Azoospermia
| Azoospermia | |
|---|---|
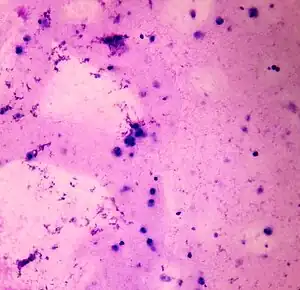 | |
| Semen analysis revealing no sperm cells and multiple white blood cells | |
| Types | Obstructive, non-obstructive[1] |
| Frequency | 1% of men of reproductive age, up to 10% of men with infertility[1] |
Azoospermia is the abscence of sperm in the semen of a man's ejaculate.[1]
It can be generally categorised as non-obstructive, where there is a problem with sperm production as may arise in the testis or the hypothalamus-pituitary-gonadal axis, or obstructive, where there is usually normal sperm production but it can't get into the semen because of a blockage in the reproductive tract such as the epididymis, vas deferens, or ejaculatory duct.[1] It is the intended result of a successful vasectomy.[2]
Globally, it affects around 1% of men of reproductive age, and up to 10% of men with infertility.[1]
Classification
Azoospermia can be classified into three major types as listed.[3] Many conditions listed may also cause various degrees of oligospermia rather than azoospermia. Pretesticular and testicular azoospermia are known as non-obstructive azoospermia, whereas post-testicular azoospermia is considered obstructive.
Pretesticular
Pretesticular azoospermia is characterized by inadequate stimulation of otherwise normal testicles and genital tract. Typically, follicle-stimulating hormone (FSH) levels are low (hypogonadotropic) commensurate with inadequate stimulation of the testes to produce sperm. Examples include hypopituitarism (for various causes), hyperprolactinemia, and exogenous FSH suppression by testosterone. Chemotherapy may suppress spermatogenesis.[4] Pretesticular azoospermia is seen in about 2% of azoospermia.[3] Pretesticular azoospermia is a kind of non-obstructive azoospermia.
Testicular
Testicular azoospermia means the testes are abnormal, atrophic, or absent, and sperm production severely disturbed to absent. FSH levels tend to be elevated (hypergonadotropic) as the feedback loop is interrupted (lack of feedback inhibition on FSH). The condition is seen in 49–93% of men with azoospermia.[3] Testicular failure includes absence of failure production and low production and maturation arrest during the process of spermatogenesis.
Causes for testicular failure include congenital issues such as in certain genetic conditions (e.g. Klinefelter syndrome), some cases of cryptorchidism or Sertoli cell-only syndrome as well as acquired conditions by infection (orchitis), surgery (trauma, cancer), radiation,[4] or other causes. Mast cells releasing inflammatory mediators appear to directly suppress sperm motility in a potentially reversible manner, and may be a common pathophysiological mechanism for many causes leading to inflammation.[5] Testicular azoospermia is a kind of non-obstructive azoospermia.
Generally, men with unexplained hypergonadotropic azoospermia need to undergo a chromosomal evaluation.
Post-testicular
In post-testicular azoospermia, sperm are produced but not ejaculated, a condition that affects 7–51% of azoospermic men.[3] The main cause is a physical obstruction (obstructive azoospermia) of the post-testicular genital tracts. The most common reason is a vasectomy done to induce contraceptive sterility.[6] Other obstructions can be congenital (for example, agenesis of the vas deferens as seen in certain cases of cystic fibrosis) or acquired, such as ejaculatory duct obstruction for instance by infection.
Ejaculatory disorders include retrograde ejaculation and anejaculation; in these conditions sperm are produced but not expelled.
Unknown
Idiopathic azoospermia is where there is no known cause of the condition. It may be a result of multiple risk factors, such as age and weight. For example, a review in 2013 came to the result that oligospermia and azoospermia are significantly associated with being overweight (odds ratio 1.1), obese (odds ratio 1.3) and morbidly obese (odds ratio 2.0), but the cause of this is unknown.[7] The review found no significant relation between oligospermia and being underweight.[7]
Genetics
Genetic factors can cause pretesticular, testicular, and post-testicular azoospermia (or oligospermia) and include the following situations:[8] The frequency of chromosomal abnormalities is inversely proportional to the semen count, thus males with azoospermia are at risk to have a 10–15% (other sources citing 15–20% incidence[9]) abnormalities on karyotyping versus about <1 % in the fertile male population.[10]
Pretesticular azoospermia may be caused by congential hypopituitarism, Kallmann syndrome, Prader-Willi syndrome and other genetic conditions that lead to GnRH or gonadotropin deficiency. Testicular azoospermia is seen in Klinefelter syndrome(XXY) and the XX male syndrome. In addition, 13% of men with azoospermia have a defective spermatogenesis that is linked to defects of the Y chromosome.[8] Such defects tend to be de novo micro-deletions and affect usually the long arm of the chromosome. A section of the long arm of the Y chromosome has been termed Azoospermia Factor (AZF) at Yq11 and subdivided into AZFa, AZFb, AZFc and possibly more subsections. Defects in this area can lead to oligospermia or azoospermia, however, a tight genotype-phenotype correlation has not been achieved.[8] Spermatogenesis is defective with gene defects for the androgen receptor.
Post-testicular azoospermia can be seen with certain point mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene commonly associated with congenital vas deferens abnormalities.
Genetic counselling is indicated for men with genetic causes of azoospermia. In terms of reproduction, it needs to be considered if the genetic defect could be transmitted to the offspring.
BRD7
BRD7, a transcription regulatory protein, is normally highly expressed in the testis. Absent or reduced expression of BRD7 protein was observed in the testes of azoospermia patients exhibiting spermatogenesis arrest.[11] Homozygous knockout mice [BRD7(-/-)] are infertile and have higher levels of apoptosis and DNA damage in their germline cells.[11]
Gene polymorphisms
The human breast cancer susceptibility gene 2 (BRCA2) is employed in DNA repair. A common single nucleotide polymorphism in BRCA2 is associated with idiopathic male infertility with azoospermia.[12]
Four genes involved in DNA double-strand break repair and chromosome synapsis (TEX11, TEX15, MLH1 and MLH3) have key roles in genomic integrity, meiotic recombination and gametogenesis. Polymorphisms in these genes were tested for associations with male infertility. Single nucleotide polymorphisms in two of these genes (TEX11 and MLH3) were found to be associated with male infertility involving azoospermy or oligospermia.[13]
Diagnosis

Azoospermia is usually detected in the course of an infertility investigation. It is established on the basis of two semen analysis evaluations done at separate occasions (when the seminal specimen after centrifugation shows no sperm under the microscope) and requires a further work-up.[14]
The investigation includes a history, a physical examination including a thorough evaluation of the scrotum and testes, laboratory tests, and possibly imaging. History includes the general health, sexual health, past fertility, libido, and sexual activity. Past exposure to a number of agents needs to be queried including medical agents like hormone/steroid therapy, antibiotics, 5-ASA inhibitors (sulfasalazine), alpha-blockers, 5 alpha-reductase inhibitors, chemotherapeutic agents, pesticides, recreational drugs (marijuana, excessive alcohol), and heat exposure of the testes. A history of surgical procedures of the genital system needs to be elicited. The family history needs to be assessed to look for genetic abnormalities.[3]
Congenital absence of the vas deferens may be detectable on physical examination and can be confirmed by a transrectal ultrasound (TRUS). If confirmed, genetic testing for cystic fibrosis is in order. Transrectal ultrasound can also assess azoospermia caused by obstruction, or anomalies related to obstruction of the ejaculatory duct, such as abnormalities within the duct itself, a median cyst of the prostate (indicating a need for cyst aspiration), or an impairment of the seminal vesicles to become enlarged or emptied.[15] Retrograde ejaculation is diagnosed by examining a post-ejaculatory urine for presence of sperm after making it alkaline and centrifuging it.[9]
Low levels of LH and FSH with low or normal testosterone levels are indicative of pretesticular problems, while high levels of gonadotropins indicate testicular problems. However, often this distinction is not clear and the differentiation between obstructive versus non-obstructive azoospermia may require a testicular biopsy.[3] On the other hand, "In azoospermic men with a normal ejaculate volume, FSH serum level greater than two times the upper limit of the normal range is reliably diagnostic of dysfunctional spermatogenesis and, when found, a diagnostic testicular biopsy is usually unnecessary, although no consensus exists in this matter."[14][16][17] Extremely high levels of FSH (>45 ID/mL) have been correlated with successful microdissection testicular sperm extraction.[18]
Serum inhibin-B weakly indicates presence of sperm cells in the testes, raising chances for successfully achieving pregnancy through testicular sperm extraction (TESE), although the association is not very substantial, having a sensitivity of 0.65 (95% confidence interval [CI]: 0.56–0.74) and a specificity of 0.83 (CI: 0.64–0.93) for prediction the presence of sperm in the testes in non-obstructive azoospermia.[19]
Seminal plasma proteins TEX101 and ECM1 were recently proposed for the differential diagnosis of azoospermia forms and subtypes, and for prediction of TESE outcome.[20][21] Mount Sinai Hospital, Canada started clinical trial to test this hypothesis in 2016.[22]
Primary hypopituitarism may be linked to a genetic cause. So a genetic evaluation may be done for men with azoospermia as a result.[10] Azoospermic men with testicular failure are advised to undergo karyotype and Y-micro-deletion testing.[23][8][14]
Treatment
Pre- and post-testicular azoospermia are frequently correctible, while testicular azoospermia is usually permanent.[10] In the former the cause of the azoospermia needs to be considered and it opens up possibilities to manage this situation directly. Thus men with azoospermia due to hyperprolactinemia may resume sperm production after treatment of hyperprolactinemia or men whose sperm production is suppressed by exogenous androgens are expected to produce sperm after cessation of androgen intake. In situations where the testes are normal but unstimulated, gonadotropin therapy can be expected to induce sperm production.
A major advancement in recent years has been the introduction of IVF with ICSI which allows successful fertilization even with immature sperm or sperm obtained directly from testicular tissue. IVF-ICSI allows for pregnancy in couples where the man has irreversible testicular azoospermia as long as it is possible to recover sperm material from the testes. Thus men with non-mosaic Klinefelter's syndrome have fathered children using IVF-ICSI.[24] Pregnancies have been achieved in situations where azoospermia was associated with cryptorchism and sperm where obtained by testicular sperm extraction (TESE).[25]
In men with post-testicular azoospermia, different approaches are available. For obstructive azoospermia, IVF-ICSI or surgery can be used and individual factors are considered for the choice of treatment.[6] Medication may be helpful for retrograde ejaculation.
Epidemiology
Globally, it affects around 1% of men of reproductive age, and up to 10% of men with infertility.[1] It may be seen in up to 20% of male infertility situations in Canada.[3]
References
- 1 2 3 4 5 6 Andrade, Danilo L.; Viana, Marina C.; Esteves, Sandro C. (January 2021). "Differential Diagnosis of Azoospermia in Men with Infertility". Journal of Clinical Medicine. 10 (14): 3144. doi:10.3390/jcm10143144. PMID 34300309.
- ↑ Barone, Mark A.; Irsula, Belinda; Chen-Mok, Mario; Sokal, David C.; the Investigator study group (2004-07-19). "Effectiveness of vasectomy using cautery". BMC Urology. 4 (1): 10. doi:10.1186/1471-2490-4-10. ISSN 1471-2490. PMC 503392. PMID 15260885. Archived from the original on 2021-12-15. Retrieved 2021-10-28.
- 1 2 3 4 5 6 7 Jarvi, K; Lo, K; Fischer, A; Grantmyre, J; Zini, A; Chow, V; Mak, V (2010). "CUA Guideline: The workup of azoospermic males". Canadian Urological Association Journal. 4 (3): 163–7. doi:10.5489/cuaj.10050. PMC 2874589. PMID 20514278.
- 1 2 Dohle, Gert R (2010). "Male infertility in cancer patients: Review of the literature". International Journal of Urology. 17 (4): 327–331. doi:10.1111/j.1442-2042.2010.02484.x. PMID 20202000.
- ↑ Menzies, F. M.; Shepherd, M. C.; Nibbs, R. J.; Nelson, S. M. (2010). "The role of mast cells and their mediators in reproduction, pregnancy and labour". Human Reproduction Update. 17 (3): 383–396. doi:10.1093/humupd/dmq053. PMID 20959350.
- 1 2 Practice Committee of ASRM, August 2008. "The management of infertility due to obstructive azzospermia" (PDF). Archived (PDF) from the original on March 4, 2016. Retrieved June 14, 2010.
- 1 2 Sermondade, N.; Faure, C.; Fezeu, L.; et al. (2012). "BMI in relation to sperm count: An updated systematic review and collaborative meta-analysis". Human Reproduction Update. 19 (3): 221–231. doi:10.1093/humupd/dms050. PMC 3621293. PMID 23242914.
- 1 2 3 4 Poongothai, J; Gopenath, TS; Manonayaki, S (2009). "Genetics of human male infertility". Singapore Medical Journal. 50 (4): 336–47. PMID 19421675.
- 1 2 Padubidri; Daftary (2011). Shaw's Textbook of Gynaecology, 15e. p. 205. ISBN 978-81-312-2548-6
- 1 2 3
- 1 2 Wang H, Zhao R, Guo C, Jiang S, Yang J, Xu Y, Liu Y, Fan L, Xiong W, Ma J, Peng S, Zeng Z, Zhou Y, Li X, Li Z, Li X, Schmitt DC, Tan M, Li G, Zhou M (2016). "Knockout of BRD7 results in impaired spermatogenesis and male infertility". Sci Rep. 6: 21776. Bibcode:2016NatSR...621776W. doi:10.1038/srep21776. PMC 4754950. PMID 26878912.
- ↑ Zhoucun A, Zhang S, Yang Y, Ma Y, Zhang W, Lin L (2006). "The common variant N372H in BRCA2 gene may be associated with idiopathic male infertility with azoospermia or severe oligozoospermia". Eur. J. Obstet. Gynecol. Reprod. Biol. 124 (1): 61–4. doi:10.1016/j.ejogrb.2005.09.001. PMID 16257105.
- ↑ Zhang X, Ding M, Ding X, Li T, Chen H (2015). "Six polymorphisms in genes involved in DNA double-strand break repair and chromosome synapsis: association with male infertility". Syst Biol Reprod Med. 61 (4): 187–93. doi:10.3109/19396368.2015.1027014. PMID 26086992.
- 1 2 3 Esteves SC, Miyaoka R, Agarwal A. An update on the clinical assessment of the infertile male. Clinics (Sao Paulo). [corrected]. 2011;66(4):691–700.
- ↑ Lotti, F.; Maggi, M. (2014). "Ultrasound of the male genital tract in relation to male reproductive health" (PDF). Human Reproduction Update. 21 (1): 56–83. doi:10.1093/humupd/dmu042. ISSN 1355-4786. PMID 25038770. Archived (PDF) from the original on 2021-12-15. Retrieved 2021-10-28.
- ↑ Fertil Steril. 2008;90(5 Suppl):S74-7.
- ↑ Coburn, M., Wheeler, T., and Lipshultz, L.I. Testicular biopsy. Its use and limitations. Urol Clin North Am. 1987; 14: 551–561.
- ↑ Ramasamy R, Lin K, Gosden LV, Rosenwaks Z, Palermo GD, Schlegel PN. High serum FSH levels in men with nonobstructive azoospermia does not affect success of microdissection testicular sperm extraction. Fertil Steril. 2009;92(2):590-3.
- ↑ Toulis, K. A.; Iliadou, P. K.; Venetis, C. A.; Tsametis, C.; Tarlatzis, B. C.; Papadimas, I.; Goulis, D. G. (2010). "Inhibin B and anti-Mullerian hormone as markers of persistent spermatogenesis in men with non-obstructive azoospermia: a meta-analysis of diagnostic accuracy studies". Human Reproduction Update. 16 (6): 713–724. doi:10.1093/humupd/dmq024. PMID 20601364.
- ↑ Drabovich, A. P.; Dimitromanolakis, A.; Saraon, P.; Soosaipillai, A.; Batruch, I.; Mullen, B.; Jarvi, K.; Diamandis, E.P. (2013). "Differential Diagnosis of Azoospermia with Proteomic Biomarkers ECM1 and TEX101 Quantified in Seminal Plasma". Science Translational Medicine. 5 (212): 212ra160. doi:10.1126/scitranslmed.3006260. PMID 24259048. S2CID 13541504.
- ↑ Korbakis, D.; Schiza, C.; Brinc, D.; Soosaipillai, A.; Karakosta, T.D.; Légaré, C.; Sullivan, R.; Mullen, B.; Jarvi, K.; Diamandis, E.P.; Drabovich, A.P. (2017). "Preclinical evaluation of a TEX101 protein ELISA test for the differential diagnosis of male infertility". BMC Medicine. 15 (1): 60. doi:10.1186/s12916-017-0817-5. PMC 5363040. PMID 28330469.
- ↑ "Use of Semen TEX101 to Improve Sperm Retrieval Rates for Men With Non-obstructive Azoospermia". March 8, 2019. Archived from the original on April 13, 2017. Retrieved April 13, 2017 – via clinicaltrials.gov.
- ↑ Schlegel, PN (2004). "Causes of azoospermia and their management". Reproduction, Fertility, and Development. 16 (5): 561–72. doi:10.1071/RD03087. PMID 15367371.
- ↑ Fullerton, G.; Hamilton, M.; Maheshwari, A. (2010). "Should non-mosaic Klinefelter syndrome men be labelled as infertile in 2009?". Human Reproduction. 25 (3): 588–597. doi:10.1093/humrep/dep431. PMID 20085911.
- ↑ Haimov-Kochman, R.; Prus, D.; Farchat, M.; Bdolah, Y.; Hurwitz, A. (2010). "Reproductive outcome of men with azoospermia due to cryptorchidism using assisted techniques". International Journal of Andrology. 33 (1): e139–e143. doi:10.1111/j.1365-2605.2009.00977.x. PMID 19622071.
External links
| -spermia, Further information: Testicular infertility factors |
| Aspermia—lack of semen; anejaculation |
| Asthenozoospermia—sperm motility below lower reference limit |
| Azoospermia—absence of sperm in the ejaculate |
| Hyperspermia—semen volume above upper reference limit |
| Hypospermia—semen volume below lower reference limit |
| Oligospermia—total sperm count below lower reference limit |
| Necrospermia—absence of living sperm in the ejaculate |
| Teratospermia—fraction of normally formed sperm below lower reference limit |
| Classification |
|---|