Transvenous pacing
| Transvenous pacing | |
|---|---|
| Other names: Transvenous heart pacing, transvenous cardiac pacing, endocardial pacing | |
 | |
| Pacer wire setup | |
| Specialty | Emergency medicine, cardiology |
| Indications | Symptomatic slow heart rate[1] |
| Contraindications | None absolute[2] |
| Steps | 1) Place a sheath introducer in the right IJ 2) Check the device balloon 3) Attach sleeve to the hub of the introducer 4) Insert device about 20 cm through the hub 5) Connect to the energy generator 6) Set the generator at 80 BPM and 20 mA 7) Inflate the balloon and advance into the right ventricle (wide QRS complex is seen) 8) Adjust the generator to lowest effective mA 9) Deflate the balloon, secure the sleeve and sheath[3][2] |
| Success | Pulse rate same as set on generator[3] |
| Complications | Heart dysrhythmias, pneumothorax[4] |
Transvenous pacing is a procedure used to correct a slow heart rate that is resulting in significant symptoms.[1] It may be used in cases that do not respond to atropine.[2] Often this rhythm is a complete heart block.[2] Other options include epinephrine or dopamine and transcutaneous pacing.[2]
The procedure is done with the person on their back with the head of the bed down.[1] A sheath introducer is than placed in the right internal jugular.[4] Connect the sleeve to the hub of the introducer.[4] Pass the device about 20 cm through the introducer and inflate the balloon.[3] Set the energy source to 80 BPM and the output at 20 mA, with sensitivity on full.[2] Advance the device until capture is obtained and deflate the balloon.[4] Extend and secure the sleeve so it covers the device.[4]
Verify both electrical capture and a pulse of 80 BPM.[4] Usually the device needs to be placed at a depth of 35 to 40 cm.[1] Decrease mA output until capture is lost than double the output to capture again.[1] A chest X-ray is than done to verify placement and rule out some complications.[1] Complications may include heart dysrhythmias and those of placing a central venous catheter, such as pneumothorax.[4]
Medical uses
Transvenous pacing is used to correct a slow heart rate that is resulting in significant symptoms.[1] It may be used in cases that do not respond to atropine.[2] Often this rhythm is a complete heart block.[2] Other options include epinephrine or dopamine and transcutaneous pacing.[2] The benefit over transcutaneous pacing is that once set up it is less painful.[2]
Contraindications
There are no absolute contraindications, though those with mild symptoms, an artificial tricuspid valve, are digoxin toxic, and who have just had a STEMI and received blood thinners are relatively contraindicated.[2]
Technique
Positioning
The procedure is done with the person on their back with the head of the bed down.[1] The procedure may be done at the bedside using local anesthetic or in conjunction with procedural sedation. At least one assistant is required.[1]
Steps
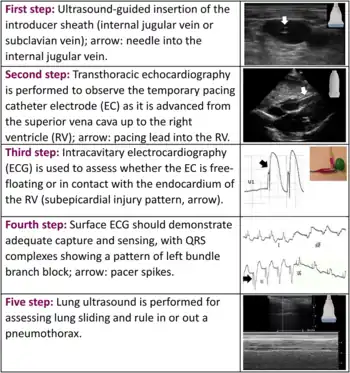
- The first step is placing a sheath introducer.[1] Usually this is a 6 Fr and most catheter electrodes are 5 Fr.[2] This is generally done in the right internal jugular vein.[3]
- To check the balloon on the device, inflate with 1.5 ml of air and than deflate.[3]
- A sterile sleeve is attached to the hub of the sheath.[3]
- Insert the device about 20 cm (to the 2 black lines) through the hub and sleeve with the coil of the tip to the persons left.[3]
- Connect the device to the energy generator and turn the generator on.[3] The positive electrode goes into the positive connector terminal and the negative electrode goes in the negative connector terminal.[2]
- Set the generator to 80 BPM and the output to 20 mA.[3][2] The sensitivity should be set to asynchronous / lowest sensitivity number.[2]
- Inflate the balloon and advance the pacer into the right ventricle.[3] This will appear as pacer spikes and a wide QRS complex on the monitor.[3]
- Adjust the generator output to the lowest effective mA.[3] Decrease the rate to 60 BPM.[2] Sensitivity can also be increased.[2]
- Deflate the balloon and secure the sleeve and sheath into place.[3]
The pacing device may also be advanced through the vein under electrocardiography (ECG) or ultrasound guidance.[1][3] Before pulling back the device make sure the balloon is deflated.[2]
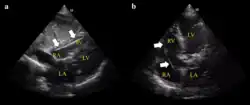 Ultrasound showing the device in the right ventricle
Ultrasound showing the device in the right ventricle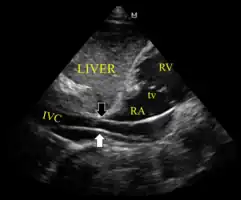 The device inappropriately passing into the inferior vena cava
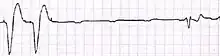
The device inappropriately passing into the inferior vena cava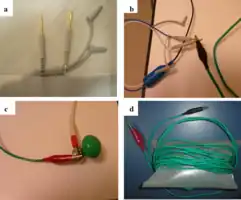 Setup for doing an ECG off the device
Setup for doing an ECG off the device Example of ECG off the device a) free floating in the RV b) in contact with the RV wall
Example of ECG off the device a) free floating in the RV b) in contact with the RV wall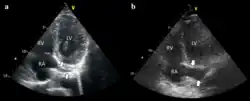 It is possible to place the lead in the coronary sinus, normal (left) dilated (right). Such placement is okay.
It is possible to place the lead in the coronary sinus, normal (left) dilated (right). Such placement is okay.
Troubleshooting
- Failure to pace
This results in the pacemaker not producing an impulse when it should.[2] Solutions may involve checking the batteries, or the connection to the energy generator.[2] The device may be set to asynchronous with a maximum mA to rule out other cause.[2]
- Undersensing
This results in the pacemaker not inhibiting itself when a normal heartbeat occurs.[2] The concern is a risk of R on T.[2] The solution is to turn down the sensitivity, making the pacemaker more sensitive.[2]
- Oversensing
This results in the pacemaker thinking a beat has naturally occurred from the heart and thus a failure to deliver an impulse.[2] The solution is often to turn up the senility to make the pacemaker less sensitive or switching it to asynchronous.[2]
- Failure to capture
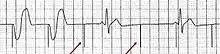
This results in a pacemaker spike without a QRS complex.[2] The solution is often to turn up the current (mA).[2] Other measures include checking for electrolyte abnormalities, rolling the person a different position, and repositioning the device.[2]
Post-procedure

An x-ray after the procedure is obtained to confirm placement of the pacing electrode and rule out complications like pneumothorax.[2][4] Defibrillation and cardioversion can still be carried out in someone with a temporary pacemaker.[2]
Complications
Complications include heart dysrhythmias and those of placing a central venous catheter such as pneumothorax.[4]
References
- 1 2 3 4 5 6 7 8 9 10 11 "Temporary Transvenous Cardiac Pacing • LITFL • CCC". Life in the Fast Lane • LITFL. 30 January 2019. Archived from the original on 23 January 2021. Retrieved 19 March 2021.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 "Identifying Complete Heart Block and the use of Temporary Cardiac Pacing in the Emergency Department". emDOCs.net - Emergency Medicine Education. 22 March 2016. Archived from the original on 26 January 2021. Retrieved 19 March 2021.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 "Transvenous Pacemaker". EM:RAP. Archived from the original on 28 October 2020. Retrieved 19 March 2021.
- 1 2 3 4 5 6 7 8 9 Roberts and Hedges' clinical procedures in emergency medicine and acute care (Seventh ed.). Philadelphia, PA: Elsevier Health Sciences. 2019. pp. 288–303. ISBN 9780323547949.
- ↑ Blanco, P (4 April 2019). "Temporary transvenous pacing guided by the combined use of ultrasound and intracavitary electrocardiography: a feasible and safe technique". The ultrasound journal. 11 (1): 8. doi:10.1186/s13089-019-0122-y. PMID 31359249.