuria is diabetes, and in any person with proteinuria and diabetes, the cause of the underlying proteinuria should be separated into two categories: diabetic proteinuria versus the field.
With severe proteinuria, general hypoproteinemia can develop which results in diminished oncotic pressure. Symptoms of diminished oncotic pressure may include ascites, edema and hydrothorax.
Conditions
Proteinuria may be a feature of the following conditions:[10]
- Dental mercury amalgam
- Nephrotic syndromes (i.e. intrinsic kidney failure)
- Pre-eclampsia
- Eclampsia
- Toxic lesions of kidneys
- Amyloidosis
- Collagen vascular diseases (e.g. systemic lupus erythematosus)
- Dehydration
- Glomerular diseases, such as membranous glomerulonephritis, focal segmental glomerulonephritis, minimal change disease (lipoid nephrosis)
- Strenuous exercise
- Stress
- Benign orthostatic (postural) proteinuria
- Focal segmental glomerulosclerosis (FSGS)
- IgA nephropathy (i.e. Berger's disease)
- IgM nephropathy
- Membranoproliferative glomerulonephritis
- Membranous nephropathy
- Minimal change disease
- Sarcoidosis
- Alport syndrome
- Diabetes mellitus (diabetic nephropathy)
- Drugs (e.g. NSAIDs, nicotine, penicillamine, lithium carbonate, gold and other heavy metals, ACE inhibitors, antibiotics, or opiates (especially heroin)[11]
- Fabry disease
- Infections (e.g. HIV, syphilis, hepatitis, poststreptococcal infection, urinary schistosomiasis)
- Aminoaciduria
- Fanconi syndrome in association with Wilson disease
- Hypertensive nephrosclerosis
- Interstitial nephritis
- Sickle cell disease
- Hemoglobinuria
- Multiple myeloma
- Myoglobinuria
- Organ rejection:[12]
- Ebola virus disease
- Nail–patella syndrome
- Familial Mediterranean fever
- HELLP syndrome
- Systemic lupus erythematosus
- Granulomatosis with polyangiitis
- Rheumatoid arthritis
- Glycogen storage disease type 1[13]
- Goodpasture syndrome
- Henoch–Schönlein purpura
- A urinary tract infection which has spread to the kidney(s)
- Sjögren syndrome
- Post-infectious glomerulonephritis
- Living kidney donor[14]
- Polycystic kidney disease[15]
Bence–Jones proteinuria
- Amyloidosis
- Pre-malignant plasma cell dyscrasias:
- Malignant plasma cell dyscrasias
- Other malignancies
- Chronic lymphocytic leukemia
- Rare cases of other Lymphoid leukemias
- Rare cases of Lymphomas
Pathophysiology
Protein is the building block of all living organisms.[16] When kidneys are functioning properly by filtering the blood, they distinguish the proteins from the wastes which were previously present together in the blood.[16] Thereafter, kidneys retain or reabsorb the filtered proteins and return them to the circulating blood while removing wastes by excreting them in the urine.[16] Whenever the kidney is compromised, their ability to filter the blood by differentiating protein from the waste, or retaining the filtered protein then returning which back to the body, is damaged.[16] As a result, there is a significant amount of protein to be discharged along with waste in the urine that makes the concentration of proteins in urine high enough to be detected by medical machine.[16]
Medical testing equipment has improved over time, and as a result tests are better able to detect smaller quantities of protein.[16] Protein in urine is considered normal as long as the value remains within the normal reference range.[16] Variation exists between healthy patients, and it is generally considered harmless for the kidney to fail to retain a few proteins in the blood, letting those protein discharge from the body through urine.[16]
Albumin and immunoglobins
Albumin is a protein produced by the liver which makes up roughly 50%-60% of the proteins in the blood while the other 40%-50% are proteins other than albumin, such as immunoglobins.[17][16] This is why the concentration of albumin in the urine is one of the single sensitive indicators of kidney disease, particularly for those with diabetes or hypertension, compared to routine proteinuria examination.[16]
As the loss of proteins from the body progresses, the suffering will gradually become symptomatic.[16]
The exception applies to the scenario when there's an overproduction of proteins in the body, in which the kidney is not to blame.[16]
Diagnosis
| Protein dipstick grading | ||
|---|---|---|
| Designation | Approx. amount | |
| Concentration[18] | Daily[19] | |
| Trace | 5–20 mg/dL | |
| 1+ | 30 mg/dL | Less than 0.5 g/day |
| 2+ | 100 mg/dL | 0.5–1 g/day |
| 3+ | 300 mg/dL | 1–2 g/day |
| 4+ | More than 1000 mg/dL | More than 2 g/day |
Conventionally, proteinuria is diagnosed by a simple dipstick test, although it is possible for the test to give a false negative reading,[20] even with nephrotic range proteinuria if the urine is dilute. False negatives may also occur if the protein in the urine is composed mainly of globulins or Bence Jones proteins because the reagent on the test strips, bromophenol blue, is highly specific for albumin.[10][21] Traditionally, dipstick protein tests would be quantified by measuring the total quantity of protein in a 24-hour urine collection test, and abnormal globulins by specific requests for protein electrophoresis.[6][22] Trace results may be produced in response to excretion of Tamm–Horsfall mucoprotein.
More recently developed technology detects human serum albumin (HSA) through the use of liquid crystals (LCs). The presence of HSA molecules disrupts the LCs supported on the AHSA-decorated slides thereby producing bright optical signals which are easily distinguishable. Using this assay, concentrations of HSA as low as 15 µg/mL can be detected.[23]
Alternatively, the concentration of protein in the urine may be compared to the creatinine level in a spot urine sample. This is termed the protein/creatinine ratio. The 2005 UK Chronic Kidney Disease guidelines state that protein/creatinine ratio is a better test than 24-hour urinary protein measurement. Proteinuria is defined as a protein/creatinine ratio greater than 45 mg/mmol (which is equivalent to albumin/creatinine ratio of greater than 30 mg/mmol or approximately 300 mg/g) with very high levels of proteinuria having a ratio greater than 100 mg/mmol.[24]
Protein dipstick measurements should not be confused with the amount of protein detected on a test for microalbuminuria which denotes values for protein for urine in mg/day versus urine protein dipstick values which denote values for protein in mg/dL. That is, there is a basal level of proteinuria that can occur below 30 mg/day which is considered non-pathology. Values between 30–300 mg/day are termed microalbuminuria which is considered pathologic.[25] Urine protein lab values for microalbumin of >30 mg/day correspond to a detection level within the "trace" to "1+" range of a urine dipstick protein assay. Therefore, positive indication of any protein detected on a urine dipstick assay obviates any need to perform a urine microalbumin test as the upper limit for microalbuminuria has already been exceeded.[26]
Analysis
It is possible to analyze urine samples in determining albumin, hemoglobin and myoglobin with an optimized MEKC method.[27]
Treatment
Treating proteinuria mainly needs proper diagnosis of the cause. The most common cause is diabetic nephropathy; in this case, proper glycemic control may slow the progression. Medical management consists of angiotensin converting enzyme (ACE) inhibitors, which are typically first-line therapy for proteinuria. In patients whose proteinuria is not controlled with ACE inhibitors, the addition of an aldosterone antagonist (i.e., spironolactone)[28] or angiotensin receptor blocker (ARB)[29] may further reduce protein loss. Caution must be used if these agents are added to ACE inhibitor therapy due to the risk of hyperkalemia. Proteinuria secondary to autoimmune disease should be treated with steroids or steroid-sparing agent plus the use of ACE inhibitors.
See also
References
- ↑ Dantas, M; Barros Silva, GE; Moysés-Neto, M (June 2013). "Foamy urine in nephrotic syndrome". Clinical kidney journal. 6 (3): 341. doi:10.1093/ckj/sft018. PMID 26064498.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 Haider, MZ; Aslam, A (January 2021). "Proteinuria". PMID 33232060.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 Carroll, MF; Temte, JL (2000-09-15). "Proteinuria in adults: a diagnostic approach". American family physician. 62 (6): 1333–40. PMID 11011862.
- ↑ "Urine protein : creatinine ratio - Primary Care Notebook". primarycarenotebook.com. Archived from the original on 1 July 2023. Retrieved 13 June 2023.
- ↑ Khitan, Zeid J.; Glassock, Richard J. (1 October 2019). "Foamy Urine: Is This a Sign of Kidney Disease?". Clinical Journal of the American Society of Nephrology. 14 (11): 1664–1666. doi:10.2215/CJN.06840619. PMC 6832055. PMID 31575619.
- 1 2 3 URINALYSIS Archived 2006-08-16 at the Wayback Machine Ed Friedlander, M.D., Pathologist – Retrieved 2007-01-20
- ↑ "Pneumaturia". GPnotebook. Retrieved 2007-01-20
- ↑ Clark WF, Kortas C, Suri RS, Moist LM, Salvadori M, Weir MA, Garg AX (2008). "Excessive fluid intake as a novel cause of proteinuria". Canadian Medical Association Journal. 178 (2): 173–175. doi:10.1503/cmaj.070792. PMC 2175005. PMID 18195291.
- ↑ "Drinking too much water called latest threat to health". Montreal Gazette. January 2008. Archived from the original on 2012-02-14.
- 1 2 Simerville JA, Maxted WC, Pahira JJ (2005). "Urinalysis: a comprehensive review". American Family Physician. 71 (6): 1153–62. PMID 15791892. Archived from the original on 2005-06-02.
- ↑ Dettmeyer RB, Preuss J, Wollersen H, Madea B (2005). "Heroin-associated nephropathy". Expert Opinion on Drug Safety. 4 (1): 19–28. doi:10.1517/14740338.4.1.19. PMID 15709895.
- ↑ Naesens (2015). "Proteinuria as a Noninvasive Marker for Renal Allograft Histology and Failure: An Observational Cohort Study". J Am Soc Nephrol. 27 (1): 281–92. doi:10.1681/ASN.2015010062. PMC 4696583. PMID 26152270.
- ↑ Chou JY, Matern D, Mansfield BC, Chen YT (2002). "Type 1 Glycogen Storage Diseases: Disorders of the Glucose-6-Phosphatase Complex". Current Molecular Medicine. 2 (2): 121–143. doi:10.2174/1566524024605798. PMID 11949931.
- ↑ Fernando, B.S. (June 14, 2008). "A Doctor's Perspective". BMJ. 336 (7657): 1374–6. doi:10.1136/bmj.a277. PMC 2427141. PMID 18556321.
- ↑ Chapman, A.B.; Johnson, A.M.; Gabow, P.A.; Schrier, R.W. (December 1, 1994). "Overt proteinuria and microalbuminuria in autosomal dominant polycystic kidney disease". Journal of the American Society of Nephrology. 5: 1349–1354. Archived from the original on May 15, 2018.
- 1 2 3 4 5 6 7 8 9 10 11 12 "Urine Protein". Lab Tests Online. Archived from the original on 2019-04-14. Retrieved 2019-05-21.
- ↑ "Globulin". Lab Tests Online. Archived from the original on 2020-06-02. Retrieved 2019-05-22.
- ↑ eMedicine > Proteinuria Archived 2010-07-29 at the Wayback Machine Author: Ronald J Kallen. Coauthor: Watson C Arnold. Updated: Apr 21, 2008
- ↑ Ivanyi B, Kemeny E, Szederkenyi E, Marofka F, Szenohradszky P (December 2001). "The value of electron microscopy in the diagnosis of chronic renal allograft rejection". Mod. Pathol. 14 (12): 1200–8. doi:10.1038/modpathol.3880461. PMID 11743041.
- ↑ Simerville JA, Maxted WC, and Pahira JJ. Urinalysis: A Comprehensive Review Archived 2012-02-05 at the Wayback Machine Am Fam Physician. 2005 Mar 15;71(6):1153–1162. Accessed 2 Feb 2012.
- ↑ "Archived copy". Archived from the original on 2006-08-10. Retrieved 2006-08-06.
{{cite web}}: CS1 maint: archived copy as title (link) Retrieved 2007-01-20 - ↑ "Archived copy". Archived from the original on 2007-02-12. Retrieved 2006-08-06.
{{cite web}}: CS1 maint: archived copy as title (link) Retrieved 2007-01-20 - ↑ Aliño VJ, Yang KL (2011). "Using liquid crystals as a readout system in urinary albumin assays". Analyst. 136 (16): 3307–13. doi:10.1039/c1an15143f. PMID 21709868. Archived from the original on 2021-04-17. Retrieved 2019-12-17.
- ↑ "Identification, management and referral of adults with chronic kidney disease: concise guidelines" (PDF). UK Renal Association. 2005-09-27. Archived from the original (PDF) on 2013-02-19. – see Guideline 4 Confirmation of proteinuria, on page 9
- ↑ Meyer NL, Mercer BM, Friedman SA, Sibai BM (Jan 1994). "Urinary dipstick protein: a poor predictor of absent or severe proteinuria". Am J Obstet Gynecol. 170 (1 Pt 1): 137–41. doi:10.1016/s0002-9378(94)70398-1. PMID 8296815.
- ↑ "The Urine Dipstick" (PDF). Georgia Regents University. Archived from the original (PDF) on 2013-06-16.
- ↑ Kočevar Glavač N, Injac R, Kreft S (2009). "Optimization and Validation of a Capillary MEKC Method for Determination of Proteins in Urine". Chromatographia. 70 (9–10): 1473–1478. doi:10.1365/s10337-009-1317-3.
- ↑ Mehdi UF, Adams-Huet B, Raskin P, Vega GL, Toto RD (2009). "Addition of angiotensin receptor blockade or mineralocorticoid antagonism to maximum angiotensin-converting enzyme inhibition in diabetic nephropathy". J Am Soc Nephrol. 20 (12): 2641–50. doi:10.1681/ASN.2009070737. PMC 2794224. PMID 19926893.
- ↑ Burgess E, Muirhead N, Rene de Cotret P, Chiu A, Pichette V, Tobe S (2009). "Supramaximal dose of candesartan in proteinuric renal disease". J Am Soc Nephrol. 20 (4): 893–900. doi:10.1681/ASN.2008040416. PMC 2663827. PMID 19211712.
External links
| Classification | |
|---|---|
| External resources |