Tenosynovial giant cell tumor
| Tenosynovial giant cell tumor | |
|---|---|
| Other names: Localized: Localized pigmented villonodular synovitis (L-PVNS), Giant cell tumor of the tendon sheath (GCT-TS), Nodular tenosynovitis, Localized nodular tenosynovitis, and L-TGCT Diffuse: Pigmented villonodular synovitis (PVNS), Conventional PVNS, and D-TGCT | |
 | |
| Micrograph of diffuse TGCT, also known as pigmented villonodular synovitis. H&E stain. | |
| Specialty | Rheumatology |
| Symptoms | Swelling, pain, sensitivity, and/or limited range of motion |
| Complications | Spreading of tumors to surrounding tissues |
| Types | Diffuse and localized |
| Diagnostic method | MRI, biopsy, surgery |
| Treatment | Surgery, CSF1R inhibitors |
Tenosynovial giant cell tumor (TGCT) is a group of rare, typically non-malignant tumors of the joints. TGCT tumors often develop from the lining of joints (also known as synovial tissue).[1][2][2]:100[3][3]:245
Common symptoms of TGCT include swelling, pain, stiffness and reduced mobility in the affected joint or limb.[2]:102 This group of tumors can be divided into different subsets according to their site, growth pattern, and prognosis.[4][4]:361 Localized TGCT is sometimes referred to as giant cell tumor of the tendon sheath;[2]:100 diffuse TGCT is also called pigmented villonodular synovitis (PVNS).[2]:102
Classification
Classification for TGCT encompasses two subtypes that can be divided according to site – within a joint (intra-articular) or outside of the joint (extra-articular) – and growth pattern (localized or diffuse) of the tumor(s).[2]:100[4]:361 Localized and diffuse subsets of TGCT differ in their prognosis, clinical presentation, and biological behavior, but share a similar manner of disease development.[2]:100
Localized TGCT
Localized TGCT is sometimes referred to as localized pigmented villonodular synovitis (L-PVNS), giant cell tumor of the tendon sheath (GCT-TS), nodular tenosynovitis, localized nodular tenosynovitis, and L-TGCT.[1]:1[2]:100
The localized form of TGCT is more common.[2]:100[3]:245 Localized TGCT tumors are typically 0.5 cm-4 cm),[2]:101 develop over years,[2]:100 are benign and non-destructive to the surrounding tissue, and may reoccur in the affected area.[2]:101 The most common symptom is painless swelling.[2]:101 Localized TGCT most often occurs in fingers, but can also occur in other joints.[2][5]
Diffuse TGCT
Diffuse TGCT is sometimes referred to as pigmented villonodular synovitis (PVNS), conventional PVNS, and D-TGCT.[1]:1[4]:361[6]:1[2]:102
Diffuse TGCT occurs less frequently and is locally aggressive (in some cases, tumors may infiltrate surrounding soft tissue).[3]:245[1]:1[2]:102[6][6]:1 It most commonly affects people under 40 years old, though the age of occurrence varies.[2]:102 Diffuse TGCT may occur inside a joint (intra-articular) or outside of a joint (extra-articular). Intra-articular tumors typically occur in the knee (approximately 75% of cases) and hip (approximately 15% of cases).[2]:102 Extra-articular tumors are usually found in the knee, thigh, and foot.[2]:101 Symptoms include swelling, pain, sensitivity, and/or limited range of motion.[2]:102 The rate of reoccurrence is estimated to be 18-46% for intra-articular tumors and 33-50% for extra-articular tumors.[2]:103[6]:1
Signs and symptoms
Complications
Diffuse TGCT is locally aggressive and can spread to surrounding tissues, causing bone erosion and tissue damage. If not treated early, it can spread to areas outside the joint, extra-articular, and potentially cause permanent loss of range as well as intense pain.[7][8]
Pathogenesis
TGCT tumors grow due to genetic overexpression of colony stimulating factor 1. This causes colony-stimulating factor-1 receptor (CSF1R) cells to accumulate in the joint tissue.[9][10]
Pathology
Per Nature, malignant Tenosynovial giant cell tumor tend to be "large, fleshy, and poorly circumscribed with areas of hemorrhage and necrosis" , while small histiocytes, larger mononuclear cells, siderophages were the given, histiologically.[11]
 55-year-old female who initially presented with progressive right posterior calf pain now status post right leg amputation for malignant tenosynovial giant cell tumor. Gross pathology of the amputated right lower extremity reveals a heterogeneous tumor with cystic (thick arrow) and solid (thin arrow) components extending from the popliteal fossa to the mid-calf.
55-year-old female who initially presented with progressive right posterior calf pain now status post right leg amputation for malignant tenosynovial giant cell tumor. Gross pathology of the amputated right lower extremity reveals a heterogeneous tumor with cystic (thick arrow) and solid (thin arrow) components extending from the popliteal fossa to the mid-calf.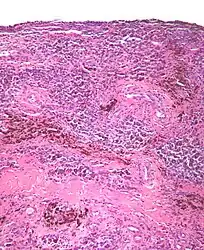 Micrograph of diffuse TGCT showing pigmented hemosiderin-laden macrophages (brown/red).
Micrograph of diffuse TGCT showing pigmented hemosiderin-laden macrophages (brown/red)..jpg.webp) Histopathology of localized TGCT arising in hand finger. H&E stain.
Histopathology of localized TGCT arising in hand finger. H&E stain.
Diagnosis
TGCT can be diagnosed by magnetic resonance imaging (MRI), by biopsy, or during surgery.[12][13] The disorder is difficult to identify and is often not diagnosed for years due to nonspecific symptoms or a general paucity of symptoms.[14] TGCT cases are often misdiagnosed as osteoarthritis,[15] localized trauma,[16] sports injuries,[17][18] xanthomas,[19] or other conditions.[20] One study of 122 diffuse TGCT patients found that the average delay in diagnosis was 2.9 years.[21]
Treatment
Surgery has been the most common form of treatment for both localized[2]:101[4]:361 and diffuse TGCT.[2]:103[4]:361[6]:1 After surgery, patients may receive physical therapy in order to help rehabilitate affected joints.[17][8] However, recurrence of TGCT after surgery is common,[15] with a higher rate of recurrence for diffuse TGCT than for localized TGCT.[4]:361 In cases of recurrent or resistant disease, multiple surgeries, total joint arthroplasties, or amputation may be required.[6]:1
A multidisciplinary approach, supplementing surgery with radiotherapy or other treatments, can also improve outcomes in cases of recurrent TGCT.[22] In the late 2010s, treatment with CSF1R inhibitors emerged as an option[23] that may help improve functionality for patients with recurrent TGCT or TGCT that is not easily managed by surgery.[4]:361
Epidemiology
A study conducted in the Netherlands estimated that the worldwide incidence of TGCT is 43 cases per million person-years. The majority – 39 cases per million person-years – were estimated to be localized TGCT; the remaining 4 cases per million person-years were estimated to be diffuse TGCT.[5] TGCT can occur in patients of any age, but people with localized TGCT are typically between 30 and 50 years old,[2]:100–101 while diffuse TGCT tends to affect people under the age of 40.[2]:102–103
See also
References
- 1 2 3 4 Lucas, David R. (2012). "Tenosynovial Giant Cell Tumor: Case Report and Review". Archives of Pathology & Laboratory Medicine. 136 (8): 901–906. doi:10.5858/arpa.2012-0165-CR. PMID 22849738.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 Fletcher, C. D.M.; Bridge, J.A.; Hogendoorn, P.; Mertens, F. (2013). WHO Classification of Tumours of Soft Tissue and Bone. Fourth Edition. World Health Organization. ISBN 9789283224341. Archived from the original on 2016-07-19. Retrieved 2021-09-22.
- 1 2 3 4 Rateb, Kochbati; Hassen, Ben Ghozlen; Leila, Abid; Faten, Farah; Med Samir, Daghfous (2017). "Giant cell tumor of soft tissues: A case report of extra-articular diffuse-type giant cell tumor of the quadriceps". International Journal of Surgery Case Reports. 31: 245–249. doi:10.1016/j.ijscr.2016.12.019. PMC 5310176. PMID 28199932.
- 1 2 3 4 5 6 7 8 Ravi, Vinod; Wang, Wei-Lien; Lewis, Valerae O. (2011). "Treatment of tenosynovial giant cell tumor and pigmented villonodular synovitis". Current Opinion in Oncology. 23 (4): 361–366. doi:10.1097/CCO.0b013e328347e1e3. PMID 21577109. S2CID 1608847.
- 1 2 Mastboom, Monique J L.; Verspoor, Floortje G M.; Verschoor, Arjan J.; Uittenbogaard, Daniël; Nemeth, Banne; Mastboom, Walter J B.; Bovée, Judith V M G.; Dijkstra, P D Sander; Schreuder, H W Bart; Gelderblom, Hans; Van De Sande, Michiel A J.; TGCT study group (2017). "Higher incidence rates than previously known in tenosynovial giant cell tumors". Acta Orthopaedica. 88 (6): 688–694. doi:10.1080/17453674.2017.1361126. PMC 5694816. PMID 28787222.
- 1 2 3 4 5 6 Mastboom, Monique J. L.; Verspoor, Floortje G. M.; Gelderblom, Hans; Sande, Michiel A. J. van de (2017). "Limb Amputation after Multiple Treatments of Tenosynovial Giant Cell Tumour: Series of 4 Dutch Cases". Case Reports in Orthopedics. 2017: 1–6. doi:10.1155/2017/7402570. PMC 5506462. PMID 28744388.
- ↑ "Clinical Study". The Stone Clinic. Archived from the original (web journal) on 2007-07-01. Retrieved 2007-08-07.
- 1 2 Jabalameli, M; Jamshidi, K; Radi, M; Hadi, H; Bagherifard, A (2014). "Surgical outcomes of 26 patients with pigmented villonodular synovitis (PVNS) of the knee at a mean follow-up of 4 years: Introducing a novel technique". Medical Journal of the Islamic Republic of Iran. 28: 123. PMC 4313448. PMID 25679002.
- ↑ West, R. B.; Rubin, B. P.; Miller, M. A.; Subramanian, S.; Kaygusuz, G.; Montgomery, K.; Zhu, S.; Marinelli, R. J.; De Luca, A.; Downs-Kelly, E.; Goldblum, J. R.; Corless, C. L.; Brown, P. O.; Gilks, C. B.; Nielsen, T. O.; Huntsman, D.; Van De Rijn, M. (2006). "A landscape effect in tenosynovial giant-cell tumor from activation of CSF1 expression by a translocation in a minority of tumor cells". Proceedings of the National Academy of Sciences. 103 (3): 690–695. Bibcode:2006PNAS..103..690W. doi:10.1073/pnas.0507321103. PMC 1325107. PMID 16407111.
The CSF1 translocations result in overexpression of CSF1. In cases of TGCT and PVNS carrying this translocation, it is present in a minority of the intratumoral cells, leading to CSF1 expression only in these cells, whereas the majority of cells express CSF1R but not CSF1, suggesting a tumor-landscaping effect with aberrant CSF1 expression in the neoplastic cells, leading to the abnormal accumulation of nonneoplastic cells that form a tumorous mass.
- ↑ Cupp, John S.; Miller, Melinda A.; Montgomery, Kelli D.; Nielsen, Torsten O.; o??Connell, John X.; Huntsman, David; Rijn, Matt van de; Gilks, Cyril B.; West, Robert B. (2007). "Translocation and Expression of CSF1 in Pigmented Villonodular Synovitis, Tenosynovial Giant Cell Tumor, Rheumatoid Arthritis and Other Reactive Synovitides". The American Journal of Surgical Pathology. 31 (6): 970–976. doi:10.1097/PAS.0b013e31802b86f8. PMID 17527089. S2CID 29544370.
As the CSF1 translocation is postulated to play an important role in the biology of PVNS/TGCT, the consistent presence of CSF1 expression in translocation-negative cases implies that other mechanisms can lead to CSF1 up-regulation.
- ↑ Al-Ibraheemi, Alyaa; Ahrens, William Albert; Fritchie, Karen; Dong, Jie; Oliveira, Andre M.; Balzer, Bonnie; Folpe, Andrew L. (February 2019). "Malignant Tenosynovial Giant Cell Tumor: The True "Synovial Sarcoma?" A Clinicopathologic, Immunohistochemical, and Molecular Cytogenetic Study of 10 Cases, Supporting Origin from Synoviocytes". Modern Pathology. 32 (2): 242–251. doi:10.1038/s41379-018-0129-0. ISSN 1530-0285. Archived from the original on 9 October 2021. Retrieved 5 October 2021.
- ↑ Akinci, Orhan; Akalin, Y.; Incesu, M.; Eren, A. (2011). "Long-term results of surgical treatment of pigmented villonodular synovitis of the knee". Acta Orthopaedica et Traumatologica Turcica. 45 (3): 149–155. doi:10.3944/AOTT.2011.2442. PMID 21765227.
- ↑ Verspoor, Floortje G. M.; Zee, Aniek A. G.; Hannink, Gerjon; Van Der Geest, Ingrid C. M.; Veth, Rene P. H.; Schreuder, H. W. Bart (2014). "Long-term follow-up results of primary and recurrent pigmented villonodular synovitis". Rheumatology. 53 (11): 2063–2070. doi:10.1093/rheumatology/keu230. PMID 24917565.
- ↑ Frassica FJ, Bhimani MA, McCarthy EF, Wenz J (October 1999). "Pigmented villonodular synovitis of the hip and knee". Am Fam Physician. 60 (5): 1404–10, discussion 1415. PMID 10524485. Archived from the original on 2011-06-06. Retrieved 2021-09-22.
- 1 2 Lei, Pengfei; Sun, Rongxin; Liu, Hao; Zhu, Jianxi; Wen, Ting; Hu, Yihe (2017). "Prognosis of Advanced Tenosynovial Giant Cell Tumor of the Knee Diagnosed During Total Knee Arthroplasty". The Journal of Arthroplasty. 32 (6): 1850–1855. doi:10.1016/j.arth.2016.12.053. PMID 28161138.
- ↑ Illian, Christian; Kortmann, Horst-Rainer; Künstler, Hans Otto; Poll, Ludger W.; Schofer, Markus (2009). "Tenosynovial giant cell tumors as accidental findings after episodes of distortion of the ankle: Two case reports". Journal of Medical Case Reports. 3: 9331. doi:10.1186/1752-1947-3-9331. PMC 2803852. PMID 20062758.
- 1 2 Hegedus, Eric J.; Theresa, Kristen (2008). "Postoperative Management of Pigmented Villonodular Synovitis in a Single Subject". Journal of Orthopaedic & Sports Physical Therapy. 38 (12): 790–797. doi:10.2519/jospt.2008.2934. PMID 19047769.
- ↑ Krych, Aaron; Odland, Andrew; Rose, Peter; Dahm, Diane; Levy, Bruce; Wenger, Doris; Stuart, Michael; Sim, Franklin (2014). "Oncologic Conditions That Simulate Common Sports Injuries". Journal of the American Academy of Orthopaedic Surgeons. 22 (4): 223–234. doi:10.5435/JAAOS-22-04-223. PMID 24668352. S2CID 37108679.
- ↑ Adams, E. L.; Yoder, E. M.; Kasdan, M. L. (2012). "Giant cell tumor of the tendon sheath: Experience with 65 cases". ePlasty. 12: e50. PMC 3499005. PMID 23185646.
- ↑ Lee, Yoo Jin; Kang, Youngjin; Jung, Jiyoon; Kim, Seojin; Kim, Chul Hwan (2016). "Intramuscular Tenosynovial Giant Cell Tumor, Diffuse-Type". Journal of Pathology and Translational Medicine. 50 (4): 306–308. doi:10.4132/jptm.2015.11.15. PMC 4963964. PMID 26755356.
- ↑ Ottaviani, Sébastien; Ayral, Xavier; Dougados, Maxime; Gossec, Laure (2011). "Pigmented Villonodular Synovitis: A Retrospective Single-Center Study of 122 Cases and Review of the Literature". Seminars in Arthritis and Rheumatism. 40 (6): 539–546. doi:10.1016/j.semarthrit.2010.07.005. PMID 20884045.
- ↑ Van Der Heijden, L.; Gibbons, C. L. M. H.; Dijkstra, P. D. S.; Kroep, J. R.; Van Rijswijk, C. S. P.; Nout, R. A.; Bradley, K. M.; Athanasou, N. A.; Hogendoorn, P. C. W.; Van De Sande, M. A. J. (2012). "The management of diffuse-type giant cell tumour (Pigmented villonodular synovitis) and giant cell tumour of tendon sheath (Nodular tenosynovitis)". The Journal of Bone and Joint Surgery. British Volume. 94-B (7): 882–888. doi:10.1302/0301-620X.94B7.28927. PMID 22733940.
- ↑ Cannarile, Michael A.; Weisser, Martin; Jacob, Wolfgang; Jegg, Anna-Maria; Ries, Carola H.; Rüttinger, Dominik (2017). "Colony-stimulating factor 1 receptor (CSF1R) inhibitors in cancer therapy". Journal for Immunotherapy of Cancer. 5 (1): 53. doi:10.1186/s40425-017-0257-y. PMC 5514481. PMID 28716061.
The tumor-permissive and immunosuppressive characteristics of tumor-associated macrophages (TAM) have fueled interest in therapeutically targeting these cells. In this context, the colony-stimulating factor 1 (CSF1)/colony-stimulating factor 1 receptor (CSF1R) axis has gained the most attention, and various approaches targeting either the ligands or the receptor are currently in clinical development.
External links
| Classification | |
|---|---|
| External resources |