Torticollis
| Torticollis | |
|---|---|
| Other names: Wry neck, crick in the neck, stiff neck, loxia | |
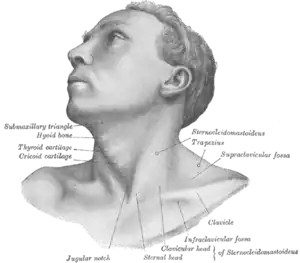 | |
| The muscles involved with torticollis | |
| Specialty | Orthopedics |
| Symptoms | Abnormal twisted position of the neck[1] |
| Usual onset | Any age[2] |
| Types | Variable, fixed[2] |
| Causes | Variable: Minor local injury, spasms of neck muscles, benign paroxysmal torticollis, certain medications, increased intracranial pressure, conversion disorder[3][2] Fixed: Congenital muscular torticollis, bone disorders, eye problems, brain injury, infections, scarring of the overlying skin[2][4] |
| Diagnostic method | By examination[4] |
| Differential diagnosis | Essential tremor, myasthenia gravis, multiple sclerosis, cerebral palsy[4] |
| Treatment | Ibuprofen, paracetamol (acetaminophen), heat, physiotherapy[3] |
| Frequency | 90% at some point[4] |
Torticollis, also known as wry neck, is an abnormal twisted position of the neck.[1] Most commonly the head is rotated to one side and flexed forwards, though other positions may occur.[4] Pain or fever may be present.[4] Depending on the underlying cause the condition may be short term or last years.[3][5]
Causes may be divided into variable and fixed.[2] Causes of the variable type includes minor local injury, spasms of neck muscles, benign paroxysmal torticollis, certain medications, increased intracranial pressure, and conversion disorder.[3][2] Causes of the fixed type include birth defects, including congenital muscular torticollis, bone disorders, eye problems, brain injury, infections, and scarring of the overlying skin.[2][4] Muscle spasms is the most common cause.[4] Diagnosis is generally by examination.[4]
When due to minor injury, often it will resolve after a few days, even without treatment.[3][6] Pain may be treated with ibuprofen or paracetamol (acetaminophen) and heat.[3] Other medications that may be used include benzodiazepines and botox.[4] Physical therapy may also be useful.[4] Certain causes may require surgery.[4][2]
Torticollis is common, with about 90% of people being affected at some point in time.[4] Females are affected more often than males.[4] About 4 in 1,000 are affected at birth, though it may occur at all ages.[4][2] The term torticollis is from the Latin tortus meaning "twisted" and collum meaning "neck".[7]
Signs and symptoms

Torticollis is a fixed or dynamic tilt, rotation, with flexion or extension of the head or neck. The type can be described depending on the positions of the head and neck.[1][8][9]
- laterocollis : the head is tipped toward the shoulder
- rotational torticollis : the head rotates along the longitudinal axis
- anterocollis : forward flexion of the head and neck[10]
- retrocollis : hyperextension of head and neck backward[11]
A combination of these movements may often be observed. Torticollis can be a disorder in itself as well as a symptom in other conditions.
Other symptoms include:[12][13]
- Neck pain
- Occasional formation of a mass
- Thickened or tight sternocleidomastoid muscle
- Tenderness on the cervical spine
- Tremor in head
- Unequal shoulder heights
- Decreased neck movement
Causes
More than 80 different causes have been described.[2] Some types include muscular fibrosis, congenital spine abnormalities, or toxic or traumatic brain injury.[7] It can be categorization into variable (dynamic) and fixed (nondynamic) torticollis.[2]
Variable
- Minor local muscle irritation[3]
- Spasmodic, also known as cervical dystonia[2]
- Drug induced[2] This includes sp,e antiemetics - neuroleptic class - phenothiazines[14]
- Sandifer syndrome is torticollis that occurs as a result of GERD[2]
Spasmodic
Torticollis with recurrent, but transient contraction of the muscles of the neck and especially of the sternocleidomastoid, is called spasmodic torticollis. Synonyms are "intermittent torticollis", "cervical dystonia" or "idiopathic cervical dystonia", depending on cause.
- A self-limiting spontaneously occurring form of torticollis with one or more painful neck muscles is by far the most common ('stiff neck') and will pass spontaneously in 1–4 weeks. Usually the sternocleidomastoid muscle or the trapezius muscle is involved. Sometimes draughts, colds, or unusual postures are implicated; however, in many cases, no clear cause is found. These episodes are commonly seen by physicians.
Fixed
- Bone related[2]
- Non-muscular soft tissue including infectious causes[2]
- Traumatic[2]
- Nervous system[2]
- Eye related include spasmus nutans[2]
- There are many other rare causes of torticollis. A very rare cause of acquired torticollis is fibrodysplasia ossificans progressiva (FOP), the hallmark of which is malformed great toes.
- Tumors of the skull base (posterior fossa tumors) can compress the nerve supply to the neck and cause torticollis, and these problems must be treated surgically.
- Infections in the posterior pharynx can irritate the nerves supplying the neck muscles and cause torticollis, and these infections may be treated with antibiotics if they are not too severe, but could require surgical debridement in intractable cases.
- Ear infections and surgical removal of the adenoids can cause an entity known as Grisel's syndrome, a subluxation of the upper cervical joints, mostly the atlantoaxial joint, due to inflammatory laxity of the ligaments caused by an infection.[15]
Noncongenital muscular torticollis may result from scarring or disease of cervical vertebrae, adenitis, tonsillitis, rheumatism, enlarged cervical glands, retropharyngeal abscess, or cerebellar tumors. It may be spasmodic (clonic) or permanent (tonic). The latter type may be due to Pott's disease (tuberculosis of the spine).
Muscular
Congenital muscular torticollis is the most common type present at birth.[16] The cause is unclear. Birth trauma or intrauterine malposition is considered to result in damage to the sternocleidomastoid muscle in the neck.[7] Other alterations to the muscle tissue arise from repetitive microtrauma within the womb or a sudden change in the calcium concentration in the body which causes a prolonged period of muscle contraction.[17]
Any of these mechanisms can result in a shortening or excessive contraction of the sternocleidomastoid muscle, which curtails its range of motion in both rotation and lateral bending. The head typically is tilted in lateral bending toward the affected muscle and rotated toward the opposite side. In other words, the head itself is tilted in the direction towards the shortened muscle with the chin tilted in the opposite direction.[18]
Congenital torticollis is presented at 1–4 weeks of age, and a hard mass usually develops. It is normally diagnosed using ultrasonography and a colour histogram or clinically through evaluating the infant's passive cervical range of motion.[19]
Congenital torticollis constitutes the majority of cases seen in clinical practice.[18] It is estimated to affect 0.3-2.0%.[20] Sometimes a mass, such as a sternocleidomastoid tumor, is noted in the affected muscle at the age of two to four weeks. Gradually it disappears, usually by the age of eight months, but the muscle is left fibrotic.[7]
Trochlear
Torticollis may be unrelated to the sternocleidomastoid muscle, instead caused by damage to the trochlear nerve (fourth cranial nerve), which supplies the superior oblique muscle of the eye. The superior oblique muscle is involved in depression, abduction, and intorsion of the eye. When the trochlear nerve is damaged, the eye is extorted because the superior oblique is not functioning. The affected person will have vision problems unless they turn their head away from the side that is affected, causing intorsion of the eye and balancing out the extorsion of the eye. This can be diagnosed by the Bielchowsky test, also called the head-tilt test, where the head is turned to the affected side. A positive test occurs when the affected eye elevates, seeming to float up.[21]
Mechanism
The underlying anatomical distortion causing torticollis often involves shortened of the sternocleidomastoid muscle. This is the muscle of the neck that originates at the sternum and clavicle and inserts on the mastoid process of the temporal bone on the same side.[18] There are two sternocleidomastoid muscles in the human body and when they both contract, the neck is flexed. The main blood supply for these muscles come from the occipital artery, superior thyroid artery, transverse scapular artery and transverse cervical artery.[18] The main innervation to these muscles is from cranial nerve XI (the accessory nerve) but the second, third and fourth cervical nerves are also involved.[18] Pathologies in these blood and nerve supplies can lead to torticollis.
Diagnosis
Cases of short duration can usually be diagnosed based on symptoms, without the need for further investigations.[22]
Evaluation of a child with torticollis begins with history taking to determine circumstances surrounding birth and any possibility of trauma or associated symptoms. Physical examination reveals decreased rotation and bending to the side opposite from the affected muscle. Some say that congenital cases more often involve the right side, but there is not complete agreement about this in published studies. Evaluation should include a thorough neurologic examination, and the possibility of associated conditions such as developmental dysplasia of the hip and clubfoot should be examined. Radiographs of the cervical spine should be obtained to rule out obvious bony abnormality, and MRI should be considered if there is concern about structural problems or other conditions.
Ultrasonography can be used to visualize muscle tissue, with a colour histogram generated to determine cross-sectional area and thickness of the muscle.
Evaluation by an eye specialist should be considered in children to ensure that the torticollis is not caused by vision problems (IV cranial nerve palsy, nystagmus-associated "null position," etc.).
Cervical dystonia appearing in adulthood has been believed to be idiopathic in nature, as specific imaging techniques most often find no specific cause.[23]
Differential diagnosis
Conditions that may present similarly include essential tremor, myasthenia gravis, multiple sclerosis, and cerebral palsy.[4]
Treatment
When due to minor injury, often it will resolve after a few days, even without treatment.[3] Pain may be treated with ibuprofen, paracetamol (acetaminophen), and heat.[3] A pillow that is not too high may be useful.[3]
Physical therapy
Initially, the condition is treated with physical therapies, such as stretching to release tightness, strengthening exercises to improve muscular balance, and handling to stimulate symmetry. Early initiation of treatment is very important for full recovery and to decrease chance of relapse.[18]
Physical therapy is an option for treating torticollis in a non-invasive and cost-effective manner.[24] In the children above 1 year of age, surgical release of the tight sternocleidomastoid muscle is indicated along with aggressive therapy and appropriate splinting. Occupational therapy rehabilitation in Congenital muscular torticollis concentrates on observation, orthosis, gentle stretching, myofascial release techniques, parents’ counseling-training, and home exercise program. While outpatient infant physiotherapy is effective, home therapy performed by a parent or guardian is just as effective in reversing the effects of congenital torticollis.[17] It is important for physical therapists to educate parents on the importance of their role in the treatment and to create a home treatment plan together with them for the best results for their child. Five components have been recognized as the "first choice intervention" in PT for treatment of torticollis and include neck passive range of motion, neck and trunk active range of motion, development of symmetrical movement, environmental adaptations, and caregiver education. In therapy, parents or guardians should expect their child to be provided with these important components, explained in detail below.[25] Lateral neck flexion and overall range of motion can be regained quicker in newborns when parents conduct physical therapy exercises several times a day.[17]
Physical therapists should teach parents and guardians to perform the following exercises:[17]
- Stretching the neck and trunk muscles actively. Parents can help promote this stretching at home with infant positioning.[25] For example, prone positioning will encourage the child to lift their chin off the ground, thereby strengthening their bilateral neck and spine extensor muscles, and stretching their neck flexor muscles.[25] Active rotation exercises in supine, sitting or prone position by using toys, lights and sounds to attract infant's attention to turn neck and look toward the non-affected side.[25]
- Stretching the muscle in a prone position passively.[25] Passive stretching is manual, and does not include infant involvement. Two people can be involved in these stretches, one person stabilizing the infant while the other holds the head and slowly brings it through the available range of motion.[25] Passive stretching should not be painful to the child, and should be stopped if the child resists.[25] Also, discontinue the stretch if changes in breathing or circulation are seen or felt.[25]
- Stretching the muscle in a lateral position supported by a pillow (have infant lie on the side with the neck supported by pillow). Affected side should be against the pillow to deviate the neck towards the non-affected side.
- Environmental adaptations can control posture in strollers, car seats and swings (using U-shaped neck pillow or blankets to hold neck in neutral position)
- Passive cervical rotation (much like stretching when being supported by a pillow, have affected side down)
- Position infant in the crib with affected side by the wall so they must turn to the non-affected side to face out
Physical therapists often encourage parents and caregivers of children with torticollis to modify the environment to improve neck movements and position. Modifications may include:
- Adding neck supports to the car seat to attain optimal neck alignment
- Reducing time spent in a single position
- Using toys to encourage the child to look in the direction of limited neck movement
- Alternating sides when bottle or breastfeeding[25]
- Encouraging prone playtime (tummy time). Although the Back to Sleep campaign promotes infants sleeping on their backs to avoid sudden infant death syndrome during sleep, parents should still ensure that their infants spend some waking hours on their stomachs.[25]
Surgery
About 5–10% of cases fail to respond to stretching and require surgical release of the muscle.[26][27]
Surgical release involves the two heads of the sternocleidomastoid muscle being dissected free. This surgery can be minimally invasive and done laparoscopically. Usually surgery is performed on those who are over 12 months old. The surgery is for those who do not respond to physical therapy or botulinum toxin injection or have a very fibrotic sternocleidomastoid muscle.[12] After surgery the child will be required to wear a soft neck collar (also called a Callot's cast). There will be an intense physiotherapy program for 3–4 months as well as strengthening exercises for the neck muscles.[28]
Other
Other treatments include:[17]
Prognosis
Studies and evidence from clinical practice show that 85–90% of cases of congenital torticollis are resolved with conservative treatment such as physical therapy.[25] Earlier intervention is shown to be more effective and faster than later treatments. More than 98% of infants with torticollis treated before 1 month of age recover by 2.5 months of age.[25] Infants between 1 and 6 months usually require about 6 months of treatment.[25] After that point, therapy will take closer to 9 months, and it is less likely that the torticollis will be fully resolved.[25] It is possible that torticollis will resolve spontaneously, but chance of relapse is possible.[18] For this reason, infants should be reassessed by their physical therapist or other provider 3–12 months after their symptoms have resolved.[25]
Terminology
The term "loxia" is also used for a genus of bird species known as "crossbills", which was assigned by Swiss naturalist Conrad Gesner because of the obvious similarities.
Other animals

In veterinary literature usually only the lateral bend of head and neck is termed torticollis, whereas the analogon to the rotatory torticollis in humans is called a head tilt. The most frequently encountered form of torticollis in domestic pets is the head tilt, but occasionally a lateral bend of the head and neck to one side is encountered.
Head tilt
Causes for a head tilt in domestic animals are either diseases of the central or peripheral vestibular system or relieving posture due to neck pain. Known causes for head tilt in domestic animals include:
- Encephalitozoon cuniculi (or E. cuniculi) infection in rabbits[32]
- Inner ear infection[33]
- Hypothyroidism in dogs[34]
- Disease of the VIIIth cranial nerve the N. Vestibulocochlearis through trauma, infection, inflammation or neoplasia
- Disease of the brain stem through either stroke, trauma or neoplasia
- Damage to the vestibular organ due to toxicity, inflammation or impaired blood supply
- Geriatric vestibular syndrome in dogs
References
- 1 2 3 Dauer, W.; Burke, RE; Greene, P; Fahn, S (1998). "Current concepts on the clinical features, aetiology and management of idiopathic cervical dystonia". Brain. 121 (4): 547–60. doi:10.1093/brain/121.4.547. PMID 9577384.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Tomczak, KK; Rosman, NP (March 2013). "Torticollis". Journal of child neurology. 28 (3): 365–78. doi:10.1177/0883073812469294. PMID 23271760.
- 1 2 3 4 5 6 7 8 9 10 "Neck pain - acute torticollis". NICE. September 2018. Archived from the original on 29 August 2021. Retrieved 6 March 2021.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Cunha, B; Tadi, P; Bragg, BN (January 2021). "Torticollis". PMID 30969679.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Dystonias Fact Sheet | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Archived from the original on 23 April 2018. Retrieved 6 March 2021.
- ↑ Bartleson, J. D.; Deen, H. Gordon (2009-07-23). Spine Disorders: Medical and Surgical Management. Cambridge University Press. p. 46. ISBN 9780521889414. Archived from the original on 2021-08-29. Retrieved 2020-11-22.
Many patients for no apparent reason will awaken in the morning with a “wry” neck or a “crick” in the neck. They may have trouble moving the neck and often have acute muscle spasm. Their pain and limited range of motion subside typically in a matter of a few days without or perhaps more quickly with treatment.
- 1 2 3 4 Cooperman, Daniel R. (1997). Karmel-Ross, Karen (ed.). The Differential Diagnosis of Torticollis in Children. Physical & Occupational Therapy in Pediatrics. Vol. 17. pp. 1–11. doi:10.1080/J006v17n02_01. ISBN 978-0-7890-0316-4. Archived from the original on 2021-08-29. Retrieved 2021-03-05.
- ↑ Velickovic, M; Benabou, R; Brin, MF (2001). "Cervical dystonia pathophysiology and treatment options". Drugs. 61 (13): 1921–43. doi:10.2165/00003495-200161130-00004. PMID 11708764. S2CID 46954613.
- ↑ "Cervical dystonia - Symptoms and causes - Mayo Clinic". www.mayoclinic.org. Archived from the original on 2018-12-12. Retrieved 2017-11-02.
- ↑ Papapetropoulos, S; Tuchman, A; Sengun, C; Russell, A; Mitsi, G; Singer, C (2008). "Anterocollis: Clinical features and treatment options". Medical Science Monitor. 14 (9): CR427–30. PMID 18758411.
- ↑ Papapetropoulos, Spiridon; Baez, Sheila; Zitser, Jennifer; Sengun, Cenk; Singer, Carlos (2008). "Retrocollis: Classification, Clinical Phenotype, Treatment Outcomes and Risk Factors". European Neurology. 59 (1–2): 71–5. doi:10.1159/000109265. PMID 17917462. S2CID 30159732.
- 1 2 Saxena, Amulya (2015). "Pediatric torticollis surgery treatment & management". Medscape.
- ↑ "Torticollis: MedlinePlus Medical Encyclopedia". medlineplus.gov. Archived from the original on 2019-04-14. Retrieved 2017-11-02.
- ↑ Dressler, D.; Benecke, R. (2005). "Diagnosis and management of acute movement disorders". Journal of Neurology. 252 (11): 1299–306. doi:10.1007/s00415-005-0006-x. PMID 16208529. S2CID 189867541.
- ↑ Bocciolini, C; Dall’Olio, D; Cunsolo, E; Cavazzuti, PP; Laudadio, P (August 2005). "Grisel's syndrome: a rare complication following adenoidectomy". Acta Otorhinolaryngologica Italica. 25 (4): 245–249. ISSN 0392-100X. PMC 2639892. PMID 16482983.
- ↑ 2013, Boston Childrens Hospital. "Torticollis | Boston Children's Hospital". www.childrenshospital.org. Archived from the original on 2017-09-21. Retrieved 2017-09-21.
{{cite web}}: CS1 maint: numeric names: authors list (link) - 1 2 3 4 5 Carenzio, G (2015). "Early rehabilitation treatment in newborns with congenital muscular torticollis". Phys Rehabil Med. 51 (5): 539–45. PMID 25692687.
- 1 2 3 4 5 6 7 Tomczak, K (2013). "Torticollis". Journal of Child Neurology. 28 (3): 365–378. doi:10.1177/0883073812469294. PMID 23271760. S2CID 216099695.
- ↑ Boricean, ID (2011). "Understanding ocular torticollis in children". Oftalmologia (Bucharest, Romania : 1990). 55 (1): 10–26. PMID 21774381.
- ↑ Cheng, JC; Wong, MW; Tang, SP; Chen, TM; Shum, SL; Wong, EM (2001). "Clinical determinants of the outcome of manual stretching in the treatment of congenital muscular torticollis in infants. A prospective study of eight hundred and twenty-one cases". The Journal of Bone and Joint Surgery. American Volume. 83-A (5): 679–87. doi:10.2106/00004623-200105000-00006. PMID 11379737. S2CID 999791.
- ↑ "Trochlear Nerve Palsy: Background, History of the Procedure, Problem". 2016-08-12. Archived from the original on 2017-03-10. Retrieved 2017-02-04.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Neck pain - acute torticollis: What investigations should I arrange for people with suspected torticollis?". NICE. September 2018. Archived from the original on 29 August 2021. Retrieved 6 March 2021.
- ↑ Crowner, Beth E. (2007-11-01). "Cervical Dystonia: Disease Profile and Clinical Management". Physical Therapy. 87 (11): 1511–1526. doi:10.2522/ptj.20060272. ISSN 0031-9023. PMID 17878433.
- ↑ Kaplan, Sandra L.; Coulter, Colleen; Fetters, Linda (2013). "Physical Therapy Management of Congenital Muscular Torticollis". Pediatric Physical Therapy. 25 (4): 348–394. doi:10.1097/pep.0b013e3182a778d2. PMID 24076627.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Kaplan, Sandra L.; Coulter, Colleen; Sargent, Barbara (October 2018). "Physical Therapy Management of Congenital Muscular Torticollis: A 2018 Evidence-Based Clinical Practice Guideline From the APTA Academy of Pediatric Physical Therapy". Pediatric Physical Therapy. 30 (4): 240–290. doi:10.1097/PEP.0000000000000544. ISSN 0898-5669. PMID 30277962. S2CID 52909510.
- ↑ Tang, SF; Hsu, KH; Wong, AM; Hsu, CC; Chang, CH (2002). "Longitudinal followup study of ultrasonography in congenital muscular torticollis". Clinical Orthopaedics and Related Research. 403 (403): 179–85. doi:10.1097/00003086-200210000-00026. PMID 12360024. S2CID 20606626.
- ↑ Hsu, Tsz-Ching; Wang, Chung-Li; Wong, May-Kuen; Hsu, Kuang-Hung; Tang, Fuk-Tan; Chen, Huan-Tang (1999). "Correlation of clinical and ultrasonographic features in congenital muscular torticollis". Archives of Physical Medicine and Rehabilitation. 80 (6): 637–41. doi:10.1016/S0003-9993(99)90165-X. PMID 10378488.
- ↑ Seung, Seo (2015). "Change of facial asymmetry in patients". Medscape.
- ↑ Samotus, Olivia; Lee, Jack; Jog, Mandar (2018-03-20). "Personalized botulinum toxin type A therapy for cervical dystonia based on kinematic guidance". Journal of Neurology. 265 (6): 1269–1278. doi:10.1007/s00415-018-8819-6. ISSN 1432-1459. PMID 29557988. S2CID 4043479.
- ↑ Safarpour, Yasaman; Jabbari, Bahman (2018-02-24). "Botulinum Toxin Treatment of Movement Disorders". Current Treatment Options in Neurology. 20 (2): 4. doi:10.1007/s11940-018-0488-3. ISSN 1092-8480. PMID 29478149. S2CID 3502413.
- ↑ Kwon, D.R. (2014). "Efficacy of micro current therapy in infants with congenital muscular torticollis involving the entire sternocleidomastoid muscle". Clinical Rehabilitation. 28 (10): 983–91. doi:10.1177/0269215513511341. PMID 24240061. S2CID 206484848.
- ↑ Künzel, Frank; Joachim, Anja (2009). "Encephalitozoonosis in rabbits". Parasitology Research. 106 (2): 299–309. doi:10.1007/s00436-009-1679-3. PMID 19921257. S2CID 11727371.
- ↑ "Head Tilt: Causes and Treatment". rabbit.org. Archived from the original on 26 January 2021. Retrieved 4 March 2021.
- ↑ Jaggy, André; Oliver, John E.; Ferguson, Duncan C.; Mahaffey, E. A.; Glaus Jr, T. Glaus (1994). "Neurological Manifestations of Hypothyroidism: A Retrospective Study of 29 Dogs". Journal of Veterinary Internal Medicine. 8 (5): 328–36. doi:10.1111/j.1939-1676.1994.tb03245.x. PMID 7837108.
External links
| Classification | |
|---|---|
| External resources |